Cancer Res Treat.
2016 Oct;48(4):1187-1195. 10.4143/crt.2015.391.
Radiation Therapy Alone in cT1-3N0 Non-small Cell Lung Cancer Patients Who Are Unfit for Surgical Resection or Stereotactic Radiation Therapy: Comparison of Risk-Adaptive Dose Schedules
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- KMID: 2356221
- DOI: http://doi.org/10.4143/crt.2015.391
Abstract
- PURPOSE
High dose definitive radiation therapy (RT) alone is recommended to patients with cT1-3N0 non-small cell lung cancer, who are unfit for surgery or stereotactic RT. This study was conducted to evaluate the clinical outcomes and cost-effectiveness following RT alone using two different modest hypofractionation dose schemes.
MATERIALS AND METHODS
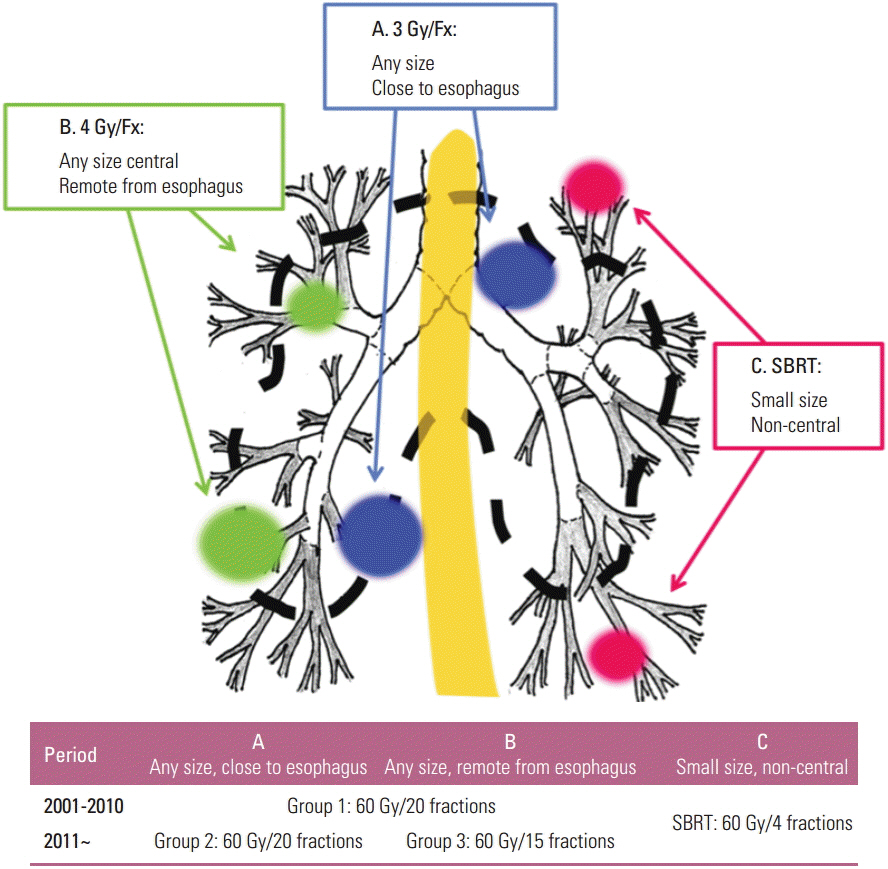
Between 2001 and 2014, 124 patients underwent RT alone. From 2001 till 2010, 60 Gy in 20 fractions was delivered to 79 patients (group 1). Since 2011, 60 Gy in 20 fractions (group 2, 20 patients), and 60 Gy in 15 fractions (group 3, 25 patients) were selectively chosen depending on estimated risk of esophagitis.
RESULTS
At follow-up of 16.7 months, 2-year rates of local control, progression-free survival, and overall survival were 62.6%, 39.1%, and 59.1%, respectively. Overall survival was significantly better in group 3 (p=0.002). In multivariate analyses, cT3 was the most powerful adverse factor affecting clinical outcomes. Incidence and severity of radiation pneumonitis were not different among groups, while no patients developed grade 2 esophagitis in group 3 (p=0.003). Under current Korean Health Insurance Policy, RT cost per person was 22.5% less in group 3 compared with others.
CONCLUSION
The current study demonstrated that 60 Gy in 15 fractions instead of 60 Gy in 20 fractions resulted in comparable clinical outcomes with excellent safety, direct cost saving, and improved convenience to the patients with tumors located at ≥ 1.5 cm from the esophagus.
MeSH Terms
Figure
Reference
-
References
1. Adebonojo SA, Bowser AN, Moritz DM, Corcoran PC. Impact of revised stage classification of lung cancer on survival: a military experience. Chest. 1999; 115:1507–13.2. Naruke T, Goya T, Tsuchiya R, Suemasu K. Prognosis and survival in resected lung carcinoma based on the new international staging system. J Thorac Cardiovasc Surg. 1988; 96:440–7.
Article3. Rowell NP, Williams CJ. Radical radiotherapy for stage I/II non-small cell lung cancer in patients not sufficiently fit for or declining surgery (medically inoperable): a systematic review. Thorax. 2001; 56:628–38.
Article4. Timmerman R, McGarry R, Yiannoutsos C, Papiez L, Tudor K, DeLuca J, et al. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol. 2006; 24:4833–9.
Article5. Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999; 43:1095–101.
Article6. Corradetti MN, Haas AR, Rengan R. Central-airway necrosis after stereotactic body-radiation therapy. N Engl J Med. 2012; 366:2327–9.
Article7. Oh D, Ahn YC, Kim B, Pyo H. Hypofractionated three-dimensional conformal radiation therapy alone for centrally located cT1-3N0 non-small-cell lung cancer. J Thorac Oncol. 2013; 8:624–9.
Article8. Soliman H, Cheung P, Yeung L, Poon I, Balogh J, Barbera L, et al. Accelerated hypofractionated radiotherapy for early-stage non-small-cell lung cancer: long-term results. Int J Radiat Oncol Biol Phys. 2011; 79:459–65.
Article9. Oh D, Ahn YC, Park HC, Lim DH, Han Y. Prediction of radiation pneumonitis following high-dose thoracic radiation therapy by 3 Gy/fraction for non-small cell lung cancer: analysis of clinical and dosimetric factors. Jpn J Clin Oncol. 2009; 39:151–7.
Article10. Ray KJ, Sibson NR, Kiltie AE. Treatment of breast and prostate cancer by hypofractionated radiotherapy: potential risks and benefits. Clin Oncol (R Coll Radiol). 2015; 27:420–6.
Article11. Oh D, Ahn YC, Seo JM, Shin EH, Park HC, Lim DH, et al. Potentially curative stereotactic body radiation therapy (SBRT) for single or oligometastasis to the lung. Acta Oncol. 2012; 51:596–602.
Article12. Bogart JA, Hodgson L, Seagren SL, Blackstock AW, Wang X, Lenox R, et al. Phase I study of accelerated conformal radiotherapy for stage I non-small-cell lung cancer in patients with pulmonary dysfunction: CALGB 39904. J Clin Oncol. 2010; 28:202–6.
Article13. Cheung P, Faria S, Ahmed S, Chabot P, Greenland J, Kurien E, et al. Phase II study of accelerated hypofractionated three-dimensional conformal radiotherapy for stage T1-3 N0 M0 non-small cell lung cancer: NCIC CTG BR.25. J Natl Cancer Inst. 2014; 106:dju164.
Article14. Lee JH, Wu HG, Kim HJ, Park CI, Lee SH, Kim DW, et al. Hypofractionated three-dimensional conformal radiotherapy for medically inoperable early stage non-small-cell lung cancer. Radiat Oncol J. 2013; 31:18–24.
Article15. Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, et al. Hypofractionated stereotactic radiotherapy (HypoFXSRT) for stage I non-small cell lung cancer: updated results of 257 patients in a Japanese multi-institutional study. J Thorac Oncol. 2007; 2(7 Suppl 3):S94–100.
Article16. Greenup RA, Camp MS, Taghian AG, Buckley J, Coopey SB, Gadd M, et al. Cost comparison of radiation treatment options after lumpectomy for breast cancer. Ann Surg Oncol. 2012; 19:3275–81.
Article17. Koshy M, Malik R, Weichselbaum RR, Sher DJ. Increasing radiation therapy dose is associated with improved survival in patients undergoing stereotactic body radiation therapy for stage I non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2015; 91:344–50.18. Park S, Urm S, Cho H. Analysis of biologically equivalent dose of stereotactic body radiotherapy for primary and metastatic lung tumors. Cancer Res Treat. 2014; 46:403–10.
Article19. Videtic GM, Stephans K, Reddy C, Gajdos S, Kolar M, Clouser E, et al. Intensity-modulated radiotherapy-based stereotactic body radiotherapy for medically inoperable early-stage lung cancer: excellent local control. Int J Radiat Oncol Biol Phys. 2010; 77:344–9.
Article20. Yamashita H, Haga A, Takahashi W, Takenaka R, Imae T, Takenaka S, et al. Volumetric modulated arc therapy for lung stereotactic radiation therapy can achieve high local control rates. Radiat Oncol. 2014; 9:243.
Article21. Bush DA, Cheek G, Zaheer S, Wallen J, Mirshahidi H, Katerelos A, et al. High-dose hypofractionated proton beam radiation therapy is safe and effective for central and peripheral early-stage non-small cell lung cancer: results of a 12-year experience at Loma Linda University Medical Center. Int J Radiat Oncol Biol Phys. 2013; 86:964–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Radiation Therapy for Non-small Cell Lung Cancer: Focused on Stereotactic Ablative Radiation Therapy in Stage I
- Management of Locally Advanced Non-small Cell Lung Cancer
- Stereotactic Body Radiation Therapy
- Treatment of Small Cell Lung Cancer
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer