J Periodontal Implant Sci.
2016 Aug;46(4):220-233. 10.5051/jpis.2016.46.4.220.
“Over-inlay†block graft and differential morphometry: a novel block graft model to study bone regeneration and host-to-graft interfaces in rats
- Affiliations
-
- 1Department of Biomedical, Biotechnological, and Translational Sciences (S.Bi.Bi.T), University of Parma Dental Medicine Unit, Parma, Italy. simone.lumetti@unipr.it
- 2Department of Biomedical, Biotechnological, and Translational Sciences (S.Bi.Bi.T), University of Parma General Pathology Unit, Parma, Italy.
- 3Department of Veterinary Science, University of Parma, Parma, Italy.
- 4Institute of Materials for Electronics and Magnetism (IMEM), Italian National Research Council (CNR), Parco Area delle Scienze, Parma, Italy.
- KMID: 2350023
- DOI: http://doi.org/10.5051/jpis.2016.46.4.220
Abstract
- PURPOSE
The aim of this study was to present new a model that allows the study of the bone healing process, with an emphasis on the biological behavior of different graft-to-host interfaces. A standardized "over-inlay" surgical technique combined with a differential histomorphometric analysis is presented in order to optimize the use of critical-size calvarial defects in pre-clinical testing.
METHODS
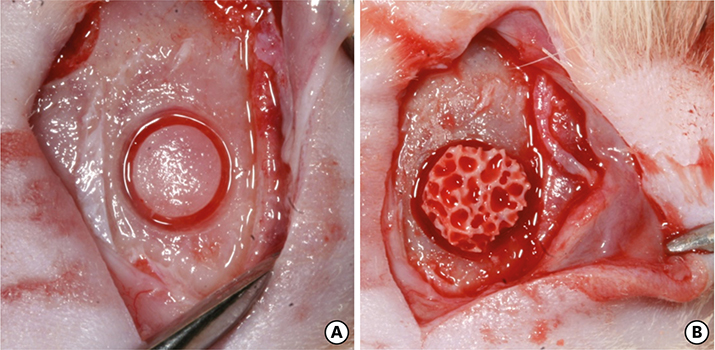
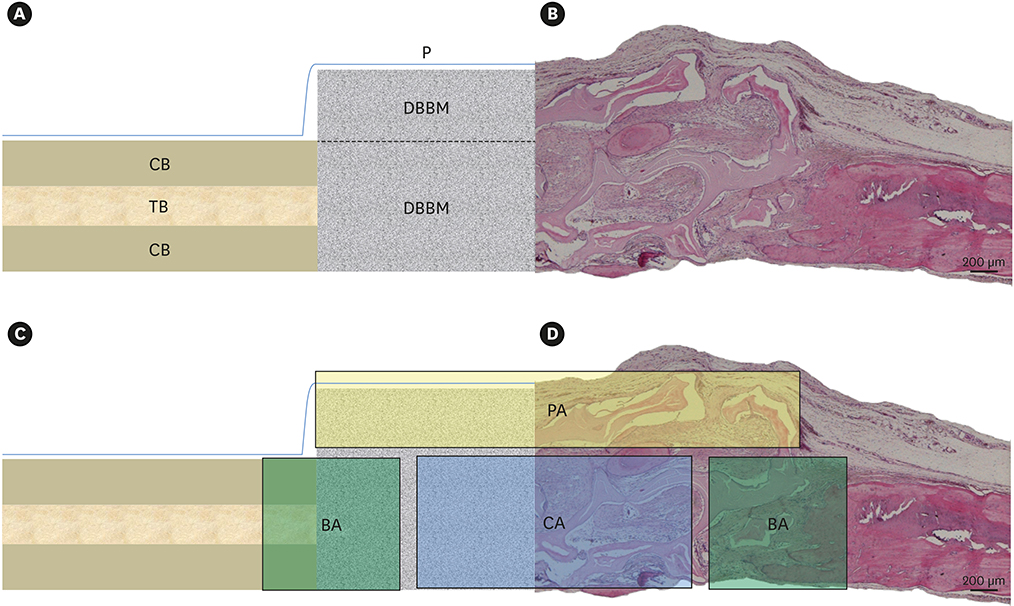
Critical-size defects were created into the parietal bone of 8 male Wistar rats. Deproteinized bovine bone (DBBM) blocks were inserted into the defects, so that part of the block was included within the calvarial thickness and part exceeded the calvarial height (an "over-inlay" graft). All animals were sacrificed at 1 or 3 months. Histomorphometric and immunohistochemical evaluation was carried out within distinct regions of interest (ROIs): the areas adjacent to the native bone (BA), the periosteal area (PA) and the central area (CA).
RESULTS
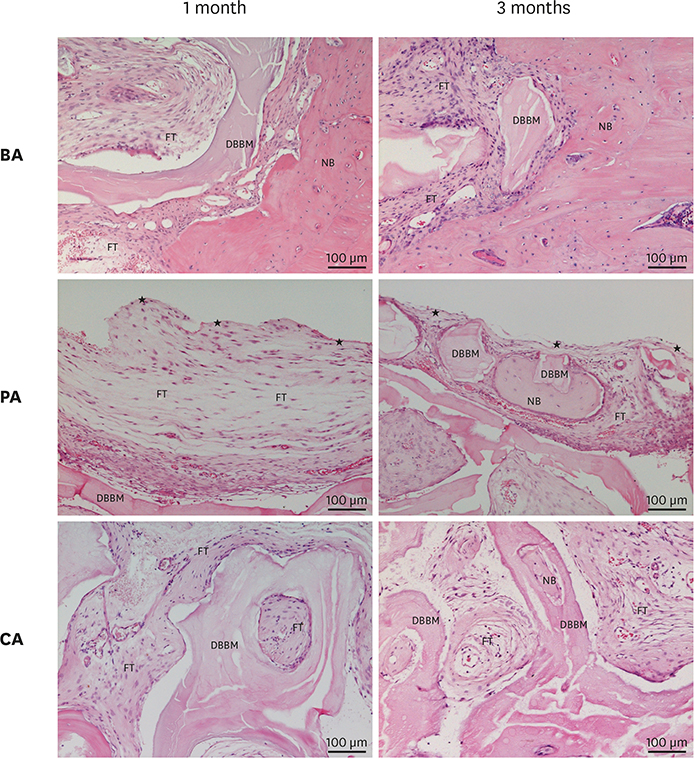
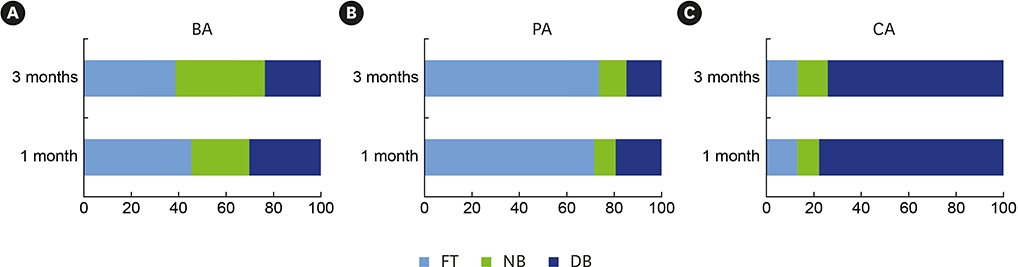
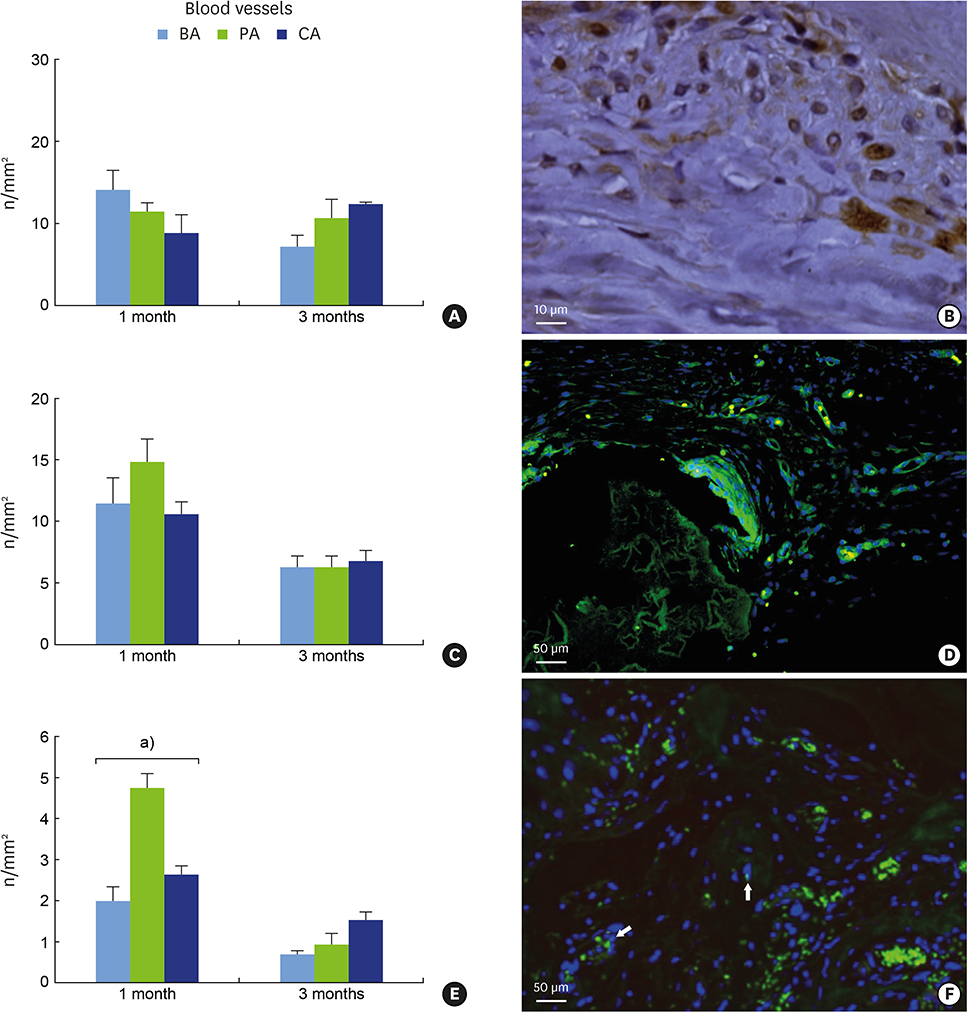
The animals healed without complications. Differential morphometry allowed the examination of the tissue composition within distinct regions: the BA presented consistent amounts of new bone formation (NB), which increased over time (24.53%±1.26% at 1 month; 37.73%±0.39% at 3 months), thus suggesting that this area makes a substantial contribution toward NB. The PA was mainly composed of fibrous tissue (71.16%±8.06% and 78.30%±2.67%, respectively), while the CA showed high amounts of DBBM at both time points (78.30%±2.67% and 74.68%±1.07%, respectively), demonstrating a slow remodeling process. Blood vessels revealed a progressive migration from the interface with native bone toward the central area of the graft. Osterix-positive cells observed at 1 month within the PA suggested that the periosteum was a source of osteoprogenitor elements. Alkaline phosphatase data on matrix deposition confirmed this observation.
CONCLUSIONS
The present model allowed for a standardized investigation of distinct graft-to-host interfaces both at vertically augmented and inlay-augmented sites, thus possibly limiting the number of animals required for pre-clinical investigations.
Keyword
MeSH Terms
Figure
Reference
-
1. Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am Acad Orthop Surg. 2005; 13:77–86.
Article2. Giuliani N, Lisignoli G, Magnani M, Racano C, Bolzoni M, Dalla Palma B, et al. New insights into osteogenic and chondrogenic differentiation of human bone marrow mesenchymal stem cells and their potential clinical applications for bone regeneration in pediatric orthopaedics. Stem Cells Int. 2013; 2013:312501.
Article3. Wang P, Liu X, Zhao L, Weir MD, Sun J, Chen W, et al. Bone tissue engineering via human induced pluripotent, umbilical cord and bone marrow mesenchymal stem cells in rat cranium. Acta Biomater. 2015; 18:236–248.
Article4. Liu W, Konermann A, Guo T, Jäger A, Zhang L, Jin Y. Canonical Wnt signaling differently modulates osteogenic differentiation of mesenchymal stem cells derived from bone marrow and from periodontal ligament under inflammatory conditions. Biochim Biophys Acta. 2014; 1840:1125–1134.
Article5. Colnot C, Zhang X, Knothe Tate ML. Current insights on the regenerative potential of the periosteum: molecular, cellular, and endogenous engineering approaches. J Orthop Res. 2012; 30:1869–1878.
Article6. Zhang X, Xie C, Lin AS, Ito H, Awad H, Lieberman JR, et al. Periosteal progenitor cell fate in segmental cortical bone graft transplantations: implications for functional tissue engineering. J Bone Miner Res. 2005; 20:2124–2137.
Article7. Nagata M, Hoshina H, Li M, Arasawa M, Uematsu K, Ogawa S, et al. A clinical study of alveolar bone tissue engineering with cultured autogenous periosteal cells: coordinated activation of bone formation and resorption. Bone. 2012; 50:1123–1129.
Article8. Gomes PS, Fernandes MH. Rodent models in bone-related research: the relevance of calvarial defects in the assessment of bone regeneration strategies. Lab Anim. 2011; 45:14–24.
Article9. Stavropoulos A, Sculean A, Bosshardt DD, Buser D, Klinge B. Pre-clinical in vivo models for the screening of bone biomaterials for oral/craniofacial indications: focus on small-animal models. Periodontol 2000. 2015; 68:55–65.
Article10. Bosch C, Melsen B, Vargervik K. Importance of the critical-size bone defect in testing bone-regenerating materials. J Craniofac Surg. 1998; 9:310–316.
Article11. Donos N, Lang NP, Karoussis IK, Bosshardt D, Tonetti M, Kostopoulos L. Effect of GBR in combination with deproteinized bovine bone mineral and/or enamel matrix proteins on the healing of critical-size defects. Clin Oral Implants Res. 2004; 15:101–111.
Article12. Zigdon-Giladi H, Bick T, Morgan EF, Lewinson D, Machtei EE. Peripheral blood-derived endothelial progenitor cells enhance vertical bone formation. Clin Implant Dent Relat Res. 2015; 17:83–92.
Article13. Hopper RA, Zhang JR, Fourasier VL, Morova-Protzner I, Protzner KF, Pang CY, et al. Effect of isolation of periosteum and dura on the healing of rabbit calvarial inlay bone grafts. Plast Reconstr Surg. 2001; 107:454–462.
Article14. Guskuma MH, Hochuli-Vieira E, Pereira FP, Rangel-Garcia Junior I, Okamoto R, Okamoto T, et al. Bone regeneration in surgically created defects filled with autogenous bone: an epifluorescence microscopy analysis in rats. J Appl Oral Sci. 2010; 18:346–353.
Article15. Russell WM, Burch RL. The principles of humane experimental technique. London: Methuen;1959.16. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191.
Article17. Cacchioli A, Ravanetti F, Soliani L, Borghetti P. Preliminary study on the mineral apposition rate in distal femoral epiphysis of New Zealand white rabbit at skeletal maturity. Anat Histol Embryol. 2012; 41:163–169.
Article18. Fontana F, Rocchietta I, Dellavia C, Nevins M, Simion M. Biocompatibility and manageability of a new fixable bone graft for the treatment of localized bone defects: preliminary study in a dog model. Int J Periodontics Restorative Dent. 2008; 28:601–607.19. Zecha PJ, Schortinghuis J, van der Wal JE, Nagursky H, van den Broek KC, Sauerbier S, et al. Applicability of equine hydroxyapatite collagen (eHAC) bone blocks for lateral augmentation of the alveolar crest. A histological and histomorphometric analysis in rats. Int J Oral Maxillofac Surg. 2011; 40:533–542.
Article20. Xuan F, Lee CU, Son JS, Fang Y, Jeong SM, Choi BH. Vertical ridge augmentation using xenogenous bone blocks: a comparison between the flap and tunneling procedures. J Oral Maxillofac Surg. 2014; 72:1660–1670.
Article21. Li J, Xuan F, Choi BH, Jeong SM. Minimally invasive ridge augmentation using xenogenous bone blocks in an atrophied posterior mandible: a clinical and histological study. Implant Dent. 2013; 22:112–116.
Article22. Rothamel D, Schwarz F, Herten M, Ferrari D, Mischkowski RA, Sager M, et al. Vertical ridge augmentation using xenogenous bone blocks: a histomorphometric study in dogs. Int J Oral Maxillofac Implants. 2009; 24:243–250.23. De Santis E, Lang NP, Favero G, Beolchini M, Morelli F, Botticelli D. Healing at mandibular block-grafted sites. An experimental study in dogs. Clin Oral Implants Res. 2015; 26:516–522.
Article24. Araújo MG, Sonohara M, Hayacibara R, Cardaropoli G, Lindhe J. Lateral ridge augmentation by the use of grafts comprised of autologous bone or a biomaterial. An experiment in the dog. J Clin Periodontol. 2002; 29:1122–1131.
Article25. Hoffman MD, Benoit DS. Emulating native periosteum cell population and subsequent paracrine factor production to promote tissue engineered periosteum-mediated allograft healing. Biomaterials. 2015; 52:426–440.
Article26. Adeyemo WL, Reuther T, Bloch W, Korkmaz Y, Fischer JH, Zöller JE, et al. Influence of host periosteum and recipient bed perforation on the healing of onlay mandibular bone graft: an experimental pilot study in the sheep. Oral Maxillofac Surg. 2008; 12:19–28.
Article27. Vajgel A, Mardas N, Farias BC, Petrie A, Cimões R, Donos N. A systematic review on the critical size defect model. Clin Oral Implants Res. 2014; 25:879–893.
Article28. Fuegl A, Tangl S, Keibl C, Watzek G, Redl H, Gruber R. The impact of ovariectomy and hyperglycemia on graft consolidation in rat calvaria. Clin Oral Implants Res. 2011; 22:524–529.
Article29. Milani S, Dal Pozzo L, Rasperini G, Sforza C, Dellavia C. Deproteinized bovine bone remodeling pattern in alveolar socket: a clinical immunohistological evaluation. Clin Oral Implants Res. 2016; 27:295–302.
Article30. Steigmann M. A bovine-bone mineral block for the treatment of severe ridge deficiencies in the anterior region: a clinical case report. Int J Oral Maxillofac Implants. 2008; 23:123–128.31. Hämmerle CH, Jung RE, Yaman D, Lang NP. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: a report of twelve consecutive cases. Clin Oral Implants Res. 2008; 19:19–25.
Article32. Felice P, Marchetti C, Piattelli A, Pellegrino G, Checchi V, Worthington H, et al. Vertical ridge augmentation of the atrophic posterior mandible with interpositional block grafts: bone from the iliac crest versus bovine anorganic bone. Eur J Oral Implantology. 2008; 1:183–198.33. Felice P, Piattelli A, Iezzi G, Degidi M, Marchetti C. Reconstruction of an atrophied posterior mandible with the inlay technique and inorganic bovine bone block: a case report. Int J Periodontics Restorative Dent. 2010; 30:583–591.34. Veis A, Dabarakis N, Koutrogiannis C, Barlas I, Petsa E, Romanos G. Evaluation of vertical bone regeneration using block and particulate forms of bio-oss bone graft: a histologic study in the rabbit mandible. J Oral Implantol. 2015; 41:e66–72.
Article35. Antunes AA, Grossi-Oliveira GA, Martins-Neto EC, Almeida AL, Salata LA. Treatment of circumferential defects with osseoconductive xenografts of different porosities: a histological, histometric, resonance frequency analysis, and micro-CT study in dogs. Clin Implant Dent Relat Res. 2015; 17:Suppl 1. e202–20.
Article36. Alberius P, Gordh M, Lindberg L, Johnell O. Onlay bone graft behaviour after marrow exposure of the recipient rat skull bone. Scand J Plast Reconstr Surg Hand Surg. 1996; 30:257–266.
Article37. Marins LV, Cestari TM, Sottovia AD, Granjeiro JM, Taga R. Radiographic and histological study of perennial bone defect repair in rat calvaria after treatment with blocks of porous bovine organic graft material. J Appl Oral Sci. 2004; 12:62–69.
Article38. Park JC, So SS, Jung IH, Yun JH, Choi SH, Cho KS, et al. Induction of bone formation by Escherichia coli-expressed recombinant human bone morphogenetic protein-2 using block-type macroporous biphasic calcium phosphate in orthotopic and ectopic rat models. J Periodontal Res. 2011; 46:682–690.
Article39. Alberius P, Gordh M. Osteopontin and bone sialoprotein distribution at the bone graft recipient site. Arch Otolaryngol Head Neck Surg. 1998; 124:1382–1386.
Article40. Murata M, Huang BZ, Shibata T, Imai S, Nagai N, Arisue M. Bone augmentation by recombinant human BMP-2 and collagen on adult rat parietal bone. Int J Oral Maxillofac Surg. 1999; 28:232–237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertical Ridge Augmentation with Mandibular Ramus Block Bone for Implant Surgery
- Vertical alveolar bone augmentation using thin block and chip bone graft technique : case report
- Clinical Study on the Alveolar Bone Repair Capacity of Dentin Matrix Block
- Acute Cutaneous Graft-Versus-Host Reaction
- SINUS GRAFT AND VERTICAL AUGMENTATION OF MAXILLARY POSTERIOR ALVEOLAR RIDGE USING MANDIBULAR RAMAL BLOCK BONE GRAFT