Intest Res.
2016 Oct;14(4):343-350. 10.5217/ir.2016.14.4.343.
Symptomatic improvement with gluten restriction in irritable bowel syndrome: a prospective, randomized, double blinded placebo controlled trial
- Affiliations
-
- 1Department of Gastroenterology, Topiwala National Medical College & Bai Yamunabai Laxman Nair Ch Hospital, Mumbai, India. drvgzanwar@gmail.com
- KMID: 2354952
- DOI: http://doi.org/10.5217/ir.2016.14.4.343
Abstract
- BACKGROUND/AIMS
The existence of non-celiac gluten sensitivity has been debated. Indeed, the intestinal and extra-intestinal symptoms of many patients with irritable bowel syndrome (IBS) but without celiac disease or wheat allergy have been shown to improve on a gluten-free diet. Therefore, this study set out to evaluate the effects of gluten on IBS symptoms.
METHODS
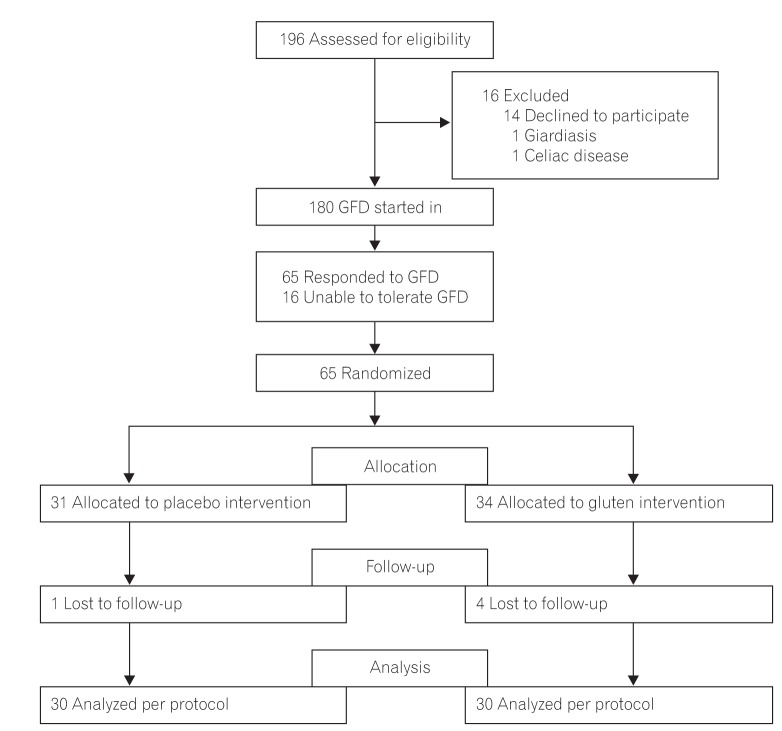
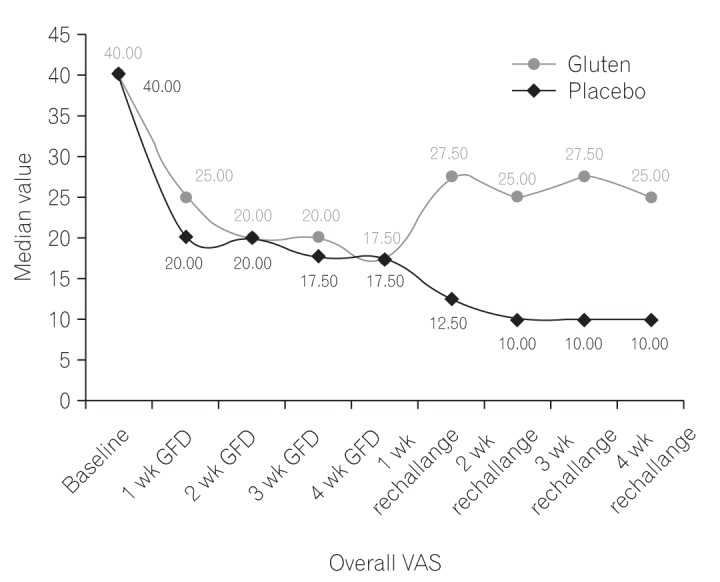
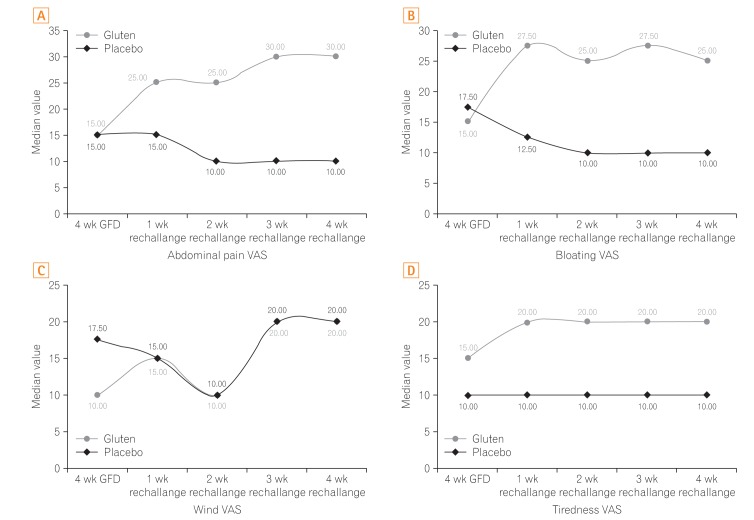
We performed a double-blind randomized placebo-controlled rechallenge trial in a tertiary care hospital with IBS patients who fulfilled the Rome III criteria. Patients with celiac disease and wheat allergy were appropriately excluded. The participants were administered a gluten-free diet for 4 weeks and were asked to complete a symptom-based questionnaire to assess their overall symptoms, abdominal pain, bloating, wind, and tiredness on the visual analog scale (0-100) at the baseline and every week thereafter. The participants who showed improvement were randomly assigned to one of two groups to receive either a placebo (gluten-free breads) or gluten (whole cereal breads) as a rechallenge for the next 4 weeks.
RESULTS
In line with the protocol analysis, 60 patients completed the study. The overall symptom score on the visual analog scale was significantly different between the two groups (P<0.05). Moreover, the patients in the gluten intervention group scored significantly higher in terms of abdominal pain, bloating, and tiredness (P<0.05), and their symptoms worsened within 1 week of the rechallenge.
CONCLUSIONS
A gluten diet may worsen the symptoms of IBS patients. Therefore, some form of gluten sensitivity other than celiac disease exists in some of them, and patients with IBS may benefit from gluten restrictions.
Keyword
MeSH Terms
Figure
Reference
-
2. Elli L, Branchi F, Tomba C, et al. Diagnosis of gluten related disorders: celiac disease, wheat allergy and non-celiac gluten sensitivity. World J Gastroenterol. 2015; 21:7110–7119. PMID: 26109797.
Article3. Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002; 123:2108–2131. PMID: 12454866.
Article4. Catassi C, Elli L, Bonaz B, et al. Diagnosis of non-celiac gluten sensitivity (NCGS): the Salerno Experts' Criteria. Nutrients. 2015; 7:4966–4977. PMID: 26096570.
Article5. Cash BD, Rubenstein JH, Young PE, et al. The prevalence of celiac disease among patients with nonconstipated irritable bowel syndrome is similar to controls. Gastroenterology. 2011; 141:1187–1193. PMID: 21762658.
Article6. Simpson S, Lebwohl B, Lewis SK, Tennyson CA, Sanders DS, Green PH. Awareness of gluten related disorders: a survey of the general public, chefs and patients. E Spen Eur E J Clin Nutr Metab. 2011; 6:e227–e231. DOI: 10.1016/j.eclnm.2011.08.001.7. Rostami K, Hogg-Kollars S. A patient's journey: non-coeliac gluten sensitivity. BMJ. 2012; 345:e7982. DOI: 10.1136/bmj.e7982. PMID: 23204003.8. DiGiacomo DV, Tennyson CA, Green PH, Demmer RT. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the Continuous National Health and Nutrition Examination Survey 2009-2010. Scand J Gastroenterol. 2013; 48:921–925. PMID: 23834276.
Article9. Biesiekierski JR, Newnham ED, Irving PM, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011; 106:508–514. PMID: 21224837.
Article10. Volta U, Tovoli F, Cicola R, et al. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J Clin Gastroenterol. 2012; 46:680–685. PMID: 22138844.
Article11. Massari S, Liso M, De Santis L, et al. Occurrence of nonceliac gluten sensitivity in patients with allergic disease. Int Arch Allergy Immunol. 2011; 155:389–394. PMID: 21346369.
Article12. Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013; 145:320–328.e3. PMID: 23648697.
Article13. Di Sabatino A, Volta U, Salvatore C, et al. Small amounts of gluten in subjects with suspected nonceliac gluten sensitivity: a randomized, double-blind, placebo-controlled, cross-over trial. Clin Gastroenterol Hepatol. 2015; 13:1604–1612.e3. PMID: 25701700.
Article14. Leffler D, Schuppan D, Pallav K, et al. Kinetics of the histological, serological and symptomatic responses to gluten challenge in adults with coeliac disease. Gut. 2013; 62:996–1004. PMID: 22619366.
Article15. Shahbazkhani B, Sadeghi A, Malekzadeh R, et al. Non-celiac gluten sensitivity has narrowed the spectrum of irritable bowel syndrome: a double-blind randomized placebo-controlled trial. Nutrients. 2015; 7:4542–4554. PMID: 26056920.
Article16. Piche T, Huet PM, Gelsi E, et al. Fatigue in irritable bowel syndrome: characterization and putative role of leptin. Eur J Gastroenterol Hepatol. 2007; 19:237–243. PMID: 17301651.
Article17. Vazquez-Roque MI, Camilleri M, Smyrk T, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndromediarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013; 144:903–911.e3. PMID: 23357715.
Article18. Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007; 5:844–850. PMID: 17553753.
Article19. Junker Y, Zeissig S, Kim SJ, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med. 2012; 209:2395–2408. PMID: 23209313.
Article20. Shepherd SJ, Parker FC, Muir JG, Gibson PR. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008; 6:765–771. PMID: 18456565.
Article21. Ghoshal UC, Abraham P, Bhatt C, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008; 27:22–28. PMID: 18541934.22. Simrén M, Månsson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001; 63:108–115.
Article23. Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013; 108:634–641. PMID: 23644955.
Article24. El-Salhy M, Ostgaard H, Gundersen D, Hatlebakk JG, Hausken T. The role of diet in the pathogenesis and management of irritable bowel syndrome (review). Int J Mol Med. 2012; 29:723–731. PMID: 22366773.
Article25. Zigich S, Heuberger R. The relationship of food intolerance and irritable bowel syndrome in adults. Gastroenterol Nurs. 2013; 36:275–282. PMID: 23899486.
Article26. Gibson PR. Food intolerance in functional bowel disorders. J Gastroenterol Hepatol. 2011; 26(Suppl 3):128–131. PMID: 21443725.
Article27. Sharma H, Verma AK, Das P, Dattagupta S, Ahuja V, Makharia GK. Prevalence of celiac disease in Indian patients with irritable bowel syndrome and uninvestigated dyspepsia. J Dig Dis. 2015; 16:443–448. PMID: 25959064.
Article28. Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet. 1978; 1:1358–1359.29. Cooper BT, Holmes GK, Ferguson R, Thompson RA, Allan RN, Cooke WT. Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology. 1980; 79(5 Pt 1):801–806. PMID: 7419003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emergence of Celiac Disease and Gluten-related Disorders in Asia
- Effect of Colostrum on the Symptoms and Mucosal Permeability in Patients with Irritable Bowel Syndrome: A Randomized Placebo-controlled Study
- Dietary Triggers in Irritable Bowel Syndrome: Is There a Role for Gluten?
- Placebo Effect in Clinical Trial Design for Irritable Bowel Syndrome
- The Effect of Phloroglucinol in Patients With Diarrhea-predominant Irritable Bowel Syndrome: A Randomized, Double-blind, Placebo-controlled Trial