J Korean Neurosurg Soc.
2016 Sep;59(5):471-477. 10.3340/jkns.2016.59.5.471.
Compression Angle of Ossification of the Posterior Longitudinal Ligament and Its Clinical Significance in Cervical Myelopathy
- Affiliations
-
- 1Department of Neurosurgery, Spine and Spinal Cord Institute, Yonsei University College of Medicine, Seoul, Korea. hayoon@yuhs.ac
- 2Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2351715
- DOI: http://doi.org/10.3340/jkns.2016.59.5.471
Abstract
OBJECTIVES
The correction of clinical and radiologic abnormalities in patients with symptomatic ossification of the posterior longitudinal ligament (OPLL) is the current mainstay of treatment. This study aimed to identify radiographic predictors of severity of myelopathy in patients with symptomatic OPLL.
METHODS
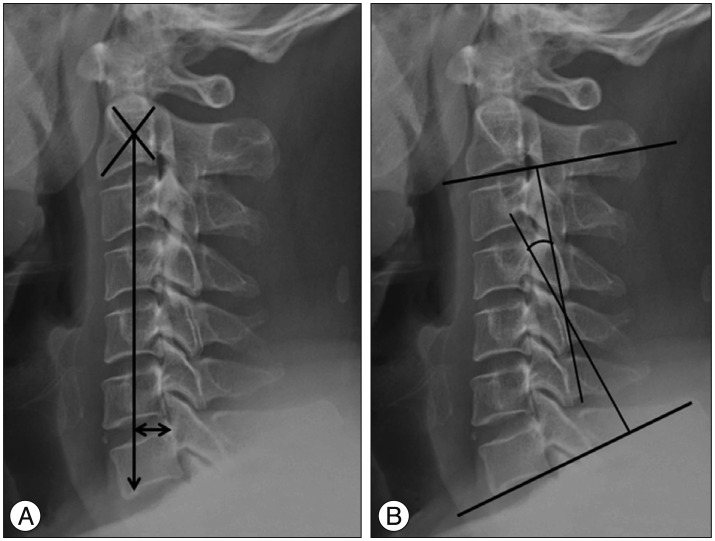
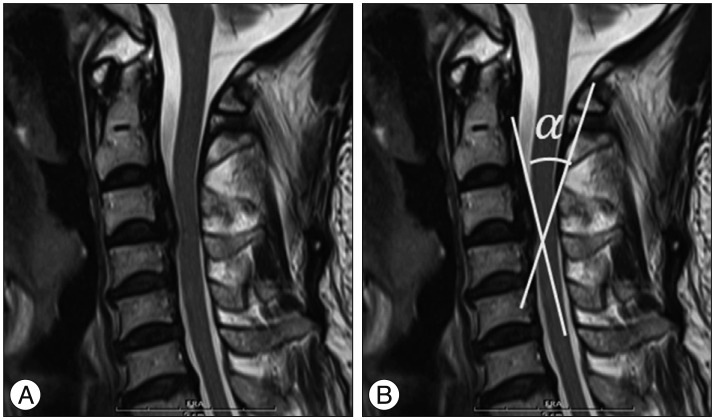
Fifty patients with symptomatic cervical OPLL were enrolled. Based on Japanese Orthopedic Association (JOA) scores, patients were divided into either the mild myelopathy (n=31) or severe myelopathy (n=19) group. All subjects underwent preoperative plain cervical roentgenogram, computed tomography (CT), and MR imaging (MRI). Radiological parameters (C2-7 sagittal vertical axis, SVA; C2-7 Cobb angle; C2-7 range of motion, ROM; OPLL occupying ratio; and compression angle) were compared. Compression angle of OPLL was defined as the angle between the cranial and caudal surfaces of OPLL at the maximum level of cord compression
RESULTS
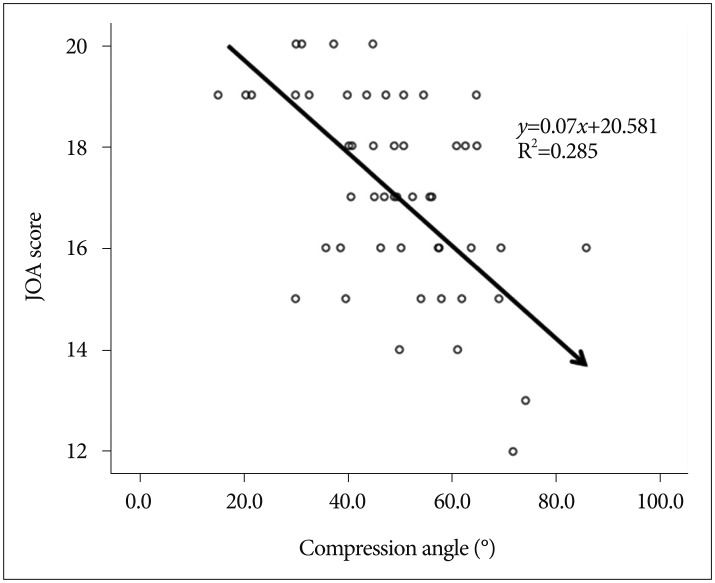
The occupying ratio of the spinal canal, C2-7 Cobb angle, C2-7 SVA, types of OPLL, and C2-7 ROM of the cervical spine were not statistically different between the two groups. However, the OPLL compression angle was significantly greater (p=0.003) in the severe myelopathy group than in the mild myelopathy group and was inversely correlated with JOA score (r=-0.533, p<0.01). Furthermore, multivariate regression analysis demonstrated that the compression angle (B=-0.069, p<0.001) was significantly associated with JOA scores (R=0.647, p<0.005).
CONCLUSION
Higher compression angles of OPLL have deleterious effects on the spinal cord and decrease preoperative JOA scores.
MeSH Terms
Figure
Reference
-
1. Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine (Phila Pa 1976). 2006; 31:2998–3005. PMID: 17172996.
Article2. Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity : effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg. 2004; 100:13–19. PMID: 14748568.
Article3. Fujiyoshi T, Yamazaki M, Okawa A, Kawabe J, Hayashi K, Endo T, et al. Static versus dynamic factors for the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Clin Neurosci. 2010; 17:320–324. PMID: 20071177.
Article4. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986; 11:521–524. PMID: 3787320.
Article5. Masaki Y, Yamazaki M, Okawa A, Aramomi M, Hashimoto M, Koda M, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament : anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007; 20:7–13. PMID: 17285045.
Article6. Masson C, Leys D, Meder JF, Dousset V, Pruvo JP. [Spinal cord ischemia]. J Neuroradiol. 2004; 31:35–46. PMID: 15026730.7. Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S, et al. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament : a multicenter cohort study. Spine (Phila Pa 1976). 2008; 33:2648–2650. PMID: 19011547.
Article8. Morio Y, Nagashima H, Teshima R, Nawata K. Radiological pathogenesis of cervical myelopathy in 60 consecutive patients with cervical ossification of the posterior longitudinal ligament. Spinal Cord. 1999; 37:853–857. PMID: 10602528.
Article9. Oshima Y, Seichi A, Takeshita K, Chikuda H, Ono T, Baba S, et al. Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spine (Phila Pa 1976). 2012; 37:1909–1913. PMID: 22511231.
Article10. Pavlov H, Torg JS, Robie B, Jahre C. Cervical spinal stenosis : determination with vertebral body ratio method. Radiology. 1987; 164:771–775. PMID: 3615879.
Article11. Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003; 28:1258–1262. PMID: 12811268.
Article12. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2015; 76(suppl 1):S14–S21. PMID: 25692364.
Article13. Taniyama T, Hirai T, Yamada T, Yuasa M, Enomoto M, Yoshii T, et al. Modified K-line in magnetic resonance imaging predicts insufficient decompression of cervical laminoplasty. Spine (Phila Pa 1976). 2013; 38:496–501. PMID: 22986838.
Article14. Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Effectiveness of posterior decompression for patients with ossification of the posterior longitudinal ligament in the thoracic spine : usefulness of the ossification-kyphosis angle on MRI. Spine (Phila Pa 1976). 2006; 31:E26–E30. PMID: 16395163.15. Tousignant M, de Bellefeuille L, O'Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine (Phila Pa 1976). 2000; 25:324–330. PMID: 10703104.
Article16. Tsukimoto H. On an autopsied case of compression myelopathy with a callus formation in the cervical spinal canal. Nihon Geka Hokan. 1960; 29:1003–1007.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament: 2 cases report
- Anterior Decompression and Fusion for the Treatment of Cervical Myelopathy Caused by Ossification of the Posterior Longitudinal Ligament: A Narrative Review
- A Case Quadriplegia due to Minor Head Trauma Associated with Ossification of the Posterior Longitudinal Ligament of the Cervical Spine
- Does Ossification of the Posterior Longitudinal Ligament Progress after Fusion?
- Cervical Myelopathy caused by Ossification of the Posterior Longitudinal Ligament