Korean J Neurotrauma.
2016 Oct;12(2):72-76. 10.13004/kjnt.2016.12.2.72.
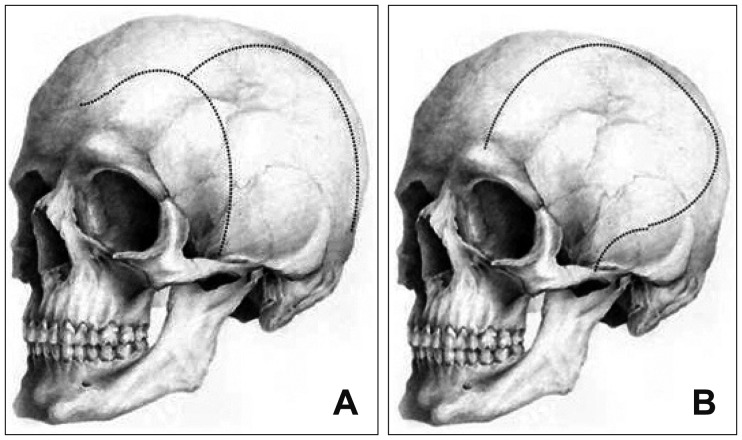
A Faster and Wider Skin Incision Technique for Decompressive Craniectomy: n-Shaped Incision for Decompressive Craniectomy
- Affiliations
-
- 1Department of Neurosurgery, Inha University School of Medicine, Incheon, Korea. dkhyun@inha.com
- 2Department of Neurosurgery, Guro Cham Teun Teun Hospital, Seoul, Korea. dhckdgus@naver.com
- KMID: 2356776
- DOI: http://doi.org/10.13004/kjnt.2016.12.2.72
Abstract
OBJECTIVE
Decompressive craniectomy (DC) is a useful surgical method to achieve adequate decompression in hypertensive intracranial patients. This study suggested a new skin incision for DC, and analyzed its efficacy and safety.
METHODS
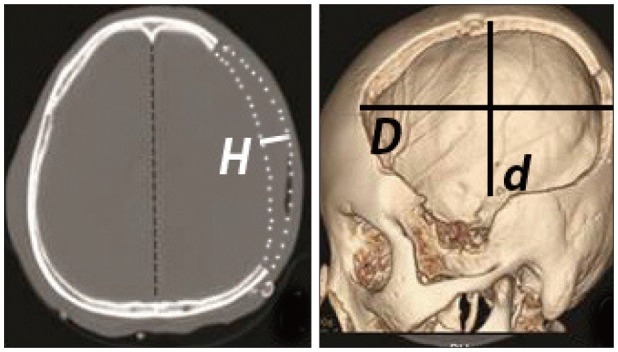
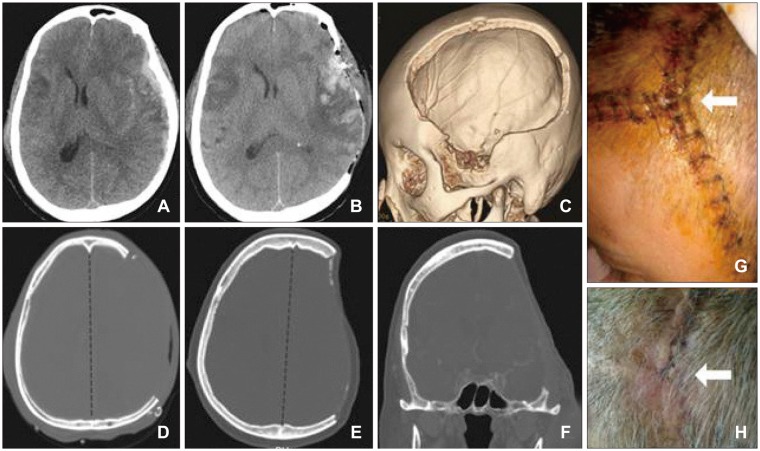
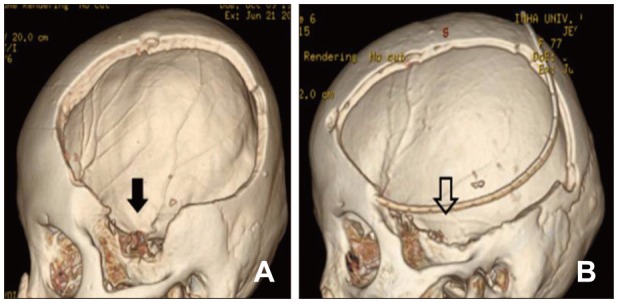
In the retrograde reviews, 15 patients underwent a newly suggested surgical approach using n-shape skin incision technique (Group A) and 23 patients were treated with conventional question mark skin incision technique (Group B). Two groups were compared in the terms of the decompressed area of the craniectomy, protruded brain volume out of the skull layer, the operation time from skin incision to bone flap removal, and modified Rankin Scale (mRS) which was evaluated for 3 months after surgery.
RESULTS
The decompressed area of craniectomy (389.1 cm² vs. 318.7 cm², p=0.041) and the protruded brain volume (151.8 cm³ vs. 116.2 cm³, p=0.045) were significantly larger in Group A compared to the area and the volume in Group B. The time interval between skin incision and bone flap removal was much shorter in Group A (23.3 minutes vs. 29.5 minutes, p=0.013). But, the clinical results were similar between 2 groups. Group A showed more favorable outcome proportion (mRS 0-3, 6/15 patients vs. 5/23 patients, p=0.225) and lesser mortality cases proportion 1/15 patients vs. 4/23 patients, but these differences were not significantly observed (p=0.225 and 0.339).
CONCLUSION
DC using n-shaped skin incision was a feasible and safe surgical technique. It may be an easier and faster method for the purpose of training neurosurgeons.
Keyword
MeSH Terms
Figure
Reference
-
1. Balan C, Alliez B. Decompressive craniectomy: from option to standard - Part I. Rom Neurosurg. 2009; 16:20–26.2. Cho DY, Chen TC, Lee HC. Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction. Surg Neurol. 2003; 60:227–232. PMID: 12922040.
Article3. Chung J, Bang OY, Lim YC, Park SK, Shin YS. Newly suggested surgical method of decompressive craniectomy for patients with middle cerebral artery infarction. Neurologist. 2011; 17:11–15. PMID: 21192185.
Article4. Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg. 2000; 92:1–6.5. Lanzino DJ, Lanzino G. Decompressive craniectomy for space-occupying supratentorial infarction: rationale, indications, and outcome. Neurosurg Focus. 2000; 8:e3.
Article6. Miller JD, Becker DP, Ward JD, Sullivan HG, Adams WE, Rosner MJ. Significance of intracranial hypertension in severe head injury. J Neurosurg. 1977; 47:503–516. PMID: 903804.
Article7. Oh CH, Shim YS, Yoon SH, Hyun D, Park H, Kim E. A Single Center Retrospective Review of 10 Years. Korean J Neurotrauma. 2016; 12:11–17. PMID: 27182496.8. Rahmanian A, Seifzadeh B, Razmkon A, Petramfar P, Kivelev J, Alibai EA, et al. Outcome of decompressive craniectomy in comparison to nonsurgical treatment in patients with malignant MCA infarction. Springerplus. 2014; 3:115. PMID: 24711983.
Article9. Timofeev I, Czosnyka M, Nortje J, Smielewski P, Kirkpatrick P, Gupta A, et al. Effect of decompressive craniectomy on intracranial pressure and cerebrospinal compensation following traumatic brain injury. J Neurosurg. 2008; 108:66–73. PMID: 18173312.
Article10. Wen L, Wang H, Wang F, Gong JB, Li G, Huang X, et al. A prospective study of early versus late craniectomy after traumatic brain injury. Brain Inj. 2011; 25:1318–1324. PMID: 21902550.
Article11. Zacko JC, Harris L, Bullock R. Surgical management of traumatic brain injury. In : Winn HR, editor. Youmans neurological surgery. ed 6. Philadelphia, PA: W. B. Saunders;2011. p. 3424–3452.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Paradoxical Herniation after Decompressive Craniectomy for Acute Subdural Hematoma
- Decompressive Craniectomy in Traumatic Brain Injury: A Review Article
- Paradoxical Transtentorial Herniation Caused by Lumbar Puncture after Decompressive Craniectomy
- "Syndrome of the Sinking Skin-Flap" Secondary to the Ventriculoperitoneal Shunt after Craniectomy
- Clinical Significance of Bifrontotemporal Decompressive Craniectomy in the Treatment of Severe Refractory Posttraumatic Brain Swelling