J Adv Prosthodont.
2016 Aug;8(4):304-312. 10.4047/jap.2016.8.4.304.
A two-short-implant-supported molar restoration in atrophic posterior maxilla: A finite element analysis
- Affiliations
-
- 1Department of Prosthodontics and Research Institute of Oral Science, College of Dentistry, Gangneung-Wonju National University, Gangneung, Republic of Korea. lila@gwnu.ac.kr
- 2Ye-Dental Clinic, Chuncheon, Republic of Korea.
- KMID: 2349339
- DOI: http://doi.org/10.4047/jap.2016.8.4.304
Abstract
- PURPOSE
The aim of this study was to investigate the stress distribution of 2-short implants (2SIs) installed in a severely atrophic maxillary molar site.
MATERIALS AND METHODS
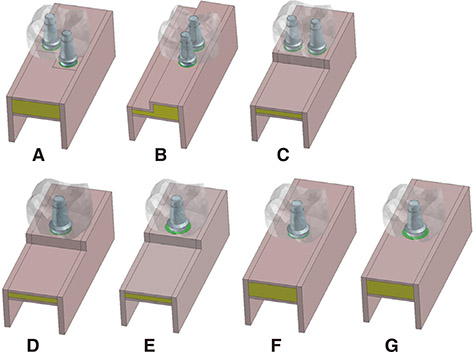
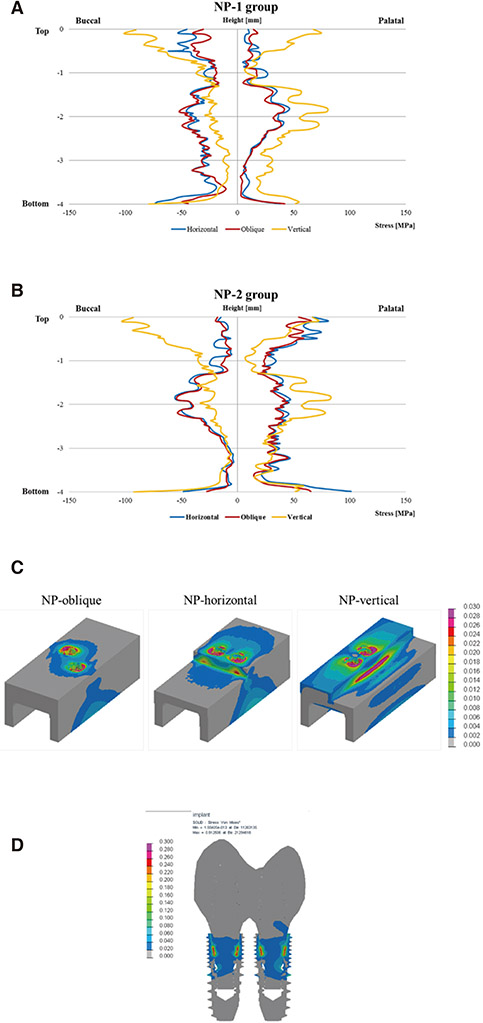
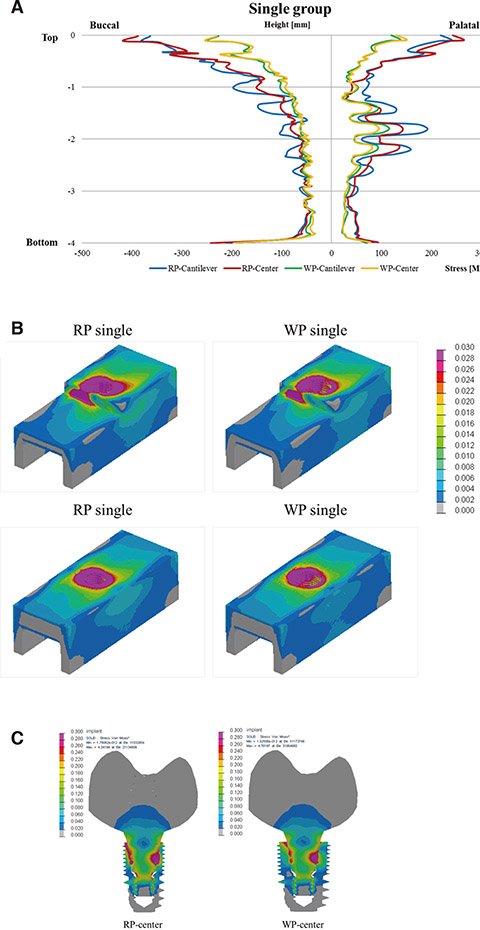
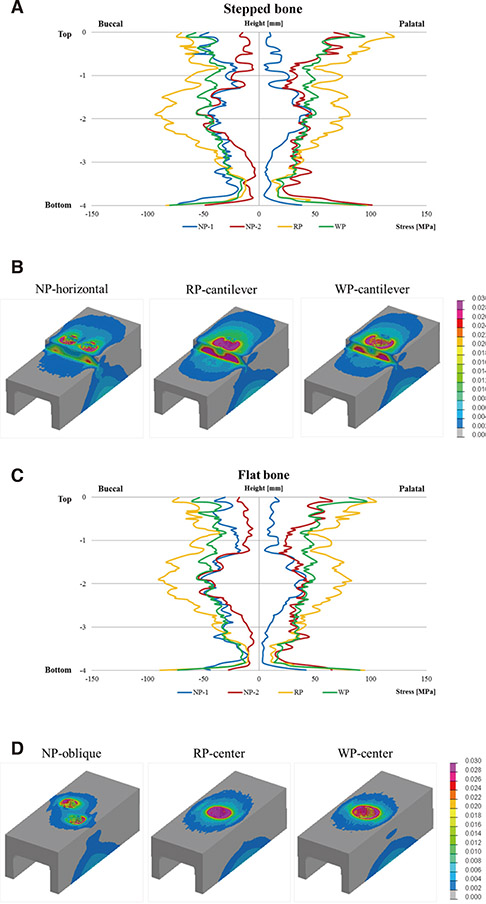
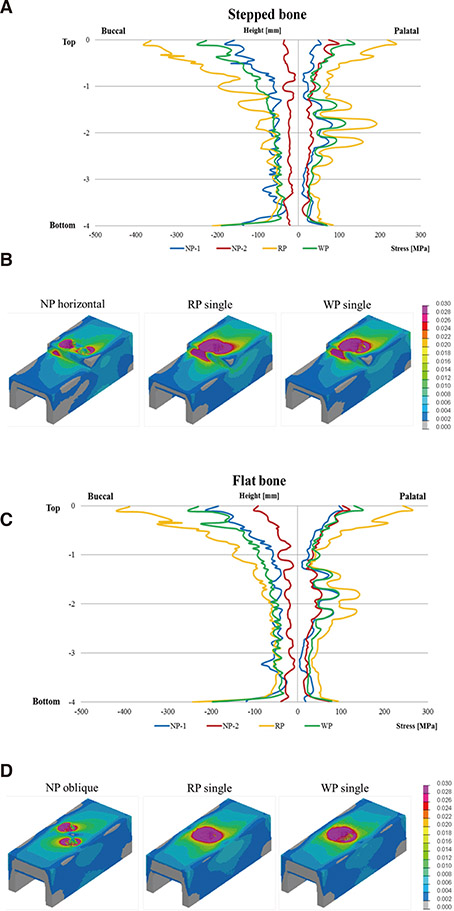
Three different diameters of internal connection implants were modeled: narrow platform (NP), regular platform (RP), and wide platform (WP). The maxillary first molars were restored with one implant or two short implants. Three 2SI models (NP-oblique, NP-vertical, and NP-horizontal) and four single implant models (RP and WP in a centered or cantilevered position) were used. Axial and oblique loadings were applied on the occlusal surface of the crown. The von Mises stress values were measured at the bone-implant, peri-implant bone, and implant/abutment complex.
RESULTS
The highest stress distribution at the bone-implant interface and the peri-implant bone was noticed in the RP group, and the lowest stress distribution was observed in the 2SI groups. Cantilevered position showed unfavorable stress distribution with axial loading. 2SI types did not affect the stress distribution in oblique loading. The number and installation positions of the implant, rather than the bone level, influenced the stress distribution of 2SIs. The implant/abutment complex of WP presented the highest stress concentration while that of 2SIs showed the lowest stress concentration.
CONCLUSION
2SIs may be useful for achieving stable stress distribution on the surrounding bone and implant-abutment complex in the atrophic posterior maxilla.
Figure
Cited by 1 articles
-
Stress distribution in premolars restored with inlays or onlays: 3D finite element analysis
Hongso Yang, Chan Park, Jin-Ho Shin, Kwi-Dug Yun, Hyun-Pil Lim, Sang-Won Park, Hyunju Chung
J Adv Prosthodont. 2018;10(3):184-190. doi: 10.4047/jap.2018.10.3.184.
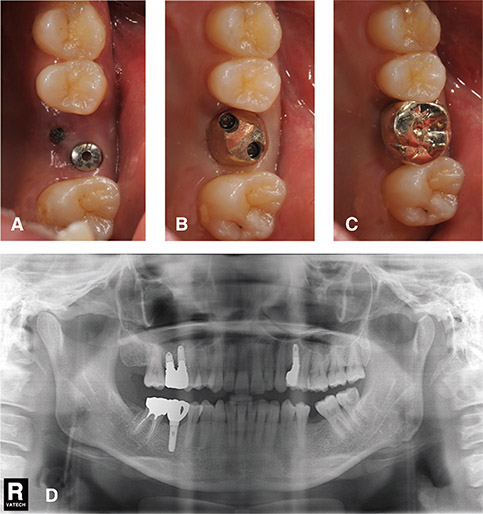
Reference
-
1. Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997; 8:161–172.2. Schwartz-Arad D, Laviv A, Levin L. Failure causes, timing, and cluster behavior: an 8-year study of dental implants. Implant Dent. 2008; 17:200–207.3. Kim SH, Kim SJ, Lee KW, Han DH. The effects of local factors on the survival of dental implants: A 19 year retrospective study. J Korean Acad Prosthodont. 2010; 48:28–40.4. Anderson DJ. Measurement of stress in mastication. I. J Dent Res. 1956; 35:664–670.5. Sakaguchi R, Powers J. Craig's restorative dental material. 13th ed. St Louis, MO: Mosby;2011. p. 60.6. Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998; 13:11–45.7. Wallace SS, Froum SJ, Cho SC, Elian N, Monteiro D, Kim BS, Tarnow DP. Sinus augmentation utilizing anorganic bovine bone (Bio-Oss) with absorbable and nonabsorbable membranes placed over the lateral window: histomorphometric and clinical analyses. Int J Periodontics Restorative Dent. 2005; 25:551–559.8. Rosen PS, Summers R, Mellado JR, Salkin LM, Shanaman RH, Marks MH, Fugazzotto PA. The bone-added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants. 1999; 14:853–858.9. Akça K, Cehreli MC, Iplikçioglu H. A comparison of three-dimensional finite element stress analysis with in vitro strain gauge measurements on dental implants. Int J Prosthodont. 2002; 15:115–121.10. Ryu HS, Kim SJ, Park EJ, Kim MR. A retrospective study of the cumulative survival rate and change of peri-implant marginal bone around implants associated with maxillary sinus augmentation. J Korean Acad Prosthodont. 2009; 47:240–246.11. Lazzara RJ. The sinus elevation procedure in endosseous implant therapy. Curr Opin Periodontol. 1996; 3:178–183.12. Winter AA, Pollack AS, Odrich RB. Placement of implants in the severely atrophic posterior maxilla using localized management of the sinus floor: a preliminary study. Int J Oral Maxillofac Implants. 2002; 17:687–695.13. Friberg B, Gröndahl K, Lekholm U, Brånemark PI. Long-term follow-up of severely atrophic edentulous mandibles reconstructed with short Brånemark implants. Clin Implant Dent Relat Res. 2000; 2:184–189.14. das Neves FD, Fones D, Bernardes SR, do Prado CJ, Neto AJ. Short implants-an analysis of longitudinal studies. Int J Oral Maxillofac Implants. 2006; 21:86–93.15. Tawil G, Younan R. Clinical evaluation of short, machined-surface implants followed for 12 to 92 months. Int J Oral Maxillofac Implants. 2003; 18:894–901.16. Fugazzotto PA. Shorter implants in clinical practice: rationale and treatment results. Int J Oral Maxillofac Implants. 2008; 23:487–496.17. Thor A, Sennerby L, Hirsch JM, Rasmusson L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: an evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg. 2007; 65:64–72.18. Bahat O. Treatment planning and placement of implants in the posterior maxillae: report of 732 consecutive Nobelpharma implants. Int J Oral Maxillofac Implants. 1993; 8:151–161.19. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003; 5:254–262.20. Lum LB. A biomechanical rationale for the use of short implants. J Oral Implantol. 1991; 17:126–131.21. Sato Y, Shindoi N, Hosokawa R, Tsuga K, Akagawa Y. Biomechanical effects of double or wide implants for single molar replacement in the posterior mandibular region. J Oral Rehabil. 2000; 27:842–845.22. Griffin TJ, Cheung WS. The use of short, wide implants in posterior areas with reduced bone height: a retrospective investigation. J Prosthet Dent. 2004; 92:139–144.23. Balshi TJ, Wolfinger GJ. Two-implant-supported single molar replacement: interdental space requirements and comparison to alternative options. Int J Periodontics Restorative Dent. 1997; 17:426–435.24. Song HY, Heo YH, Park CJ, Cho LR. Two-short implant supported single molar restoration in atrophic posterior maxilla : a clinical study. J Korean Dent Assoc. 2015; 53:628–643.25. Collings E. The physical metallurgy of titanium alloys. American Society for Metals. Ohio: Metals Park;1984.26. Pessoa RS, Vaz LG, Marcantonio E Jr, Vander Sloten J, Duyck J, Jaecques SV. Biomechanical evaluation of platform switching in different implant protocols: computed tomography-based three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2010; 25:911–919.27. Rangert B, Jemt T, Jörneus L. Forces and moments on Branemark implants. Int J Oral Maxillofac Implants. 1989; 4:241–247.28. Cağlar A, Aydin C, Ozen J, Yilmaz C, Korkmaz T. Effects of mesiodistal inclination of implants on stress distribution in implant-supported fixed prostheses. Int J Oral Maxillofac Implants. 2006; 21:36–44.29. Cha HS, Kim YS, Jeon JH, Lee JH. Cumulative survival rate and complication rates of single-tooth implant; focused on the coronal fracture of fixture in the internal connection implant. J Oral Rehabil. 2013; 40:595–602.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of reliability of zirconia materials to be used in implant-retained restoration on the atrophic bone of the posterior maxilla: A finite element study
- Finite element analysis of the effect of cantilever and implant orientation on stress distribution in a mandibular implant-supported bar overdenture
- Three-dimensional finite element stress analysis of single implant restoration using different fixture and abutment screw diameters
- The effects of posterior retraction on the displacement of the maxilla
- A finite element analysis on the 3-unit fixed prosthesis supported with a natural tooth and angle variable implant