Ewha Med J.
2016 Oct;39(4):118-121. 10.12771/emj.2016.39.4.118.
A Patient with IgA Nephropathy: 5 Years after Complete Remission of Minimal Change Nephrotic Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. wondoful1958@paik.ac.kr
- KMID: 2356383
- DOI: http://doi.org/10.12771/emj.2016.39.4.118
Abstract
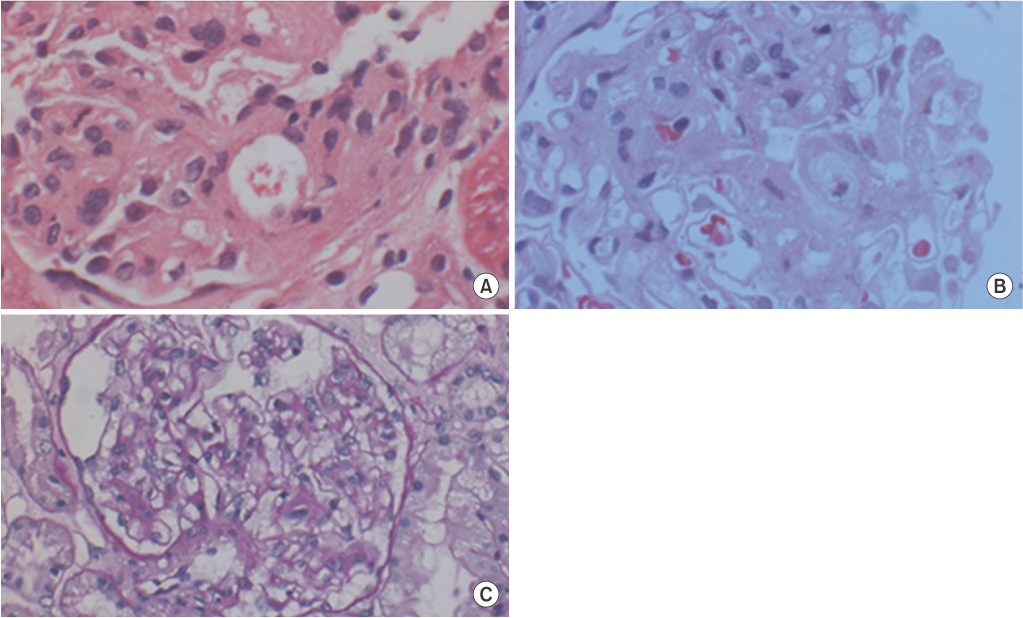
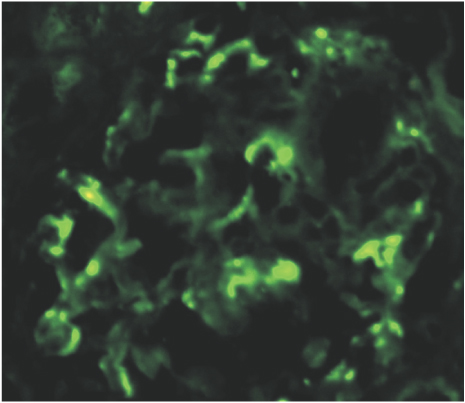
- A 37-year-old male patient was admitted with generalized edema as the main symptom. A blood test confirmed hypoalbuminemia and hyperlipidemia, and a urine test confirmed severe albuminuria. A renal biopsy was conducted, which revealed a diagnosis of minimal change disease. Although the patient experienced complete remission of minimal change nephrotic syndrome after oral prednisolone and cyclophosphamide treatment, he is readmitted due to bilateral leg edema 5 years later since minimal change nephrotic syndrome was completely cured. The patient is diagnosed with IgA nephropathy. Although the exact mechanisms of IgA nephropathy in this patient remain unclear, this case represents an extremely rare development, and is separate from the remission of minimal change nephrotic syndrome.
MeSH Terms
Figure
Reference
-
1. Kikuchi M, Yumura W, Sugino N. Definition and classification of nephrotic syndrome. Nihon Rinsho. 1984; 42:1346–1351.2. Sung JH, Hwang EA, Jin KB, Kwak JH, Han SY, Park SB, et al. Clinical pathologic study on adults idiophathic nephritic syndrome in Korea. Korean J Nephrol. 2007; 26:61–69.3. Nolasco F, Cameron JS, Heywood EF, Hicks J, Ogg C, Williams DG. Adult-onset minimal change nephrotic syndrome: a longterm follow-up. Kidney Int. 1986; 29:1215–1223.4. Shin YT, Oh SM, Na KR, Kim JH, Hwang PJ, Kim JS, et al. Clinical characteristics of minimal change nephrotic syndrome in adults. Korean J Nephrol. 1998; 17:46–52.5. Fujimoto S, Yamamoto Y, Hisanaga S, Morita S, Eto T, Tanaka K. Minimal change nephrotic syndrome in adults: response to corticosteroid therapy and frequency of relapse. Am J Kidney Dis. 1991; 17:687–692.6. Chang KJ, Park SB, Kim HC. Long-term follow-up of adultonset minimal change nephrotic syndrome. Korean J Nephrol. 2003; 22:185–194.7. Kida H, Iida H, Dohi K, Nakamoto Y, Mizumura Y, Takeuchi J. Period of freedom from relapse as an indication of cure in minimal change nephrotic syndrome in adults. Nephron. 1977; 19:153–157.8. Kim YS, Suh WK, Lee TW, Ihm CG, Kim MJ. Clinical characteristics and therapeutic response of adult-onset minimal change disease. Korean J Nephrol. 1987; 6:276–282.9. Shin DH, Kim JH, Kim JY, Noh YJ, Moon SY, Kim JG, et al. A case of adult-onset minimal change nephrotic syndrome relapsed after 15-year of complete remission. Korean J Nephrol. 2003; 22:608–611.10. Cho MH, Hong EH, Lee TH, Ko CW. Pathophysiology of minimal change nephrotic syndrome and focal segmental glomerulosclerosis. Nephrology (Carlton). 2007; 12:Suppl 3. S11–S14.11. Barratt J, Feehally J. IgA nephropathy. J Am Soc Nephrol. 2005; 16:2088–2097.12. Donadio JV, Grande JP. IgA nephropathy. N Engl J Med. 2002; 347:738–748.13. Oberweis BS, Mattoo A, Wu M, Goldfarb DS. Minimal change disease and IgA deposition: separate entities or common pathophysiology? Case Rep Nephrol. 2013; 2013:268401.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Remission of Nephrotic Syndrome in IgA Nephropathy
- A Case of Adult Minimal Change Nephrotic Syndrome Associated with Thin Basement Membrane Nephropathy
- A case of early gastric cancer with IgA nephropathy and minimal change nephrotic syndrome
- A Case of Overlapping Syndrome of Primary Membranous Nephropathy and IgA Nephropathy
- Significance of mesangial IgA deposition in minimal change nephrotic syndrome: a study of 60 cases