J Korean Ophthalmol Soc.
2016 Aug;57(8):1210-1215. 10.3341/jkos.2016.57.8.1210.
Measurement of Ophthalmic-arterial Blood-flow Velocity Using Transcranial Doppler Ultrasonography in Patients with Central Serous Chorioretinopathy
- Affiliations
-
- 1Department of Ophthalmology, Sahmyook Medical Center, Seoul, Korea. ymedi@hanmail.net
- KMID: 2349065
- DOI: http://doi.org/10.3341/jkos.2016.57.8.1210
Abstract
- PURPOSE
To measure and compare the ocular blood-flow velocity of ophthalmic artery in patients with central serous chorioretinopathy (CSC); affected eyes, asymptomatic fellow eyes, and CSC resolved eyes using transcranial Doppler ultrasonography.
METHODS
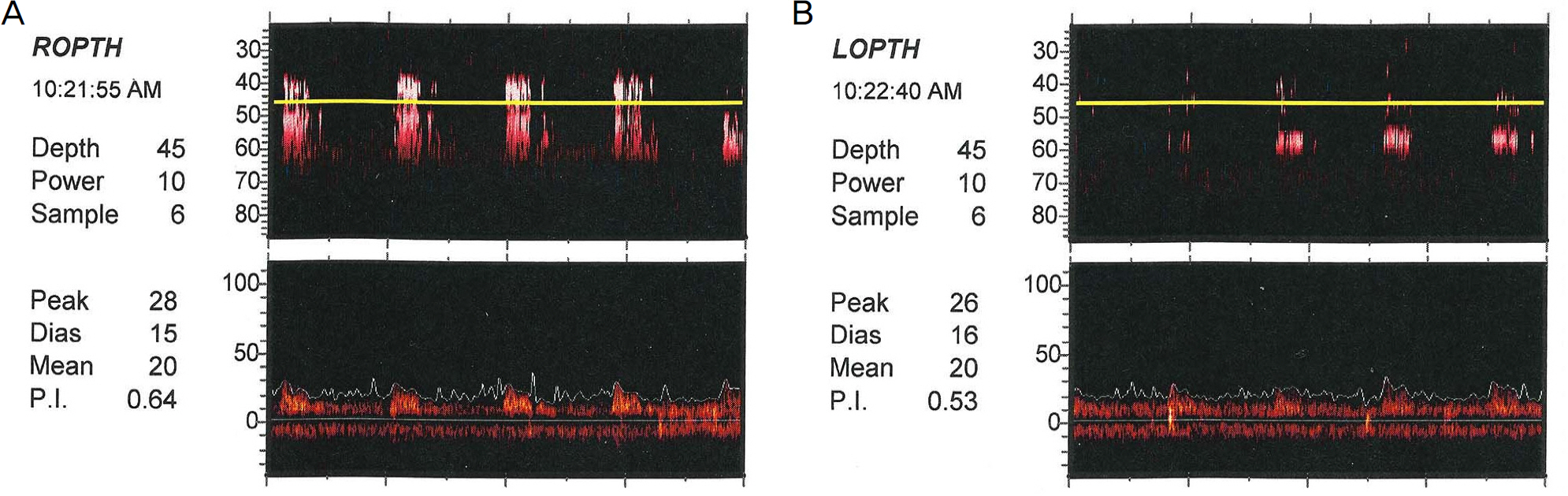
A total of 31 patients (age 20-52 years) with CSC were evaluated using power motion mode Doppler 150 digital transcranial Doppler ultrasonography. The peak systolic velocity (PSV), peak diastolic velocity (PDV), and resistance index (RI) were measured in the ophthalmic artery of both affected and asymptomatic fellow eyes. After 2 months, 23 patients with resolved serous retinal detachment underwent repeated measurement of the above hemodynamic indices.
RESULTS
The PSV and PDV of the ophthalmic artery were 30.05 ± 5.34 cm/sec and 14.07 ± 2.90 cm/sec in affected eyes and 33.03 ± 2.00 cm/sec and 17.17 ± 2.76 cm/sec in asymptomatic fellow eyes, respectively. Both indices were significantly lower in affected eyes (p = 0.004, p < 0.001, respectively). The RI was 0.52 ± 0.08 in affected eyes and 0.43 ± 0.04 in fellow eyes, a significant difference (p < 0.001). After 2 months, in 23 eyes with resolved CSC, the PSV and PDV were 32.94 ± 6.24 cm/sec and 15.54 ± 2.88 cm/sec, respectively. Both indices were significantly higher than at baseline (p = 0.031, p = 0.045, respectively). However, RI was 0.48 ± 0.04 and was not significantly different (p = 0.073).
CONCLUSIONS
The CSC-affected eyes showed lower ocular blood-flow velocity and higher RI than the asymptomatic fellow eyes. The ocular blood-flow velocity was increased as CSC was resolved. These findings provide insights into the ophthalmic arterial vascular factors related to the pathogenesis of CSC.
MeSH Terms
Figure
Reference
-
References
1. Von Graefe A. Ueber centrale recidivierende retinitis. Graefes Arch Clin Exp Ophthalmol. 1866; 12:211–5.2. Donald J, Gass M. Pathogenesis of disciform detachment of the neuroepithelium: II. Idiopathic central serous choroidopathy. Am J Ophthalmol. 1967; 63:587–15.3. Gelber GS, Schatz H. Loss of vision due to central serous abdominal following psychological stress. Am J Psychiatry. 1987; 144:46–50.4. Yannuzzi LA. Type-A behavior and central serous chorioretinopathy. Retina. 1987; 7:111–31.
Article5. Yap EY, Robertson DM. The long-term outcome of central serous chorioretinopathy. Arch Ophthalmol. 1996; 114:689–92.
Article6. Scheider A, Nasemann JE, Lund OE. Fluorescein and indocyanine green angiographies of central serous choroidopathy by scanning laser ophthalmoscopy. Am J Ophthalmol. 1993; 115:50–6.
Article7. Kitaya N, Nagaoka T, Hikichi T, et al. Features of abnormal abdominal circulation in central serous chorioretinopathy. Br J Ophthalmol. 2003; 87:709–12.8. Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982; 57:769–74.
Article9. Chen Q, Haeri S, Van Veen T, et al. Power M-mode transcranial Doppler examination of the ophthalmic artery in pregnancy: abdominal operating procedure and review of the literature. J Ultrasound Med. 2013; 32:1671–5.10. Erickson SJ, Hendrix LE, Massaro BM, et al. Color Doppler flow imaging of the normal and abnormal orbit. Radiology. 1989; 173:511–6.
Article11. Kim YY, Huh K, Lee TS. Color Doppler imaging in diagnose abdominal disorders. J Korean Ophthalmol Soc. 1999; 40:261–6.12. Youn JW, Lee HB, Lee KW, Youn DH. The measurement of ocular blood flow velocity using Doppler ultrasound in primary open angle glaucoma and ocular hypertension patents. J Korean Ophthalmol Soc. 1994; 35:1651–6.13. Hamidi C, Türkcü FM, Göya C, et al. Evaluation of retrobulbar blood flow with color doppler ultrasonography in patients with central serous chorioretinopathy. J Clin Ultrasound. 2014; 42:481–5.
Article14. Gass JD. Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol. 1967; 63(Suppl):1–139.15. Spitznas M. Pathogenesis of central serous retinopathy: a new working hypothesis. Graefes Arch Clin Exp Ophthalmol. 1986; 224:321–4.
Article16. Iida T, Kishi S, Hagimura N, Shimizu K. Persistent and bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina. 1999; 19:508–12.
Article17. Spaide RF, Hall L, Haas A, et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 1996; 16:203–13.
Article18. Bujarborua D, Chatterjee S, Choudhury A, et al. Fluorescein abdominal features of asymptomatic eyes in central serous chorioretinopathy. Retina. 2005; 25:422–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Measurement of Blood Flow Velocity of Ophthalmic and Central Retinal Artery using Color Doppler Imaging
- Transcranial Doppler Measurement of Intracraial Arterial Flow Velocity in Subarachnoid Hemorrhage
- Effect of Calculation Task on the Regional Cerebral Blood Flow Velocity: a Transcranial Doppler Study
- Role of Transcranial Doppler Study in the Patients with Ruptured Cerebral Aneurysm
- Diagnostic Values of Transcranial Doppler Ultrasound Detecting High-grade Carotid Stenosis