Perinatology.
2016 Sep;27(3):185-189. 10.14734/PN.2016.27.3.185.
Fetal Congenital Complete Atrioventricular Block in a Mother with Isolated Serum Anti-SSA/Ro and Anti-SSB/La Antibodies
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. drmaxmix.choi@samsung.com
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2355579
- DOI: http://doi.org/10.14734/PN.2016.27.3.185
Abstract
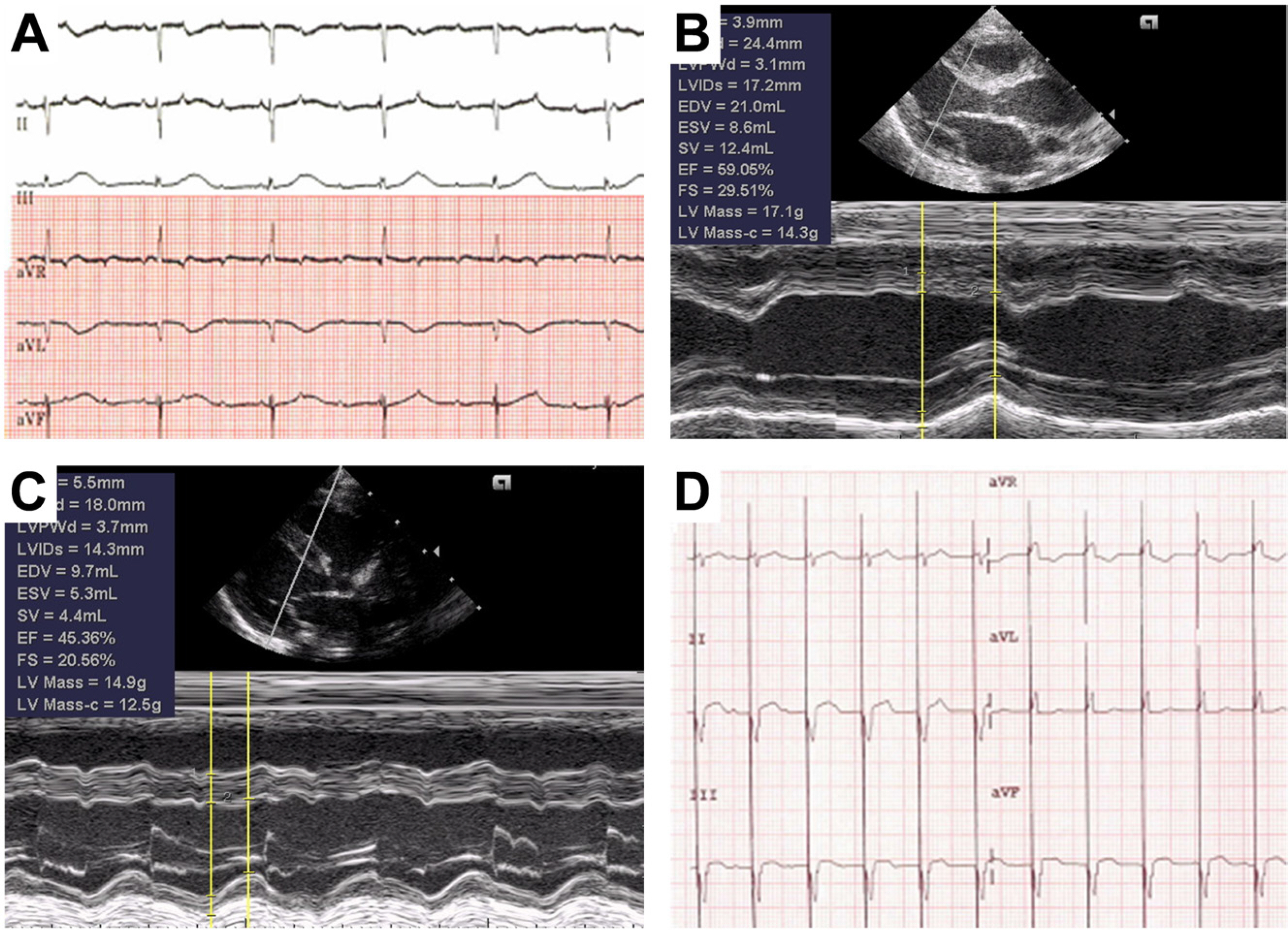
- Congenital atrioventricular block (AVB) is rare but carries a significant fetal or neonatal mortality and morbidity. In about half of the cases, it is associated with a congenital structural heart anomaly and often results from the transplacental transfer of maternal anti-SSA/Ro and/or anti-SSB/La autoantibodies in women with autoimmune diseases. We report a case of an isolated congenital AVB with cardiomegaly and pericardial effusion in a woman who had both serum anti-SSA/Ro and anti-SSB/La antibodies, but had no clinical or laboratory evidence of autoimmune diseases. The mother was treated with oral dexamethasone for about 10 days antenatally until the fetal pericardial effusion regressed. AVB persisted without any fetal compromise throughout the remaining gestational period until elective cesarean delivery at term. A permanent pacemaker was implanted into the baby at 2 weeks after birth due to hypotension and aggravating heart failure. The baby did not develop any complications and was discharged from the hospital.
MeSH Terms
Figure
Reference
-
1). Kuleva M., Le Bidois J., Decaudin A., Villain E., Costedoat-Chalumeau N., Lemercier D, et al. Clinical course and outcome of antenatally detected atrioventricular block: experience of a single tertiary centre and review of the literature. Prenat Diagn. 2015. 35:354–61.
Article2). Waltuck J., Buyon JP. Autoantibody-associated congenital heart block: outcome in mothers and children. Ann Intern Med. 1994. 120:544–51.
Article3). Ambrosi A., Wahren-Herlenius M. Congenital heart block: evidence for a pathogenic role of maternal autoantibodies. Arthritis Res Ther. 2012. 14:208.
Article4). Friedman DM., Kim MY., Copel JA., Llanos C., Davis C., Buyon JP. Prospective evaluation of fetuses with autoimmune-associated congenital heart block followed in the PR Interval and Dexamethasone Evaluation (PRIDE) Study. Am J Cardiol. 2009. 103:1102–6.
Article5). Lee JY., Hur SE., Lee SK. Prevention of anti-SSA/Ro and anti-SSB/La antibodies-mediated congenital heart block in pregnant woman with systemic lupus erythematosus: A case report. Korean J Obstet Gyne-col. 2012. 55:502–6.
Article6). Brucato A., Jonzon A., Friedman D., Allan LD., Vignati G., Gasparini M, et al. Proposal for a new definition of congenital complete atrioventricular block. Lupus. 2003. 12:427–35.
Article7). Brucato A., Cimaz R., Caporali R., Ramoni V., Buyon J. Pregnancy outcomes in patients with autoimmune diseases and anti-Ro/SSA antibodies. Clin Rev Allergy Immunol. 2011. 40:27–41.
Article8). Brucato A., Doria A., Frassi M., Castellino G., Franceschini F., Faden D, et al. Pregnancy outcome in 100 women with autoimmune diseases and anti-Ro/SSA antibodies: a prospective controlled study. Lupus. 2002. 11:716–21.9). Tonello M., Ruffatti A., Marson P., Tison T., Marozio L., Hoxha A, et al. Plasma exchange effectively removes 52- and 60-kDa anti-Ro/SSA and anti-La/SSB antibodies in pregnant women with congenital heart block. Transfusion. 2015. 55:1782–6.
Article10). Friedman DM., Llanos C., Izmirly PM., Brock B., Byron J., Copel J, et al. Evaluation of fetuses in a study of intravenous immunoglobulin as preventive therapy for congenital heart block: Results of a multicenter, prospective, open-label clinical trial. Arthritis Rheum. 2010. 62:1138–46.
Article11). Saxena A., Izmirly PM., Mendez B., Buyon JP., Friedman DM. Prevention and treatment in utero of autoimmune-associated congenital heart block. Cardiol Rev. 2014. 22:263–7.
Article12). Iozza I., Cianci S., Di Natale A., Garofalo G., Giacobbe AM., Giorgio E, et al. Update on systemic lupus erythematosus pregnancy. J Prenat Med. 2010. 4:67–73.13). Hutter D., Silverman ED., Jaeggi ET. The benefits of transplacental treatment of isolated congenital complete heart block associated with maternal anti-Ro/SSA antibodies: a review. Scand J Immunol. 2010. 72:235–41.
Article14). Fesslova V., Vignati G., Brucato A., De Sanctis M., Butera G., Pisoni MP, et al. The impact of treatment of the fetus by maternal therapy on the fetal and postnatal outcomes for fetuses diagnosed with isolated complete atrioventricular block. Cardiol Young. 2009. 19:282–90.
Article15). Jaeggi ET., Fouron JC., Silverman ED., Ryan G., Smallhorn J., Hornberger LK. Transplacental fetal treatment improves the outcome of prenatally diagnosed complete atrioventricular block without structural heart disease. Circulation. 2004. 110:1542–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of anti-SSA/Ro and anti-SSB/La antibodies-mediated congenital heart block in pregnant woman with systemic lupus erythematosus: A case report
- A case of neonatal lupus syndrome with congenital complete heart block
- A case of complete atrioventricular block in neonatal lupus erythematosus
- Neonatal Lupus Erythematosus
- Neonatal Lupus Erythematosus in an Infant Born to an Asymptomatic Mother with Anti-SSA/SSB Antibodies