J Korean Med Sci.
2016 Dec;31(12):2010-2019. 10.3346/jkms.2016.31.12.2010.
Gender-Specific Factors Associated with Suicide Attempts among the Community-Dwelling General Population with Suicidal Ideation: the 2013 Korean Community Health Survey
- Affiliations
-
- 1Department of Nursing, Graduate School, Chonnam National University, Gwangju, Korea.
- 2Department of Counseling Psychology, Graduate School of Dongshin University, Naju, Korea.
- 3Department of Preventive Medicine and Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea. lyh8275@hanmail.net
- 4Regional Cardiocerebrovascular Center, Wonkwang University Hospital, Iksan, Korea.
- KMID: 2355633
- DOI: http://doi.org/10.3346/jkms.2016.31.12.2010
Abstract
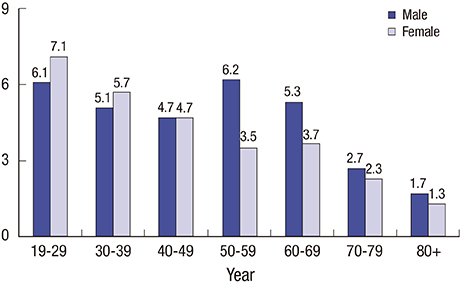
- We identified traditional risk factors and investigated poorly understood risk factors for suicide attempts according to gender in a large Korean population. We analyzed the data from 6,768 males and 12,475 females with suicidal ideation obtained from the nationwide 2013 Korean Community Health Survey. The dependent variable was suicide attempts within the past year. There was a significant trend towards an increase in suicide attempts with decreasing age in both genders. Compared with those who were married, suicide attempts were significantly higher among those who were widowed, divorced, or separated for males (odds ratio [OR], 2.07; 95% confidence interval [CI], 1.34-3.20), but lower for females (OR, 0.66; 95% CI, 0.45-0.98). Current smoking and depression were significant risk factor for suicide attempts in males and females. However, monthly household income, myocardial infarction, and osteoporosis were significantly associated with suicide attempts only in males, whereas education level, recipient of National Basic Livelihood Security, family contact, leisure activity, and drinking frequency were significantly associated only in females. These findings indicate that gender difference should be considered in the assessment, prevention, and management of future suicide attempts by community policy-makers and clinicians.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of Food Labeling Policy in Korea: Analyzing the Community Health Survey 2014–2017
Heui Sug Jo, Su Mi Jung
J Korean Med Sci. 2019;34(32):. doi: 10.3346/jkms.2019.34.e211.
Reference
-
1. Statistics Korea. Annual report on the cause of death statistics: 2014 [Internet]. accessed on 30 July 2016. Available at http://kosis.kr.2. Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003; 42:386–405.3. Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lepine JP, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999; 29:9–17.4. Kjøller M, Helweg-Larsen M. Suicidal ideation and suicide attempts among adult Danes. Scand J Public Health. 2000; 28:54–61.5. Bernal M, Haro JM, Bernert S, Brugha T, de Graaf R, Bruffaerts R, Lépine JP, de Girolamo G, Vilagut G, Gasquet I, et al. Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord. 2007; 101:27–34.6. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008; 192:98–105.7. Scocco P, de Girolamo G, Vilagut G, Alonso J. Prevalence of suicide ideation, plans, and attempts and related risk factors in Italy: results from the European study on the epidemiology of mental disorders--world mental health study. Compr Psychiatry. 2008; 49:13–21.8. Cheng JK, Fancher TL, Ratanasen M, Conner KR, Duberstein PR, Sue S, Takeuchi D. Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian Am J Psychol. 2010; 1:18–30.9. Kim MH, Jung-Choi K, Jun HJ, Kawachi I. Socioeconomic inequalities in suicidal ideation, parasuicides, and completed suicides in South Korea. Soc Sci Med. 2010; 70:1254–1261.10. Dai J, Chiu HF, Conner KR, Chan SS, Hou ZJ, Yu X, Caine ED. Suicidal ideation and attempts among rural Chinese aged 16-34 years--socio-demographic correlates in the context of a transforming China. J Affect Disord. 2011; 130:438–446.11. Vera M, Reyes-Rabanillo ML, Huertas S, Juarbe D, Pérez-Pedrogo C, Huertas A, Peña M. Suicide ideation, plans, and attempts among general practice patients with chronic health conditions in Puerto Rico. Int J Gen Med. 2011; 4:197–205.12. Handley TE, Inder KJ, Kay-Lambkin FJ, Stain HJ, Fitzgerald M, Lewin TJ, Attia JR, Kelly BJ. Contributors to suicidality in rural communities: beyond the effects of depression. BMC Psychiatry. 2012; 12:105.13. Li Y, Li Y, Cao J. Factors associated with suicidal behaviors in mainland China: a meta-analysis. BMC Public Health. 2012; 12:524.14. Aschan L, Goodwin L, Cross S, Moran P, Hotopf M, Hatch SL. Suicidal behaviours in South East London: prevalence, risk factors and the role of socio-economic status. J Affect Disord. 2013; 150:441–449.15. Miret M, Caballero FF, Huerta-Ramírez R, Moneta MV, Olaya B, Chatterji S, Haro JM, Ayuso-Mateos JL. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J Affect Disord. 2014; 163:1–9.16. Cho HD, Kim NY, Gil HW, Jeong DS, Hong SY. Comparison of families with and without a suicide prevention plan following a suicidal attempt by a family member. J Korean Med Sci. 2015; 30:974–978.17. Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008; 30:133–154.18. Kposowa AJ. Marital status and suicide in the national longitudinal mortality study. J Epidemiol Community Health. 2000; 54:254–261.19. Lorant V, Kunst AE, Huisman M, Costa G, Mackenbach J. EU Working Group on Socio-Economic Inequalities in Health. Socio-economic inequalities in suicide: a European comparative study. Br J Psychiatry. 2005; 187:49–54.20. Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides--a case-control study. Psychol Med. 2001; 31:1193–1202.21. Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004; 34:1331–1337.22. Stravynski A, Boyer R. Loneliness in relation to suicide ideation and parasuicide: a population-wide study. Suicide Life Threat Behav. 2001; 31:32–40.23. Schneider B, Baumert J, Schneider A, Marten-Mittag B, Meisinger C, Erazo N, Hammer GP, Ladwig KH. The effect of risky alcohol use and smoking on suicide risk: findings from the German MONICA/KORA-Augsburg cohort study. Soc Psychiatry Psychiatr Epidemiol. 2011; 46:1127–1132.24. Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict Behav. 2012; 37:982–985.25. Liu RT, Miller I. Life events and suicidal ideation and behavior: a systematic review. Clin Psychol Rev. 2014; 34:181–192.26. Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001; 31:837–845.27. Ro J, Park J, Lee J, Jung H. Factors that affect suicidal attempt risk among Korean elderly adults: a path analysis. J Prev Med Public Health. 2015; 48:28–37.28. Waern M, Rubenowitz E, Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. 2003; 49:328–334.29. Bae SM, Lee YJ, Cho IH, Kim SJ, Im JS, Cho SJ. Risk factors for suicidal ideation of the general population. J Korean Med Sci. 2013; 28:602–607.30. Webb RT, Kontopantelis E, Doran T, Qin P, Creed F, Kapur N. Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry. 2012; 69:256–264.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gender difference in socioeconomic factors affecting suicidal ideation and suicidal attempts among community-dwelling elderly: based on the Korea Community Health Survey
- Associated Factors of Suicidal Ideation in Community Residents with Suicidal Attempt Experiences
- Predictors of Suicidal Ideation in Community-dwelling Older Men: A Comparison between Young-old and Old-old
- Factors Related to Suicidal Ldeation in Community-Dwelling Older Adults with Multimorbidity Using Data From the 2017 Korean Community Health Survey
- Suicide Related Indicators and Trend of Korea in 2015