Korean J Urol.
2015 Nov;56(11):756-761. 10.4111/kju.2015.56.11.756.
Concurrent and predictive validation of robotic simulator Tube 3 module
- Affiliations
-
- 1Department of Urology, Korea University College of Medicine, Seoul, Korea. kkangsung76@daum.net
- KMID: 2351038
- DOI: http://doi.org/10.4111/kju.2015.56.11.756
Abstract
- PURPOSE
We previously described a new procedure specific module (Tube 3) to allow the practice of vesicourethral anastomosis after robot-assisted radical prostatectomy. Herein, we report a predetermined proficiency level of Tube 3 and preliminary validation to explore whether this new module can lead to performance improvement in the da Vinci system.
MATERIALS AND METHODS
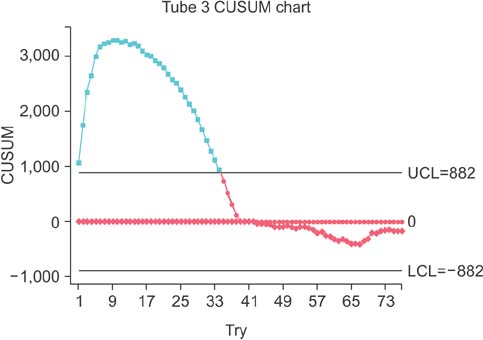
Eight urology residents and three urology fellows performed the Tube 3 module 1 hour daily for 7 days. The learning curve was depicted through a scatterplot and the stable point was identified through the cumulative sum chart. Concurrent and predictive validations were performed with the da Vinci system. The mean time to complete the task and end product rating score between Tube 3 training group and no Tube 3 training group were compared.
RESULTS
Concerning the learning curve, about 41 repetitions comprising about 5 hours were needed to achieve this stable point when the mean time to complete Tube of 384 seconds was set as a target. With regarding to the concurrent and predictive validation, there significant differences were evident in the mean time to complete 16 needle passages and the vesicourethral anastomosis and the end product rating score.
CONCLUSIONS
The virtual reality (VR) simulator can yield sufficient improvement in technical performance in Tube 3 within 5 hours. The acquired proficiency can be transferable to the vesicourethral anastomosis using the da Vinci system.
Keyword
MeSH Terms
Figure
Reference
-
1. Hung AJ, Jayaratna IS, Teruya K, Desai MM, Gill IS, Goh AC. Comparative assessment of three standardized robotic surgery training methods. BJU Int. 2013; 112:864–871.2. Kang SG, Cho S, Kang SH, Haidar AM, Samavedi S, Palmer KJ, et al. The Tube 3 module designed for practicing vesicourethral anastomosis in a virtual reality robotic simulator: determination of face, content, and construct validity. Urology. 2014; 84:345–350.3. Kang SG, Yang KS, Ko YH, Kang SH, Park HS, Lee JG, et al. A study on the learning curve of the robotic virtual reality simulator. J Laparoendosc Adv Surg Tech A. 2012; 22:438–442.4. Kenney PA, Wszolek MF, Gould JJ, Libertino JA, Moinzadeh A. Face, content, and construct validity of dV-trainer, a novel virtual reality simulator for robotic surgery. Urology. 2009; 73:1288–1292.5. Sethi AS, Peine WJ, Mohammadi Y, Sundaram CP. Validation of a novel virtual reality robotic simulator. J Endourol. 2009; 23:503–508.6. Liss MA, McDougall EM. Robotic surgical simulation. Cancer J. 2013; 19:124–129.7. Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, et al. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013; 81:767–774.8. Kang SG, Ryu BJ, Yang KS, Ko YH, Cho S, Kang SH, et al. An effective repetitive training schedule to achieve skill proficiency using a novel robotic virtual reality simulator. J Surg Educ. 2015; 72:369–376.9. Hung AJ, Patil MB, Zehnder P, Cai J, Ng CK, Aron M, et al. Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. J Urol. 2012; 187:630–637.10. Van Velthoven RF, Ahlering TE, Peltier A, Skarecky DW, Clayman RV. Technique for laparoscopic running urethrovesical anastomosis:the single knot method. Urology. 2003; 61:699–702.11. Sabbagh R, Chatterjee S, Chawla A, Hoogenes J, Kapoor A, Matsumoto ED. Transfer of laparoscopic radical prostatectomy skills from bench model to animal model: a prospective, single-blind, randomized, controlled study. J Urol. 2012; 187:1861–1866.12. Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001; 87:408–410.13. Sterrett SP, Jarrard DF. Robotic assisted laparoscopic radical prostatectomy: evolution and outcomes. Minerva Urol Nefrol. 2008; 60:31–39.14. Ou YC, Yang CR, Wang J, Yang CK, Cheng CL, Patel VR, et al. The learning curve for reducing complications of robotic-assisted laparoscopic radical prostatectomy by a single surgeon. BJU Int. 2011; 108:420–425.15. Sahabudin RM, Arni T, Ashani N, Arumuga K, Rajenthran S, Murali S, et al. Development of robotic program: an Asian experience. World J Urol. 2006; 24:161–164.16. Reznick R, Regehr G, MacRae H, Martin J, McCulloch W. Testing technical skill via an innovative "bench station" examination. Am J Surg. 1997; 173:226–230.17. Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg. 1999; 177:167–170.18. Wanzel KR, Matsumoto ED, Hamstra SJ, Anastakis DJ. Teaching technical skills: training on a simple, inexpensive, and portable model. Plast Reconstr Surg. 2002; 109:258–263.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Application of PBL Module Using Simulator: Focused on Simman
- A Validation Study of Surveillance Data: Focus on the Korean National Healthcare-associated Infections Surveillance System (KONIS), Intensive Care Unit Module
- Development of a prototype simulator for dental education
- A Newly Designed 3-Dimensional Printer-Based Gastric Hemostasis Simulator with Two Modules for Endoscopic Trainees (with Video)
- Tube thoracostomy training with a medical simulator is associated with faster, more successful performance of the procedure