J Periodontal Implant Sci.
2016 Aug;46(4):254-265. 10.5051/jpis.2016.46.4.254.
Primary implant stability in a bone model simulating clinical situations for the posterior maxilla: an in vitro study
- Affiliations
-
- 1Department of Periodontology, Kyung Hee University School of Dentistry, Seoul, Korea. ssyislet@khu.ac.kr
- 2Department of Periodontology, Periodontal-Implant Clinical Research Institute, Kyung Hee University Dental Hospital, Seoul, Korea.
- 3Department of Biomaterials & Prosthodontics, Institute of Oral Biology, Kyung Hee University School of Dentistry, Seoul, Korea.
- 4Department of Dentistry & Periodontology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2350026
- DOI: http://doi.org/10.5051/jpis.2016.46.4.254
Abstract
- PURPOSE
The aim of this study was to determine the influence of anatomical conditions on primary stability in the models simulating posterior maxilla.
METHODS
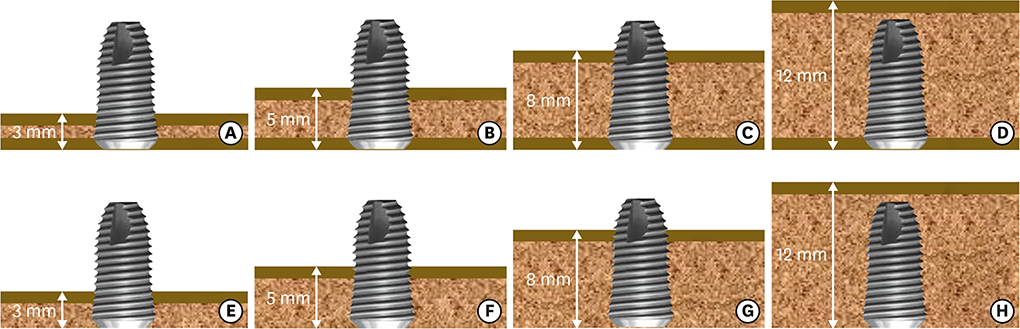
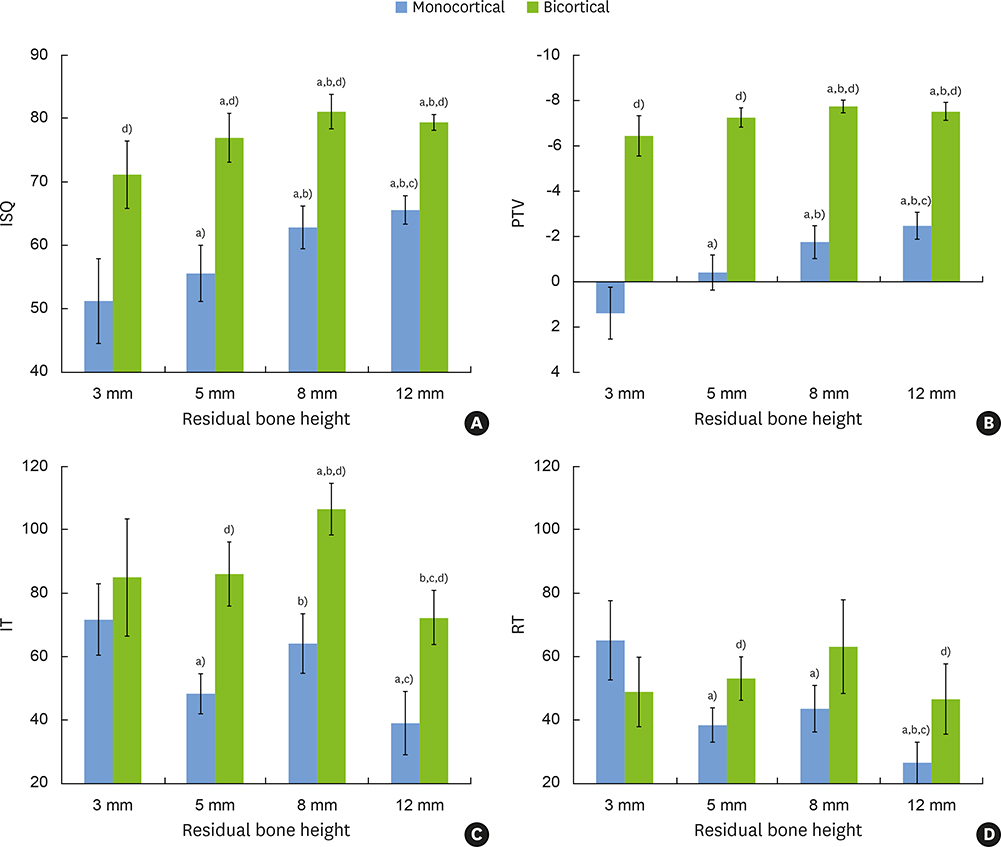
Polyurethane blocks were designed to simulate monocortical (M) and bicortical (B) conditions. Each condition had four subgroups measuring 3 mm (M3, B3), 5 mm (M5, B5), 8 mm (M8, B8), and 12 mm (M12, B12) in residual bone height (RBH). After implant placement, the implant stability quotient (ISQ), Periotest value (PTV), insertion torque (IT), and reverse torque (RT) were measured. Two-factor ANOVA (two cortical conditions×four RBHs) and additional analyses for simple main effects were performed.
RESULTS
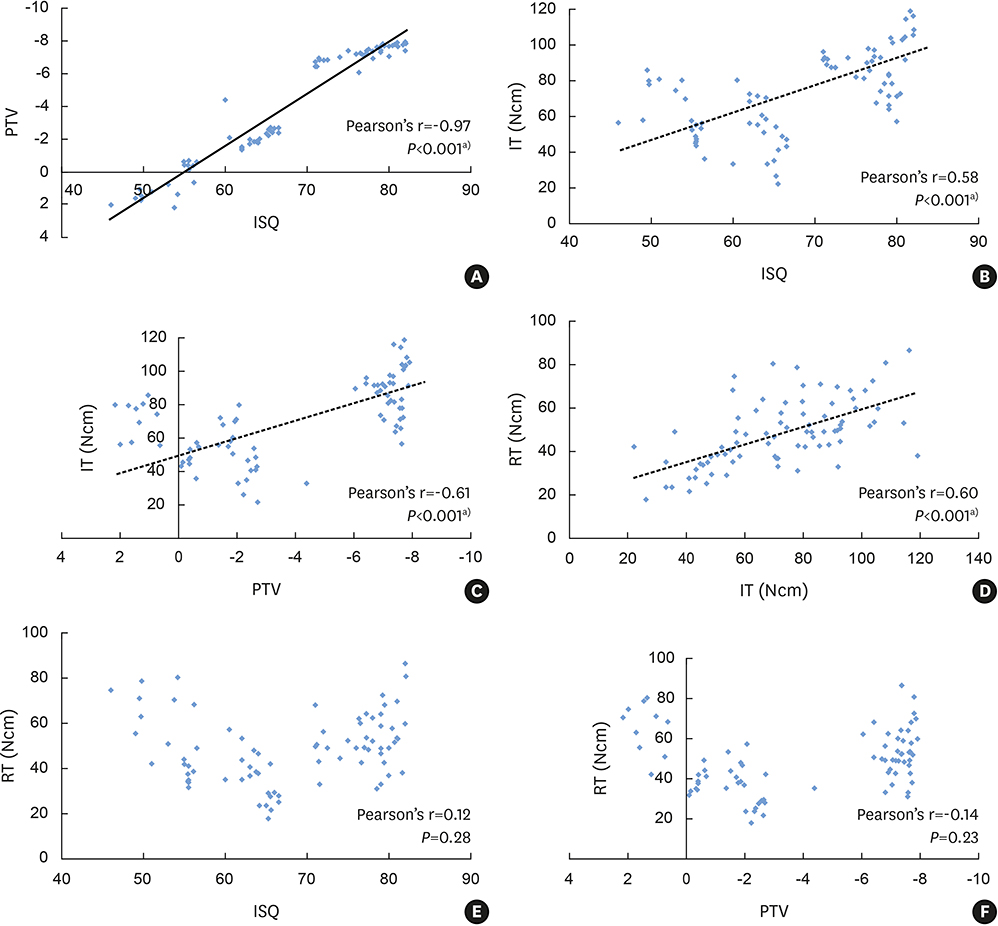
A significant interaction between cortical condition and RBH was demonstrated for all methods measuring stability with two-factor ANOVA. In the analyses for simple main effects, ISQ and PTV were statistically higher in the bicortical groups than the corresponding monocortical groups, respectively. In the monocortical group, ISQ and PTV showed a statistically significant rise with increasing RBH. Measurements of IT and RT showed a similar tendency, measuring highest in the M3 group, followed by the M8, the M5, and the M12 groups. In the bicortical group, all variables showed a similar tendency, with different degrees of rise and decline. The B8 group showed the highest values, followed by the B12, the B5, and the B3 groups. The highest coefficient was demonstrated between ISQ and PTV.
CONCLUSIONS
Primary stability was enhanced by the presence of bicortex and increased RBH, which may be better demonstrated by ISQ and PTV than by IT and RT.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of implant stability measurements between a resonance frequency analysis device and a modified damping capacity analysis device: an in vitro study
Jungwon Lee, Se-Wook Pyo, Hyun-Jae Cho, Jung-Sub An, Jae-Hyun Lee, Ki-Tae Koo, Yong-Moo Lee
J Periodontal Implant Sci. 2020;50(1):56-66. doi: 10.5051/jpis.2020.50.1.56.
Reference
-
1. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996; 7:261–267.
Article2. Roccuzzo M, Aglietta M, Cordaro L. Implant loading protocols for partially edentulous maxillary posterior sites. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 147–157.3. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008; 47:51–66.
Article4. Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants. 2007; 22:743–754.5. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998; 11:491–501.6. Shin SY, Shin SI, Kye SB, Hong J, Paeng JY, Chang SW, et al. The effects of defect type and depth, and measurement direction on the implant stability quotient value. J Oral Implantol. 2015; 41:652–656.
Article7. Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lindström J, Rockler B. An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. J Oral Maxillofac Surg. 1984; 42:497–505.
Article8. Jensen J, Sindet-Pedersen S, Oliver AJ. Varying treatment strategies for reconstruction of maxillary atrophy with implants: results in 98 patients. J Oral Maxillofac Surg. 1994; 52:210–216.
Article9. Ivanoff CJ, Sennerby L, Lekholm U. Influence of mono- and bicortical anchorage on the integration of titanium implants. A study in the rabbit tibia. Int J Oral Maxillofac Surg. 1996; 25:229–235.
Article10. Van Oosterwyck H, Duyck J, Vander Sloten J, Van der Perre G, De Cooman M, Lievens S, et al. The influence of bone mechanical properties and implant fixation upon bone loading around oral implants. Clin Oral Implants Res. 1998; 9:407–418.
Article11. Bahat O. Treatment planning and placement of implants in the posterior maxillae: report of 732 consecutive Nobelpharma implants. Int J Oral Maxillofac Implants. 1993; 8:151–161.12. Akça K, Chang TL, Tekdemir I, Fanuscu MI. Biomechanical aspects of initial intraosseous stability and implant design: a quantitative micro-morphometric analysis. Clin Oral Implants Res. 2006; 17:465–472.
Article13. Schulte W, Lukas D. Periotest to monitor osseointegration and to check the occlusion in oral implantology. J Oral Implantol. 1993; 19:23–32.14. Aparicio C, Lang NP, Rangert B. Validity and clinical significance of biomechanical testing of implant/bone interface. Clin Oral Implants Res. 2006; 17:Suppl 2. 2–7.
Article15. Devlin H, Horner K, Ledgerton D. A comparison of maxillary and mandibular bone mineral densities. J Prosthet Dent. 1998; 79:323–327.
Article16. Raghavendra S, Wood MC, Taylor TD. Early wound healing around endosseous implants: a review of the literature. Int J Oral Maxillofac Implants. 2005; 20:425–431.17. Cakur B, Sümbüllü MA, Durna D. Relationship among Schneiderian membrane, Underwood's septa, and the maxillary sinus inferior border. Clin Implant Dent Relat Res. 2013; 15:83–87.
Article18. Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery--clinical, prospective, biomechanical, and imaging study. Bone. 2005; 37:776–780.
Article19. Akkocaoglu M, Uysal S, Tekdemir I, Akca K, Cehreli MC. Implant design and intraosseous stability of immediately placed implants: a human cadaver study. Clin Oral Implants Res. 2005; 16:202–209.
Article20. Nkenke E, Hahn M, Weinzierl K, Radespiel-Tröger M, Neukam FW, Engelke K. Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res. 2003; 14:601–609.
Article21. Heidari B, Khalesi M, Khodadoustan A, Kadkhodazadeh M. The influence of cortical width of sheep bone on the primary stability of dental implants: an in vitro study. J Long Term Eff Med Implants. 2013; 23:87–91.
Article22. Shin SY, Shin SI, Kye SB, Chang SW, Hong J, Paeng JY, et al. Bone cement grafting increases implant primary stability in circumferential cortical bone defects. J Periodontal Implant Sci. 2015; 45:30–35.
Article23. Ahn SJ, Leesungbok R, Lee SW, Heo YK, Kang KL. Differences in implant stability associated with various methods of preparation of the implant bed: an in vitro study. J Prosthet Dent. 2012; 107:366–372.
Article24. Yan X, Zhang X, Chi W, Ai H, Wu L. Comparing the influence of crestal cortical bone and sinus floor cortical bone in posterior maxilla bi-cortical dental implantation: a three-dimensional finite element analysis. Acta Odontol Scand. 2015; 73:312–320.
Article25. Hong J, Lim YJ, Park SO. Quantitative biomechanical analysis of the influence of the cortical bone and implant length on primary stability. Clin Oral Implants Res. 2012; 23:1193–1197.
Article26. Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Brånemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991; 6:142–146.27. Jung UW, Kim S, Kim YH, Cha JK, Lee IS, Choi SH. Osseointegration of dental implants installed without mechanical engagement: a histometric analysis in dogs. Clin Oral Implants Res. 2012; 23:1297–1301.
Article28. Rea M, Lang NP, Ricci S, Mintrone F, González González G, Botticelli D. Healing of implants installed in over- or under-prepared sites--an experimental study in dogs. Clin Oral Implants Res. 2015; 26:442–446.
Article29. Ivanoff CJ, Gröndahl K, Bergström C, Lekholm U, Brånemark PI. Influence of bicortical or monocortical anchorage on maxillary implant stability: a 15-year retrospective study of Brånemark System implants. Int J Oral Maxillofac Implants. 2000; 15:103–110.30. Krafft T, Graef F, Karl M. Osstell resonance frequency measurement values as a prognostic factor in implant dentistry. J Oral Implantol. 2015; 41:e133–7.
Article31. Molly L. Bone density and primary stability in implant therapy. Clin Oral Implants Res. 2006; 17:Suppl 2. 124–135.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of osteotome technique on primary implant stability according to implant fixture diameter
- The factors that influence postoperative stability of the dental implants in posterior edentulous maxilla
- A comparison of the implant stability among various implant systems: clinical study
- Evaluation of reliability of zirconia materials to be used in implant-retained restoration on the atrophic bone of the posterior maxilla: A finite element study
- Implant placement simultaneously sinus augmentation using crestal approach in severely atrophic maxilla; minimally invasive approach