Yonsei Med J.
2015 Nov;56(6):1566-1571. 10.3349/ymj.2015.56.6.1566.
Does Sedation Affect Examination of Esophagogastric Junction during Upper Endoscopy?
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. sklee@yuhs.ac
- 2Biostatistics Collaboration Unit, Yonsei University, Seoul, Korea.
- KMID: 2345884
- DOI: http://doi.org/10.3349/ymj.2015.56.6.1566
Abstract
- PURPOSE
During sedated esophagogastroduodenoscopy (EGD), patients may not be able to perform inspiration, which is necessary to examine the esophagogastric junction. Therefore sedation may affect diagnosis of gastroesophageal reflux-related findings. The aim of our study was to investigate the effect of sedation on diagnosis of gastroesophageal reflux-related findings during EGD.
MATERIALS AND METHODS
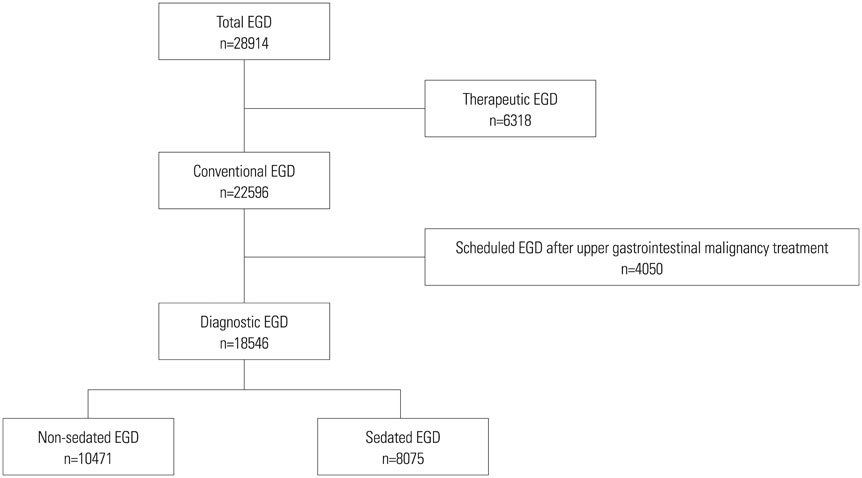
This retrospective study evaluated 28914 patients older than 20 years who underwent EGD at our institution between January 2011 and December 2011. Ultimately, 1546 patients indicated for EGD for health check-up and symptom evaluation were included.
RESULTS
There were 18546 patients who had diagnostic EGD: 10471 patients (56%) by non-sedated EGD and 8075 patients (43%) by sedated EGD. After statistical adjustment for age, sex, and body mass index, minimal change esophagitis, and hiatal hernia were significantly less frequently observed in the sedated EGD group [odds ratio (OR), 0.651; 95% confidence interval (CI), 0.586 to 0.722 and OR, 0.699; 95% CI, 0.564 to 0.866]. Nevertheless, there was no significant difference in other findings at the gastroesophageal junction, such as reflux esophagitis with Los Angeles classification A, B, C, and D or Barrett's esophagus, between the two groups. Similarly, there were no differences in early gastric cancer, advanced gastric cancer, and gastric ulcer occurrence.
CONCLUSION
Sedation can impede the detection of minimal change esophagitis and hiatal hernia, but does not influence detection of reflux esophagitis of definite severity and Barrett's esophagus.
MeSH Terms
Figure
Reference
-
1. Goh KL, Chang CS, Fock KM, Ke M, Park HJ, Lam SK. Gastro-oesophageal reflux disease in Asia. J Gastroenterol Hepatol. 2000; 15:230–238.
Article2. Inamori M, Togawa J, Nagase H, Abe Y, Umezawa T, Nakajima A, et al. Clinical characteristics of Japanese reflux esophagitis patients as determined by Los Angeles classification. J Gastroenterol Hepatol. 2003; 18:172–176.
Article3. Rosaida MS, Goh KL. Gastro-oesophageal reflux disease, reflux oesophagitis and non-erosive reflux disease in a multiracial Asian population: a prospective, endoscopy based study. Eur J Gastroenterol Hepatol. 2004; 16:495–501.
Article4. Shim KN, Hong SJ, Sung JK, Park KS, Kim SE, Park HS, et al. Clinical spectrum of reflux esophagitis among 25,536 Koreans who underwent a health check-up: a nationwide multicenter prospective, endoscopy-based study. J Clin Gastroenterol. 2009; 43:632–638.
Article5. Thomson A, Andrew G, Jones DB. Optimal sedation for gastrointestinal endoscopy: review and recommendations. J Gastroenterol Hepatol. 2010; 25:469–478.
Article6. Standards of Practice Committee. Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008; 68:205–216.
Article7. Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Methods of granting hospital privileges to perform gastrointestinal endoscopy. Gastrointest Endosc. 2002; 55:780–783.
Article8. Horiuchi A, Nakayama Y, Hidaka N, Ichise Y, Kajiyama M, Tanaka N. Low-dose propofol sedation for diagnostic esophagogastroduodenoscopy: results in 10,662 adults. Am J Gastroenterol. 2009; 104:1650–1655.
Article9. Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996; 111:85–92.
Article10. Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006; 41:95–99.
Article11. Kim JH, Park H, Lee YC. MIGHT study group. Is minimal change esophagitis really part of the spectrum of endoscopic findings of gastroesophageal reflux disease? A prospective, multicenter study. Endoscopy. 2011; 43:190–195.
Article12. Block B. Endoscopy of the upper GI tract. New York, NY: Thieme Medical Publishers, Incorporated.;2004. p. 32–33.13. de Leon A, Ahlstrand R, Thörn SE, Wattwil M. Effects of propofol on oesophageal sphincters: a study on young and elderly volunteers using high-resolution solid-state manometry. Eur J Anaesthesiol. 2011; 28:273–278.
Article14. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45:172–180.
Article15. Chang CS, Poon SK, Lien HC, Chen GH. The incidence of reflux esophagitis among the Chinese. Am J Gastroenterol. 1997; 92:668–671.16. Watanabe T, Urita Y, Sugimoto M, Miki K. Gastroesophageal reflux disease symptoms are more common in general practice in Japan. World J Gastroenterol. 2007; 13:4219–4223.
Article17. Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008; 27:173–185.
Article18. Kim KM, Cho YK, Bae SJ, Kim DS, Shim KN, Kim JH, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012; 27:741–745.
Article19. Lee SJ, Song CW, Jeen YT, Chun HJ, Lee HS, Um SH, et al. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001; 16:373–376.
Article20. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005; 54:710–717.
Article21. Kim JH, Rhee PL, Lee JH, Lee H, Choi YS, Son HJ, et al. Prevalence and risk factors of Barrett's esophagus in Korea. J Gastroenterol Hepatol. 2007; 22:908–912.
Article22. Tseng PH, Lee YC, Chiu HM, Huang SP, Liao WC, Chen CC, et al. Prevalence and clinical characteristics of Barrett's esophagus in a Chinese general population. J Clin Gastroenterol. 2008; 42:1074–1079.
Article23. Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut Liver. 2011; 5:267–277.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypotonic Upper Esophageal Sphincter With Functional Esophagogastric Junction Obstruction in a Patient With Oropharyngeal and Esophageal Dysphagia
- A Case of Multiple Gastric Diverticula
- A Case of Early Adenocarcinoma at Esophagogastric Junction Treated with Cap-pitted Endoscopic Mucosal Resection
- Current and Future Use of Esophageal Capsule Endoscopy
- Acute Anisakiasis at the Esophagogastric Junction Mimicking Angina Pectoris