J Korean Orthop Assoc.
2016 Aug;51(4):345-349. 10.4055/jkoa.2016.51.4.345.
Neurolymphomatosis Involving Antebrachial Cutaneous Nerve
- Affiliations
-
- 1Department of Orthopedic Surgery, Bundang Jesaeng General Hospital, Seongnam, Korea. ncd1896@naver.com
- 2Department of Pathology, Bundang Jesaeng General Hospital, Seongnam, Korea.
- KMID: 2348642
- DOI: http://doi.org/10.4055/jkoa.2016.51.4.345
Abstract
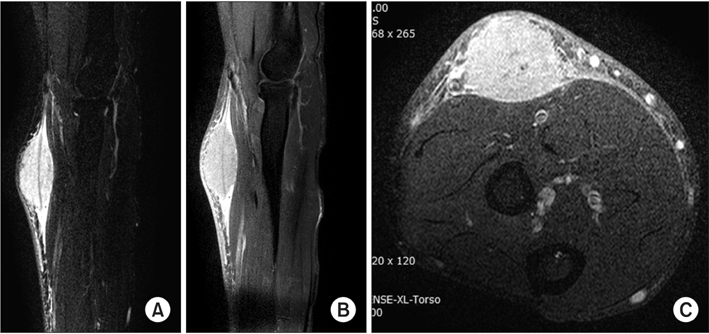
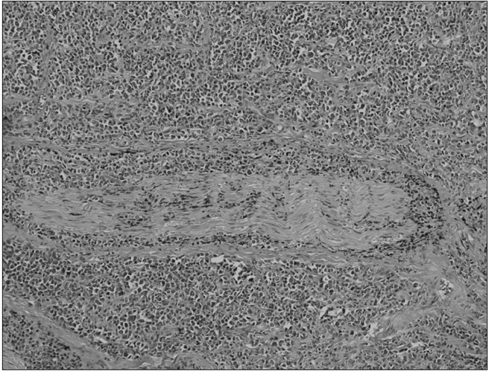
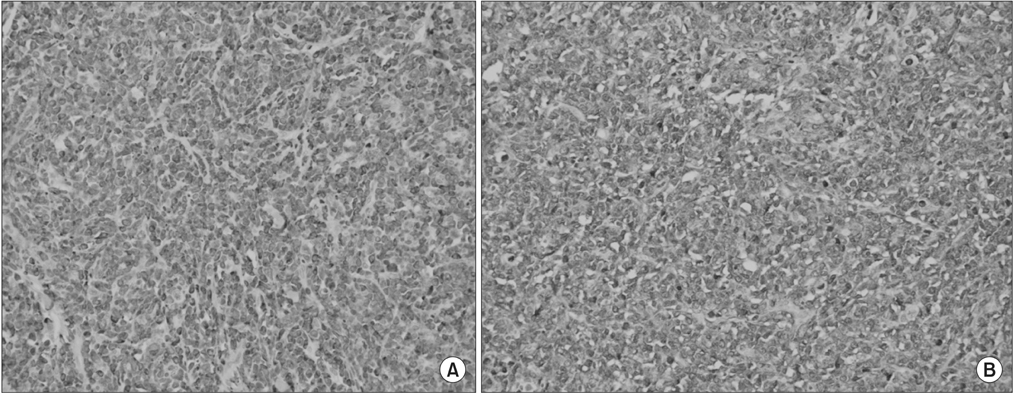
- The term neurolymphomatosis has included infiltration of the peripheral nervous system by lymphoma. In generally, direct invasion of the peripheral nervous system is rare. The difficulty in treatment of neurolymphomatosis is due to unclassified characteristic symptoms and diagnosis. We performed excision of mass on the antebrachial cutaneous nerve with no specific symptoms. After diagnosis of diffuse large B cell lymphoma, further treatment and observation were followed. However, recurrence of the lymphoma was found in the ipsilateral forearm ulnar nerve, therefore we described a case of neurolymphomatosis with a brief review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Baehring JM, Damek D, Martin EC, Betensky RA, Hochberg FH. Neurolymphomatosis. Neuro Oncol. 2003; 5:104–115.
Article2. Currie S, Henson RA. Neurological syndromes in the reticuloses. Brain. 1971; 94:307–320.
Article3. Richmond J, Sherman RS, Diamond HD, Craver LF. Renal lesions associated with malignant lymphomas. Am J Med. 1962; 32:184–207.
Article4. Teissier J. Primary malignant lymphoma localized in the trunk of the ulnar nerve at the elbow. A case report. Ann Chir Main Memb Super. 1992; 11:170–172.5. Gonzalvo A, McKenzie C, Harris M, Biggs M. Primary non-Hodgkin's lymphoma of the radial nerve: case report. Neurosurgery. 2010; 67:E872–E873.6. Gan HK, Azad A, Cher L, Mitchell PL. Neurolymphomatosis: diagnosis, management, and outcomes in patients treated with rituximab. Neuro Oncol. 2010; 12:212–215.
Article7. Byun WM, Park WK, Park BH, Ahn SH, Hwang MS, Chang JC. Guillain-Barré syndrome: MR imaging findings of the spine in eight patients. Radiology. 1998; 208:137–141.
Article8. Lin M, Kilanowska J, Taper J, Chu J. Neurolymphomatosis: diagnosis and assessment of treatment response by FDG PET-CT. Hematol Oncol. 2008; 26:43–45.9. Salm LP, Van der Hiel B, Stokkel MP. Increasing importance of 18F-FDG PET in the diagnosis of neurolymphomatosis. Nucl Med Commun. 2012; 33:907–916.
Article10. Habermann TM, Weller EA, Morrison VA, et al. Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol. 2006; 24:3121–3127.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomical Distribution of Branches of the Medial Antebrachial Cutaneous Nerve during Cubital Tunnel Surgery
- Neurolymphomatosis Involving Sciatic Nerve: A Case Report
- Neurilemmoma of the Tibial Nerve and Lateral Antebrachial Cutaneous nerve: Case Report
- Lumbosacral plexopathy due to neurolymphomatosis superimposed on traumatic nerve injury
- A Case of Neurolymphomatosis Involving Cranial Nerve Diagnosed by PET-CT Imaging