J Korean Ophthalmol Soc.
2016 Aug;57(8):1333-1338. 10.3341/jkos.2016.57.8.1333.
A Case of Wyburn-Mason Syndrome with Facial Nevus Flammeus and the Associated Optical Coherence Tomography Findings
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. drahn323@gmail.com
- 2Department of Ophthalmology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea.
- KMID: 2349086
- DOI: http://doi.org/10.3341/jkos.2016.57.8.1333
Abstract
- PURPOSE
To describe a case of Wyburn-Mason Syndrome, which is a rare phakomatosis, and its associated optical coherence tomography findings.
CASE SUMMARY
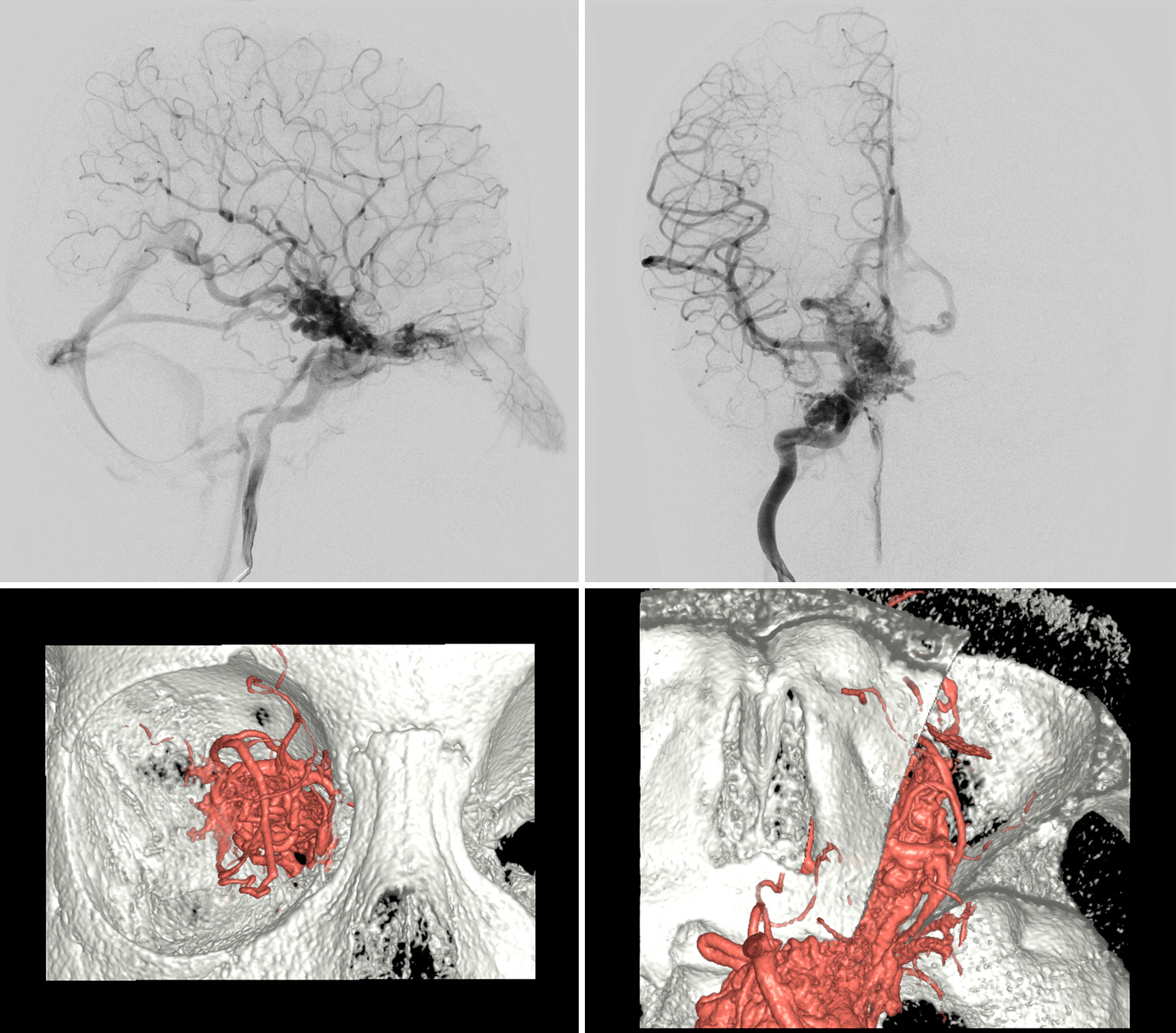
A 5-year-old boy was referred to our clinic for decreased vision in his right eye. He had nevus flammeus on his right forehead, upper eyelid, and cheek. His best corrected visual acuity was hand motion in the right eye, in which a relative afferent pupillary defect was noted. Fundus examination of the right eye showed marked dilation and tortuosity of retinal vessels, which could not be discriminated between arteries and veins on the posterior pole. Optical coherence tomography showed multiple large intraretinal vessels without involvement of the internal limiting membrane. Cerebral angiography revealed arteriovenous malformations (AVMs) and feeder vessels from the internal carotid artery to the ophthalmic artery, extending to the ethmoidal artery in the nasal cavity.
CONCLUSIONS
Wyburn-Mason syndrome is a rare phakomatoses and shows unique retinal AVM. Misdiagnosis or undertreatment of Wyburn-Mason syndrome can lead to serious complications. Patients with facial nevus flammeus should undergo thorough ocular examinations to rule out this disorder. Optical coherence tomography is a useful method for understanding structural features of retinal vascular malformations in Wyburn-Mason syndrome.
Keyword
MeSH Terms
-
Arteries
Arteriovenous Malformations
Carotid Artery, Internal
Cerebral Angiography
Cheek
Child, Preschool
Diagnostic Errors
Eyelids
Forehead
Hand
Humans
Male
Membranes
Methods
Nasal Cavity
Neurocutaneous Syndromes
Nevus*
Ophthalmic Artery
Port-Wine Stain*
Pupil Disorders
Retinal Vessels
Retinaldehyde
Tomography, Optical Coherence*
Vascular Malformations
Veins
Visual Acuity
Retinaldehyde
Figure
Reference
-
References
1. Wyburn-Mason R. Arteriovenous aneurysm of midbrain and abdominal, facial naevi and mental changes. Brain. 1943; 66:163–203.2. Chowaniec MJ, Suh DW, Boldt HC, et al. Anomalous optical abdominal tomography findings in Wyburn-Mason syndrome and isolated retinal arteriovenous malformation. J AAPOS. 2015; 19:175–7.3. Bae HD, Kim BH, Shin DM. A case of congenital arteriovenous communications of the retina. J Korean Ophthalmol Soc. 1981; 22:647–51.4. Joo JD, Lee JH. A case of bilateral congenital arteriovenous communication. J Korean Ophthalmol Soc. 1996; 37:1218–23.5. Jang HS, Lee TK, Kim JW. A case of retinal racemose hemangioma. J Korean Ophthalmol Soc. 2001; 42:1232–5.6. Shin CH, Lee SN. Wyburn-Mason syndrome: a case report. J Korean Ophthalmol Soc. 2010; 51:145–9.
Article7. Schmidt D, Pache M, Schumacher M. The congenital unilateral abdominal vascular malformation syndrome (bonnet-dechaumeblanc syndrome or wyburn-mason syndrome): review of the literature. Surv Ophthalmol. 2008; 53:227–49.8. Iwata A, Mitamura Y, Niki M, et al. Binarization of enhanced depth imaging optical coherence tomographic images of an eye with Wyburn-Mason syndrome: a case report. BMC Ophthalmol. 2015; 15:19.
Article9. Ponce FA, Han PP, Spetzler RF, et al. Associated arteriovenous malformation of the orbit and brain: a case of Wyburn-Mason abdominal without retinal involvement. Case report. J Neurosurg. 2001; 95:346–9.10. Magnus H. Aneurysma arterioso-venosum retinale. Virchows Arch Pathol Anat Physiol Klin Med. 1874; 60:38–45.
Article11. Bonnet P, Dechaume J, Blanc M. L'aneurisme cirsoide de la retine (aneurysme racemeux). J Med Lyon. 1937; 18:165–78.12. Bech K, Jensen OA. On the frequency of abdominal racemose hae-mangiomata of the retina and brain. Acta Psychiatr Scand. 1961; 36:47–56.13. Théron J, Newton TH, Hoyt WF. Unilateral retinocephalic vascular malformations. Neuroradiology. 1974; 7:185–96.
Article14. Dayani PN, Sadun AA. A case report of Wyburn-Mason syndrome and review of the literature. Neuroradiology. 2007; 49:445–56.
Article15. Wilkins RH. Natural history of intracranial vascular malformations: a review. Neurosurgery. 1985; 16:421–30.
Article16. Ondra SL, Troupp H, George ED, Schwab K. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg. 1990; 73:387–91.
Article17. Brown RD Jr, Wiebers DO, Forbes G, et al. The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg. 1988; 68:352–7.
Article18. Grigg JRB, Jamieson RV. Phakomatoses. Hoyt CS, Taylor D, editors. Pediatric Ophthalmology and Strabismus. 4th ed.New York: Elsevier;2013. chap. 65.
Article19. Telander DG, Choi SS, Zawadzki RJ, et al. Microstructural abdominal revealed by high resolution imaging systems in central macular arteriovenous malformation. Ophthalmic Surg Lasers Imaging. 2010; 9:1–4.20. Onder HI, Alisan S, Tunc M. Serous retinal detachment and abdominal macular edema in a patient with Wyburn-Mason syndrome. Semin Ophthalmol. 2015; 30:154–6.21. Rizzo R, Pavone L, Pero G, et al. A neurocutaneous disorder with a severe course: Wyburn-Mason's syndrome. J Child Neurol. 2004; 19:908–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wyburn-Mason Syndrome: A Case Report
- Phakomatosis Pigmentovascularis Type Ia
- Clinical Experience of Treatment in a Case of Sturge-Weber Syndrome with Bilateral Glaucoma
- A Case of Angioma Serpiginosum Accompanied with Ipsilateral Nevus Flammeus on the Hand
- A Case of Phakomatosis Pigmentovascularis with Eye Involvement