Ann Rehabil Med.
2016 Aug;40(4):568-574. 10.5535/arm.2016.40.4.568.
Validation of Attitude and Heading Reference System and Microsoft Kinect for Continuous Measurement of Cervical Range of Motion Compared to the Optical Motion Capture System
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. KeewonKimM.D@gmail.com
- 2Interdisciplinary Program of Bioengineering, Graduate School, Seoul National University, Seoul, Korea.
- 3School of Computer Science and Engineering, Seoul National University, Seoul, Korea.
- KMID: 2356641
- DOI: http://doi.org/10.5535/arm.2016.40.4.568
Abstract
OBJECTIVE
To compare optical motion capture system (MoCap), attitude and heading reference system (AHRS) sensor, and Microsoft Kinect for the continuous measurement of cervical range of motion (ROM).
METHODS
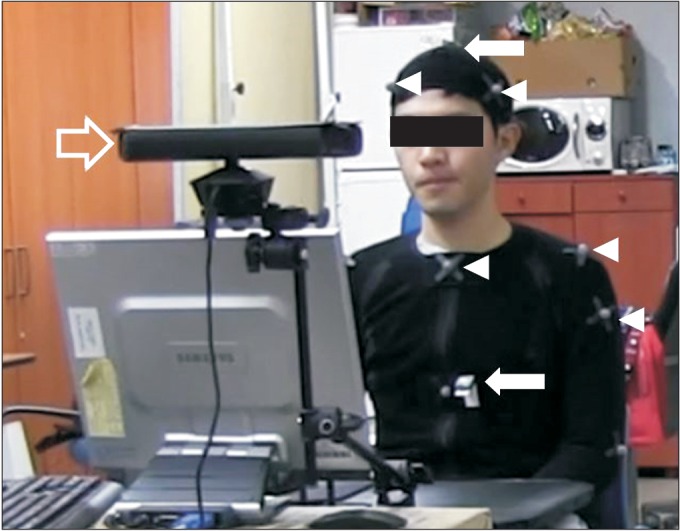
Fifteen healthy adult subjects were asked to sit in front of the Kinect camera with optical markers and AHRS sensors attached to the body in a room equipped with optical motion capture camera. Subjects were instructed to independently perform axial rotation followed by flexion/extension and lateral bending. Each movement was repeated 5 times while being measured simultaneously with 3 devices. Using the MoCap system as the gold standard, the validity of AHRS and Kinect for measurement of cervical ROM was assessed by calculating correlation coefficient and Bland-Altman plot with 95% limits of agreement (LoA).
RESULTS
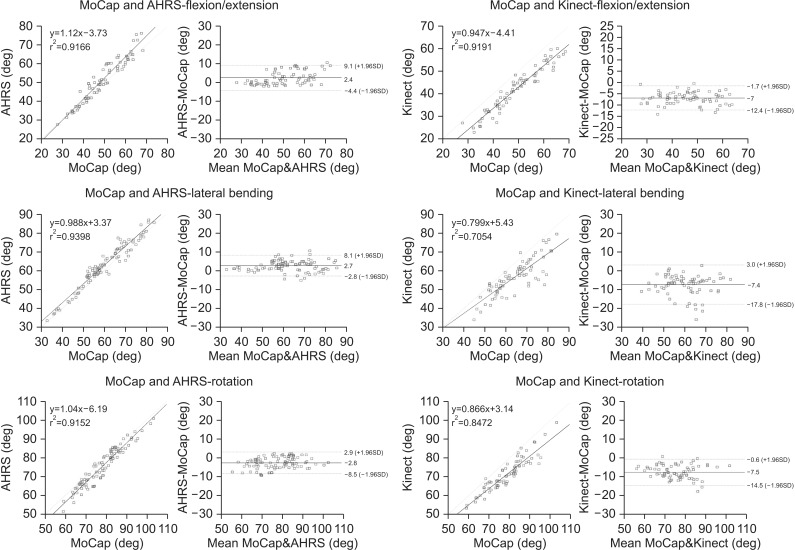
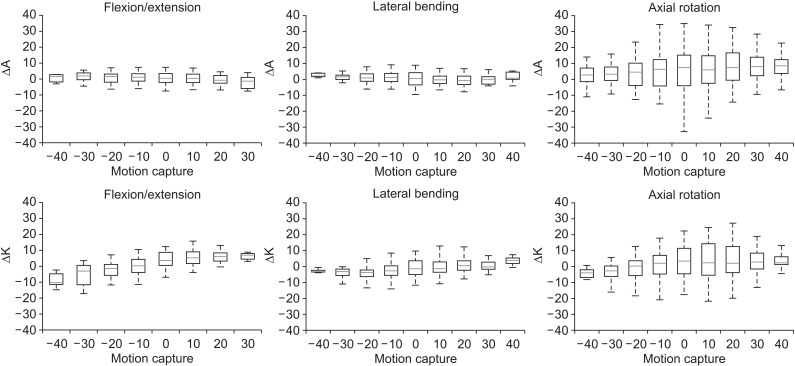
MoCap and ARHS showed fair agreement (95% LoA<10°), while MoCap and Kinect showed less favorable agreement (95% LoA>10°) for measuring ROM in all directions. Intraclass correlation coefficient (ICC) values between MoCap and AHRS in -40° to 40° range were excellent for flexion/extension and lateral bending (ICC>0.9). ICC values were also fair for axial rotation (ICC>0.8). ICC values between MoCap and Kinect system in -40° to 40° range were fair for all motions.
CONCLUSION
Our study showed feasibility of using AHRS to measure cervical ROM during continuous motion with an acceptable range of error. AHRS and Kinect system can also be used for continuous monitoring of flexion/extension and lateral bending in ordinary range.
Keyword
Figure
Reference
-
1. Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion: comparison of three methods. Phys Ther. 1991; 71:98–104. PMID: 1989013.2. Cano SJ, Hobart JC, Fitzpatrick R, Bhatia K, Thompson AJ, Warner TT. Patient-based outcomes of cervical dystonia: a review of rating scales. Mov Disord. 2004; 19:1054–1059. PMID: 15372595.
Article3. Jost WH, Hefter H, Stenner A, Reichel G. Rating scales for cervical dystonia: a critical evaluation of tools for outcome assessment of botulinum toxin therapy. J Neural Transm (Vienna). 2013; 120:487–496. PMID: 22899277.
Article4. Mularski S, Picht T, Kuehn B, Kombos T, Brock M, Suess O. Real-time tracking of vertebral body movement with implantable reference microsensors. Comput Aided Surg. 2006; 11:137–146. PMID: 16829507.
Article5. Bifulco P, Cesarelli M, Romano M, Fratini A, Sansone M. Measurement of intervertebral cervical motion by means of dynamic x-ray image processing and data interpolation. Int J Biomed Imaging. 2013; 2013:152920. PMID: 24288523.
Article6. Haque MA, Anderst W, Tashman S, Marai GE. Hierarchical model-based tracking of cervical vertebrae from dynamic biplane radiographs. Med Eng Phys. 2013; 35:994–1004. PMID: 23122602.
Article7. Anderst WJ, Baillargeon E, Donaldson WF 3rd, Lee JY, Kang JD. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine (Phila Pa 1976). 2011; 36:E393–E400. PMID: 21372650.
Article8. Shotton J, Sharp T, Kipman A, Fitzgibbon A, Finocchio M, Blake A, et al. Real-time human pose recognition in parts from single depth images. Commun ACM. 2013; 56:116–124.
Article9. Schmitz A, Ye M, Shapiro R, Yang R, Noehren B. Accuracy and repeatability of joint angles measured using a single camera markerless motion capture system. J Biomech. 2014; 47:587–591. PMID: 24315287.
Article10. Khoshelham K, Elberink SO. Accuracy and resolution of Kinect depth data for indoor mapping applications. Sensors (Basel). 2012; 12:1437–1454. PMID: 22438718.
Article11. Zhang Z. Microsoft kinect sensor and its effect. IEEE Multimed. 2012; 19:4–10.
Article12. Fernández-Baena A, Susin A, Lligadas X. Biomechanical validation of upper-body and lower-body joint movements of kinect motion capture data for rehabilitation treatments. Proceedings of 2012 4th International Conference on Intelligent Networking and Collaborative Systems (INCoS). 2012 Sep 19-21; Bucharest, Romania. p. 656–661.13. Oikonomidis I, Kyriazis N, Argyros AA. Efficient model-based 3D tracking of hand articulations using Kinect. Proceedings of the British Machine Vision Conference (BMVC). In : ; 2011 Aug 29-Sep 2; Dundee, UK. p. 1–11.14. Chang YJ, Chen SF, Huang JD. A Kinect-based system for physical rehabilitation: a pilot study for young adults with motor disabilities. Res Dev Disabil. 2011; 32:2566–2570. PMID: 21784612.
Article15. Wendel J, Meister O, Schlaile C, Trommer GF. An integrated GPS/MEMS-IMU navigation system for an autonomous helicopter. Aerosp Sci Technol. 2006; 10:527–533.
Article16. Armstrong B, Wolbrecht E, Edwards DB. AUV navigation in the presence of a magnetic disturbance with an extended Kalman filter. Proceedings of the OCEANS 2010 IEEE. 2010 May 24-27; Sydney, Australia. p. 1–6.17. Kim H, Shin SH, Kim JK, Park YJ, Oh HS, Park YB. Cervical coupling motion characteristics in healthy people using a wireless inertial measurement unit. Evid Based Complement Alternat Med. 2013; 2013:570428. PMID: 23935668.
Article18. Windolf M, Gotzen N, Morlock M. Systematic accuracy and precision analysis of video motion capturing systems: exemplified on the Vicon-460 system. J Biomech. 2008; 41:2776–2780. PMID: 18672241.19. Henmi S, Yonenobu K, Masatomi T, Oda K. A biomechanical study of activities of daily living using neck and upper limbs with an optical three-dimensional motion analysis system. Mod Rheumatol. 2006; 16:289–293. PMID: 17039309.
Article20. Lexell JE, Downham DY. How to assess the reliability of measurements in rehabilitation. Am J Phys Med Rehabil. 2005; 84:719–723. PMID: 16141752.
Article21. Lebel K, Boissy P, Hamel M, Duval C. Inertial measures of motion for clinical biomechanics: comparative assessment of accuracy under controlled conditions - effect of velocity. PLoS One. 2013; 8:e79945. PMID: 24260324.
Article22. Lebel K, Boissy P, Hamel M, Duval C. Inertial measures of motion for clinical biomechanics: comparative assessment of accuracy under controlled conditions - changes in accuracy over time. PLoS One. 2015; 10:e0118361. PMID: 25811838.
Article23. Yadav N, Bleakley C. Accurate orientation estimation using AHRS under conditions of magnetic distortion. Sensors (Basel). 2014; 14:20008–20024. PMID: 25347584.
Article24. Luinge HJ, Veltink PH. Inclination measurement of human movement using a 3-D accelerometer with autocalibration. IEEE Trans Neural Syst Rehabil Eng. 2004; 12:112–121. PMID: 15068194.
Article25. Ishii T, Mukai Y, Hosono N, Sakaura H, Nakajima Y, Sato Y, et al. Kinematics of the upper cervical spine in rotation: in vivo three-dimensional analysis. Spine (Phila Pa 1976). 2004; 29:E139–E144. PMID: 15087810.26. Zhao X, Wu ZX, Han BJ, Yan YB, Zhang Y, Lei W. Three-dimensional analysis of cervical spine segmental motion in rotation. Arch Med Sci. 2013; 9:515–520. PMID: 23847675.
Article27. Anderst W, Baillargeon E, Donaldson W, Lee J, Kang J. Motion path of the instant center of rotation in the cervical spine during in vivo dynamic flexion-extension: implications for artificial disc design and evaluation of motion quality after arthrodesis. Spine (Phila Pa 1976). 2013; 38:E594–E601. PMID: 23429677.28. Sforza C, Grassi G, Fragnito N, Turci M, Ferrario V. Three-dimensional analysis of active head and cervical spine range of motion: effect of age in healthy male subjects. Clin Biomech (Bristol, Avon). 2002; 17:611–614.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of foot pitch angle estimation using inertial measurement unit against marker-based optical 3D motion capture system
- Measurement of the Shoulder Motion Using 3-D Motion Capture Technique
- Cervical Range of Motion in Korean Adults
- Automation of Workplace Lifting Hazard Assessment for Musculoskeletal Injury Prevention
- Range of Motion of Cervical Spine in Normal Korean People