Korean Circ J.
2016 Mar;46(2):117-134. 10.4070/kcj.2016.46.2.117.
Heart Disease in Disorders of Muscle, Neuromuscular Transmission, and the Nerves
- Affiliations
-
- 1Krankenanstalt Rudolfstiftung, Vienna, Austria. fifigs1@yahoo.de
- 22nd Medical Department with Cardiology and Intensive Care Medicine, Krankenanstalt Rudolfstiftung, Vienna, Austria.
- KMID: 2344462
- DOI: http://doi.org/10.4070/kcj.2016.46.2.117
Abstract
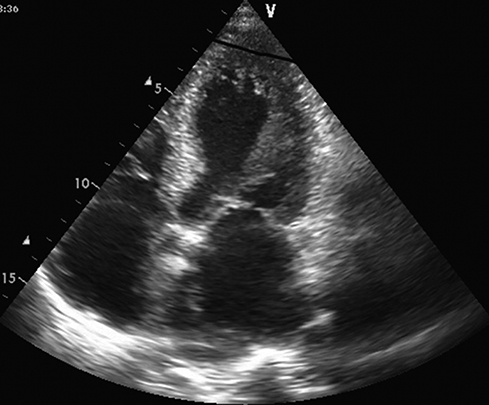
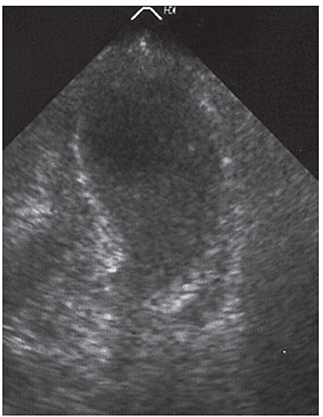
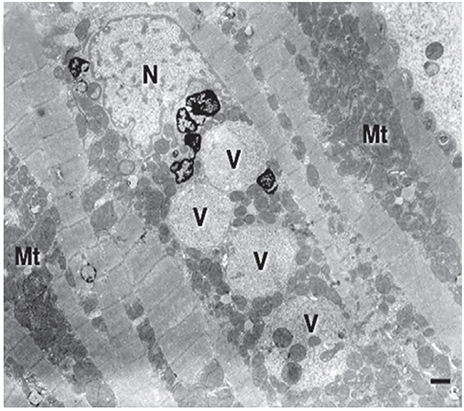
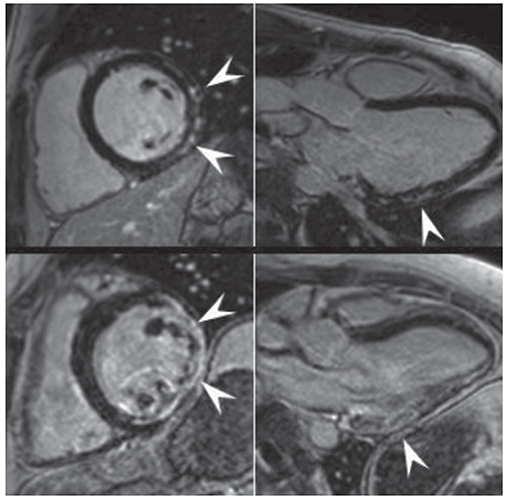
- Little is known regarding cardiac involvement (CI) by neuromuscular disorders (NMDs). The purpose of this review is to summarise and discuss the major findings concerning the types, frequency, and severity of cardiac disorders in NMDs as well as their diagnosis, treatment, and overall outcome. CI in NMDs is characterized by pathologic involvement of the myocardium or cardiac conduction system. Less commonly, additional critical anatomic structures, such as the valves, coronary arteries, endocardium, pericardium, and even the aortic root may be involved. Involvement of the myocardium manifests most frequently as hypertrophic or dilated cardiomyopathy and less frequently as restrictive cardiomyopathy, non-compaction, arrhythmogenic right-ventricular dysplasia, or Takotsubo-syndrome. Cardiac conduction defects and supraventricular and ventricular arrhythmias are common cardiac manifestations of NMDs. Arrhythmias may evolve into life-threatening ventricular tachycardias, asystole, or even sudden cardiac death. CI is common and carries great prognostic significance on the outcome of dystrophinopathies, laminopathies, desminopathies, nemaline myopathy, myotonias, metabolic myopathies, Danon disease, and Barth-syndrome. The diagnosis and treatment of CI in NMDs follows established guidelines for the management of cardiac disease, but cardiotoxic medications should be avoided. CI in NMDs is relatively common and requires complete work-up following the establishment of a neurological diagnosis. Appropriate cardiac treatment significantly improves the overall long-term outcome of NMDs.
MeSH Terms
-
Arrhythmias, Cardiac
Cardiomyopathies
Cardiomyopathy, Dilated
Cardiomyopathy, Restrictive
Coronary Vessels
Death, Sudden, Cardiac
Diagnosis
Endocardium
Glycogen Storage Disease Type IIb
Heart Arrest
Heart Diseases*
Heart*
Muscular Diseases
Myocardium
Myopathies, Nemaline
Myotonia
Neuromuscular Diseases
Pericardium
Tachycardia, Ventricular
Figure
Reference
-
1. Rubin HJ, Lowbeer L. Progressive muscular dystrophy with involvement of heart muscle. Proc Staff Meet Tulsa Okla Hillcrest Meml Hosp. 1947; 4:141–156.2. Coelho E. Heart changes in the familial type of paramyloidosis with peripheral neuropathy. Z Kreislaufforsch. 1963; 52:1066–1078.3. Hertzman PA, Maddoux GL, Sternberg EM, et al. Repeated coronary artery spasm in a young woman with the eosinophilia-myalgia syndrome. JAMA. 1992; 267:2932–2934.4. Rakocević-Stojanović V, Pavlović S, Seferović P, et al. Pathohistological changes in endomyocardial biopsy specimens in patients with myotonic dystrophy. Panminerva Med. 1999; 41:27–30.5. Palladino A, Passamano L, Taglia A, et al. Cardiac involvement in patients with spinal muscular atrophies. Acta Myol. 2011; 30:175–178.6. Yasuma F, Kuru S, Konagaya M. Dilated cardiomyopathy in Kugelberg-Welander disease: coexisting sleep disordered breathing and its treatment with continuous positive airway pressure. Intern Med. 2004; 43:951–954.7. Elkohen M, Vaksmann G, Elkohen MR, Francart C, Foucher C, Rey C. Cardiac involvement in Kugelberg-Welander disease. A prospective study of 8 cases. Arch Mal Coeur Vaiss. 1996; 89:611–617.8. Iwahara N, Hisahara S, Hayashi T, Kawamata J, Shimohama S. A novel lamin A/C gene mutation causing spinal muscular atrophy phenotype with cardiac involvement: report of one case. BMC Neurol. 2015; 15:13.9. Namazi MH, Khaheshi I, Haybar H, Esmaeeli S. Cardiac failure as an unusual presentation in a patient with history of amyotrophic lateral sclerosis. Case Rep Neurol Med. 2014; 2014:986139.10. Tanaka Y, Yamada M, Koumura A, et al. Cardiac sympathetic function in the patients with amyotrophic lateral sclerosis: analysis using cardiac [123I] MIBG scintigraphy. J Neurol. 2013; 260:2380–2386.11. Shemisa K, Kaelber D, Parikh SA, Mackall JA. Autonomic etiology of heart block in amyotrophic lateral sclerosis: a case report. J Med Case Rep. 2014; 8:224.12. Massari FM, Tonella T, Tarsia P, Kirani S, Blasi F, Magrini F. Tako-tsubo syndrome in a young man with amyotrophic lateral sclerosis. A case report. G Ital Cardiol (Rome). 2011; 12:388–391.13. Araki A, Katsuno M, Suzuki K, et al. Brugada syndrome in spinal and bulbar muscular atrophy. Neurology. 2014; 82:1813–1821.14. Sakpichaisakul K, Taeranawich P, Nitiapinyasakul A, Sirisopikun T. Identification of Sandhoff disease in a Thai family: clinical and biochemical characterization. J Med Assoc Thai. 2010; 93:1088–1092.15. Carr AS, Pelayo-Negro AL, Jaunmuktane Z, et al. Transthyretin V122I amyloidosis with clinical and histological evidence of amyloid neuropathy and myopathy. Neuromuscul Disord. 2015; 25:511–515.16. Longhi S, Quarta CC, Milandri A, et al. Atrial fibrillation in amyloidotic cardiomyopathy: prevalence, incidence, risk factors and prognostic role. Amyloid. 2015; 22:147–155.17. Klein CJ, Wu Y, Vogel P, et al. Ubiquitin ligase defect by DCAF8 mutation causes HMSN2 with giant axons. Neurology. 2014; 82:873–878.18. Uechi Y, Higa K. Recurrent takotsubo cardiomyopathy within a short span of time in a patient with hereditary motor and sensory neuropathy. Intern Med. 2008; 47:1609–1613.19. Corrado G, Checcarelli N, Santarone M, Stollberger C, Finsterer J. Left ventricular hypertrabeculation/noncompaction with PMP22 duplication-based Charcot-Marie-Tooth disease type 1A. Cardiology. 2006; 105:142–145.20. Hofstad H, Ohm OJ, Mørk SJ, Aarli JA. Heart disease in myasthenia gravis. Acta Neurol Scand. 1984; 70:176–184.21. Tanahashi N, Sato H, Nogawa S, Satoh T, Kawamura M, Shimoda M. A case report of giant cell myocarditis and myositis observed during the clinical course of invasive thymoma associated with myasthenia gravis. Keio J Med. 2004; 53:30–42.22. Thanaviratananich S, Katirji B, Alshekhlee A. Broken heart syndrome during myasthenic crisis. J Clin Neuromuscul Dis. 2014; 15:90–95.23. Mayor-Gomez S, Lacruz F, Ezpeleta D. Myasthenic crisis and Takotsubo syndrome: a non-chance relationship. Rev Neurol. 2012; 55:725–728.24. Bansal V, Kansal MM, Rowin J. Broken heart syndrome in myasthenia gravis. Muscle Nerve. 2011; 44:990–993.25. Beydoun SR, Wang J, Levine RL, Farvid A. Emotional stress as a trigger of myasthenic crisis and concomitant takotsubo cardiomyopathy: a case report. J Med Case Rep. 2010; 4:393.26. Lang SM, Shugh S, Mazur W, et al. Myocardial fibrosis and left ventricular dysfunction in Duchenne muscular dystrophy carriers using cardiac magnetic resonance imaging. Pediatr Cardiol. 2015; 36:1495–1501.27. Brunklaus A, Parish E, Muntoni F, et al. The value of cardiac MRI versus echocardiography in the pre-operative assessment of patients with Duchenne muscular dystrophy. Eur J Paediatr Neurol. 2015; 19:395–401.28. Tandon A, Villa CR, Hor KN, et al. Myocardial fibrosis burden predicts left ventricular ejection fraction and is associated with age and steroid treatment duration in duchenne muscular dystrophy. J Am Heart Assoc. 2015; (4):pii: e001338.29. Finsterer J, Gelpi E, Stöllberger C. Left ventricular hypertrabeculation/noncompaction as a cardiac manifestation of Duchenne muscular dystrophy under non-invasive positive-pressure ventilation. Acta Cardiol. 2005; 60:445–448.30. Florian A, Rösch S, Bietenbeck M, et al. Cardiac involvement in female Duchenne and Becker muscular dystrophy carriers in comparison to their first-degree male relatives: a comparative cardiovascular magnetic resonance study. Eur Heart J Cardiovasc Imaging. 2015; [Epub ahead of print].31. Birnkrant DJ, Ararat E, Mhanna MJ. Cardiac phenotype determines survival in Duchenne muscular dystrophy. Pediatr Pulmonol. 2015; [Epub ahead of print].32. Vidal-Pérez R, Diaz-Villanueva J, Arzanauskaite M, Rojas R, Carreras F. Cardiac involvement in Becker muscular dystrophy: role of cardiovascular magnetic resonance. Eur Heart J Cardiovasc Imaging. 2013; 14:1038.33. Andrikopoulos G, Kourouklis S, Trika C, et al. Cardiac resynchronization therapy in becker muscular dystrophy. Hellenic J Cardiol. 2013; 54:227–229.34. Tsuda T, Fitzgerald K, Scavena M, et al. Early-progressive dilated cardiomyopathy in a family with Becker muscular dystrophy related to a novel frameshift mutation in the dystrophin gene exon 27. J Hum Genet. 2015; 60:151–155.35. Guo X, Dai Y, Cui L, Fang Q. A novel dystrophin deletion mutation in a becker muscular dystrophy patient with early-onset dilated cardiomyopathy. Can J Cardiol. 2014; 30:956.e1–956.e3.36. Petri H, Sveen ML, Thune JJ, et al. Progression of cardiac involvement in patients with limb-girdle type 2 and Becker muscular dystrophies: a 9-year follow-up study. Int J Cardiol. 2015; 182:403–411.37. van den Bergen JC, Schade van Westrum SM, Dekker L, et al. Clinical characterisation of Becker muscular dystrophy patients predicts favourable outcome in exon-skipping therapy. J Neurol Neurosurg Psychiatry. 2014; 85:92–98.38. Finsterer J, Stöllberger C, Sehnal E, Rehder H, Laccone F. Dilated, arrhythmogenic cardiomyopathy in emery-dreifuss muscular dystrophy due to the emerin splice-site mutation c.449 + 1G>A. Cardiology. 2015; 130:48–51.39. Pen AE, Nyegaard M, Fang M, et al. A novel single nucleotide splice site mutation in FHL1 confirms an Emery-Dreifuss plus phenotype with pulmonary artery hypoplasia and facial dysmorphology. Eur J Med Genet. 2015; 58:222–229.40. Gossios TD, Lopes LR, Elliott PM. Left ventricular hypertrophy caused by a novel nonsense mutation in FHL1. Eur J Med Genet. 2013; 56:251–255.41. Tiffin HR, Jenkins ZA, Gray MJ, et al. Dysregulation of FHL1 spliceforms due to an indel mutation produces an Emery-Dreifuss muscular dystrophy plus phenotype. Neurogenetics. 2013; 14:113–121.42. Wessely R, Seidl S, Schömig A. Cardiac involvement in Emery-Dreifuss muscular dystrophy. Clin Genet. 2005; 67:220–223.43. Coutance G, Labombarda F, Cauderlier E, et al. Hypoplasia of the aorta in a patient diagnosed with LMNA gene mutation. Congenit Heart Dis. 2013; 8:E127–E129.44. Redondo-Vergé L, Yaou RB, Fernández-Recio M, Dinca L, Richard P, Bonne G. Cardioembolic stroke prompting diagnosis of LMNA-associated Emery-Dreifuss muscular dystrophy. Muscle Nerve. 2011; 44:587–589.45. Maggi L, D'Amico A, Pini A, et al. LMNA-associated myopathies: the Italian experience in a large cohort of patients. Neurology. 2014; 83:1634–1644.46. Sveen ML, Thune JJ, Køber L, Vissing J. Cardiac involvement in patients with limb-girdle muscular dystrophy type 2 and Becker muscular dystrophy. Arch Neurol. 2008; 65:1196–1201.47. Groh WJ. Arrhythmias in the muscular dystrophies. Heart Rhythm. 2012; 9:1890–1895.48. Volpi L, Ricci G, Passino C, et al. Prevalent cardiac phenotype resulting in heart transplantation in a novel LMNA gene duplication. Neuromuscul Disord. 2010; 20:512–516.49. Quick S, Schaefer J, Waessnig N, et al. Evaluation of heart involvement in calpainopathy (LGMD2A) using cardiovascular magnetic resonance. Muscle Nerve. 2015; 52:661–663.50. Okere A, Reddy SS, Gupta S, Shinnar M. A cardiomyopathy in a patient with limb girdle muscular dystrophy type 2A. Circ Heart Fail. 2013; 6:e12–e13.51. Nishikawa A, Mori-Yoshimura M, Segawa K, et al. Respiratory and cardiac function in Japanese patients with dysferlinopathy. Muscle Nerve. 2015; [Epub ahead of print].52. Rosales XQ, Moser SJ, Tran T, et al. Cardiovascular magnetic resonance of cardiomyopathy in limb girdle muscular dystrophy 2B and 2I. J Cardiovasc Magn Reson. 2011; 13:39.53. Takahashi T, Aoki M, Suzuki N, et al. Clinical features and a mutation with late onset of limb girdle muscular dystrophy 2B. J Neurol Neurosurg Psychiatry. 2013; 84:433–440.54. Kuru S, Yasuma F, Wakayama T, et al. A patient with limb girdle muscular dystrophy type 2B (LGMD2B) manifesting cardiomyopathy. Rinsho Shinkeigaku. 2004; 44:375–378.55. Calvo F, Teijeira S, Fernandez JM, et al. Evaluation of heart involvement in gamma-sarcoglycanopathy (LGMD2C). A study of ten patients. Neuromuscul Disord. 2000; 10:560–566.56. Merlini L, Kaplan JC, Navarro C, et al. Homogeneous phenotype of the gypsy limb-girdle MD with the gamma-sarcoglycan C283Y mutation. Neurology. 2000; 54:1075–1079.57. Semplicini C, Vissing J, Dahlqvist JR, et al. Clinical and genetic spectrum in limb-girdle muscular dystrophy type 2E. Neurology. 2015; 84:1772–1781.58. Fanin M, Melacini P, Boito C, Pegoraro E, Angelini C. LGMD2E patients risk developing dilated cardiomyopathy. Neuromuscul Disord. 2003; 13:303–309.59. Wahbi K, Meune C, Hamouda el H, et al. Cardiac assessment of limb-girdle muscular dystrophy 2I patients: an echography, Holter ECG and magnetic resonance imaging study. Neuromuscul Disord. 2008; 18:650–655.60. Hollingsworth KG, Willis TA, Bates MG, et al. Subepicardial dysfunction leads to global left ventricular systolic impairment in patients with limb girdle muscular dystrophy 2I. Eur J Heart Fail. 2013; 15:986–994.61. Gaul C, Deschauer M, Tempelmann C, et al. Cardiac involvement in limb-girdle muscular dystrophy 2I: conventional cardiac diagnostic and cardiovascular magnetic resonance. J Neurol. 2006; 253:1317–1322.62. D'Amico A, Petrini S, Parisi F, et al. Heart transplantation in a child with LGMD2I presenting as isolated dilated cardiomyopathy. Neuromuscul Disord. 2008; 18:153–155.63. Schottlaender LV, Petzold A, Wood N, Houlden H. Diagnostic clues and manifesting carriers in fukutin-related protein (FKRP) limb-girdle muscular dystrophy. J Neurol Sci. 2015; 348:266–268.64. Matsui M, Endo T, Matsumura T, Saito T, Fujimura H. A case of limb-girdle muscular dystrophy 2M diagnosed by the occurence of dilated cardiomyopathy. Rinsho Shinkeigaku. 2015; 55:585–588.65. Schade van Westrum SM, Dekker LR, de Voogt WG, et al. Cardiac involvement in Dutch patients with sarcoglycanopathy: a cross-sectional cohort and follow-up study. Muscle Nerve. 2014; 50:909–913.66. Dinçer P, Bönnemann CG, Erdir Aker O, et al. A homozygous nonsense mutation in delta-sarcoglycan exon 3 in a case of LGMD2F. Neuromuscul Disord. 2000; 10:247–250.67. Tsubata S, Bowles KR, Vatta M, et al. Mutations in the human delta-sarcoglycan gene in familial and sporadic dilated cardiomyopathy. J Clin Invest. 2000; 106:655–662.68. Finsterer J, Stöllberger C, Gatterer E, Jakubiczka S. Intermittent pre-excitation-syndrome in facio-scapulo-humeral muscular dystrophy. Korean Circ J. 2014; 44:348–350.69. Nakayama T, Komiya T, Tyou E, Watanabe S, Kawai M. Cardiac deformity and dysfunction in facioscapulohumeral dystrophy--electrocardiogram, ECG gate cardiac MRI studies. Rinsho Shinkeigaku. 1999; 39:610–614.70. Faustmann PM, Farahati J, Rupilius B, Dux R, Koch MC, Reiners C. Cardiac involvement in facio-scapulo-humeral muscular dystrophy: a family study using Thallium-201 single-photon-emission-computed tomography. J Neurol Sci. 1996; 144:59–63.71. Della Marca G, Frusciante R, Scatena M, et al. Heart rate variability in facioscapulohumeral muscular dystrophy. Funct Neurol. 2010; 25:211–216.72. Pasqualin LM, Reed UC, Costa TV, et al. Congenital muscular dystrophy with dropped head linked to the LMNA gene in a Brazilian cohort. Pediatr Neurol. 2014; 50:400–406.73. Flöck A, Kornblum C, Hammerstingl C, Claeys KG, Gembruch U, Merz WM. Progressive cardiac dysfunction in Bethlem myopathy during pregnancy. Obstet Gynecol. 2014; 123:2 Pt 2 Suppl 2. 436–438.74. Plonka C, Wearden PD, Morell VO, Miller SA, Webber SA, Feingold B. Successful heart transplantation from a donor with Ullrich congenital muscular dystrophy. Am J Transplant. 2013; 13:1915–1917.75. Martinez HR, Craigen WJ, Ummat M, Adesina AM, Lotze TE, Jefferies JL. Novel cardiovascular findings in association with a POMT2 mutation: three siblings with α-dystroglycanopathy. Eur J Hum Genet. 2014; 22:486–491.76. Haliloglu G, Talim B, Sel CG, Topaloglu H. Clinical characteristics of megaconial congenital muscular dystrophy due to choline kinase beta gene defects in a series of 15 patients. J Inherit Metab Dis. 2015; 38:1099–1108.77. Marques J, Duarte ST, Costa S, et al. Atypical phenotype in two patients with LAMA2 mutations. Neuromuscul Disord. 2014; 24:419–424.78. Carboni N, Marrosu G, Porcu M, et al. Dilated cardiomyopathy with conduction defects in a patient with partial merosin deficiency due to mutations in the laminin-α2-chain gene: a chance association or a novel phenotype. Muscle Nerve. 2011; 44:826–828.79. Matsuda H, Arai M, Okamoto H. Total intravenous anesthesia for a patient with Fukuyama congenital muscular dystrophy undergoing scoliosis surgery. Masui. 2014; 63:650–653.80. Pane M, Messina S, Vasco G, et al. Respiratory and cardiac function in congenital muscular dystrophies with alpha dystroglycan deficiency. Neuromuscul Disord. 2012; 22:685–689.81. Ceviz N, Alehan F, Alehan D, et al. Assessment of left ventricular systolic and diastolic functions in children with merosin-positive congenital muscular dystrophy. Int J Cardiol. 2003; 87:129–133. discussion 133-482. Vattemi G, Neri M, Piffer S, et al. Clinical, morphological and genetic studies in a cohort of 21 patients with myofibrillar myopathy. Acta Myol. 2011; 30:121–126.83. Konersman CG, Bordini BJ, Scharer G, et al. BAG3 myofibrillar myopathy presenting with cardiomyopathy. Neuromuscul Disord. 2015; 25:418–422.84. Lee HC, Cherk SW, Chan SK, et al. BAG3-related myofibrillar myopathy in a Chinese family. Clin Genet. 2012; 81:394–398.85. Liewluck T, Kintarak J, Sangruchi T, Selcen D, Kulkantrakorn K. Myofibrillar myopathy with limb-girdle phenotype in a Thai patient. J Med Assoc Thai. 2009; 92:290–295.86. Piñol-Ripoll G, Shatunov A, Cabello A, et al. Severe infantile-onset cardiomyopathy associated with a homozygous deletion in desmin. Neuromuscul Disord. 2009; 19:418–422.87. Zheng M, Cheng H, Li X, et al. Cardiac-specific ablation of Cypher leads to a severe form of dilated cardiomyopathy with premature death. Hum Mol Genet. 2009; 18:701–713.88. Stöllberger C, Gatterer E, Finsterer J, Kuck KH, Tilz RR. Repeated radiofrequency ablation of atrial tachycardia in restrictive cardiomyopathy secondary to myofibrillar myopathy. J Cardiovasc Electrophysiol. 2014; 25:905–907.89. El-Menyar AA, Al-Suwaidi J, Gehani AA, Bener A. Clinical and histologic studies of a Qatari family with myofibrillar myopathy. Saudi Med J. 2004; 25:1723–1726.90. Chauveau C, Bonnemann CG, Julien C, et al. Recessive TTN truncating mutations define novel forms of core myopathy with heart disease. Hum Mol Genet. 2014; 23:980–991.91. Şimşek Z, Açar G, Akçakoyun M, Esen Ö, Emiroğlu Y, Esen AM. Left ventricular noncompaction in a patient with multiminicore disease. J Cardiovasc Med (Hagerstown). 2012; 13:660–662.92. Cullup T, Lamont PJ, Cirak S, et al. Mutations in MYH7 cause Multi-minicore Disease (MmD) with variable cardiac involvement. Neuromuscul Disord. 2012; 22:1096–1104.93. Hachenberg T, Brssel T, Lawin P, Konertz W, Scheld HH. Heart transplantation in a patient with central core disease. J Cardiothorac Vasc Anesth. 1992; 6:386–387.94. Gal A, Inczedy-Farkas G, Pal E, et al. The coexistence of dynamin 2 mutation and multiple mitochondrial DNA (mtDNA) deletions in the background of severe cardiomyopathy and centronuclear myopathy. Clin Neuropathol. 2015; 34:89–95.95. Al-Ruwaishid A, Vajsar J, Tein I, Benson L, Jay V. Centronuclear myopathy and cardiomyopathy requiring heart transplant. Brain Dev. 2003; 25:62–66.96. Hikita T, Wakita S, Mori Y, et al. Severe infantile myotubular myopathy with complete atrioventricular block. Pediatr Int. 2008; 50:698–700.97. Fujita K, Nakano S, Yamamoto H, Ito H, Ito H, Goto Y, Kusaka H. An adult case of congenital fiber type disproportion (CFTD) with cardiomyopathy. Rinsho Shinkeigaku. 2005; 45:380–382.98. Kajino S, Ishihara K, Goto K, et al. Congenital fiber type disproportion myopathy caused by LMNA mutations. J Neurol Sci. 2014; 340:94–98.99. Gatayama R, Ueno K, Nakamura H, et al. Nemaline myopathy with dilated cardiomyopathy in childhood. Pediatrics. 2013; 131:e1986–e1990.100. Sarullo FM, Vitale G, Di Franco A, et al. Nemaline myopathy and heart failure: role of ivabradine; a case report. BMC Cardiovasc Disord. 2015; 15:5.101. Mir A, Lemler M, Ramaciotti C, Blalock S, Ikemba C. Hypertrophic cardiomyopathy in a neonate associated with nemaline myopathy. Congenit Heart Dis. 2012; 7:E37–E41.102. Müller TJ, Kraya T, Stoltenburg-Didinger G, et al. Phenotype of matrin-3-related distal myopathy in 16 German patients. Ann Neurol. 2014; 76:669–680.103. Naddaf E, Waclawik AJ. Two families with MYH7 distal myopathy associated with cardiomyopathy and core formations. J Clin Neuromuscul Dis. 2015; 16:164–169.104. Lefter S, Hardiman O, McLaughlin RL, Murphy SM, Farrell M, Ryan AM. A novel MYH7 Leu1453pro mutation resulting in Laing distal myopathy in an Irish family. Neuromuscul Disord. 2015; 25:155–160.105. Finsterer J, Stöllberger C, Brandau O, Laccone F, Bichler K, Laing NG. Novel MYH7 mutation associated with mild myopathy but life-threatening ventricular arrhythmias and noncompaction. Int J Cardiol. 2014; 173:532–535.106. D'Arcy C, Kanellakis V, Forbes R, et al. X-linked recessive distal myopathy with hypertrophic cardiomyopathy caused by a novel mutation in the FHL1 gene. J Child Neurol. 2015; 30:1211–1217.107. Kayman-Kurekci G, Talim B, Korkusuz P, et al. Mutation in TOR1AIP1 encoding LAP1B in a form of muscular dystrophy: a novel gene related to nuclear envelopathies. Neuromuscul Disord. 2014; 24:624–633.108. Nalini A, Gayathri N, Richard P, Cobo AM, Urtizberea JA. New mutation of the desmin gene identified in an extended Indian pedigree presenting with distal myopathy and cardiac disease. Neurol India. 2013; 61:622–626.109. Nishino I, Noguchi S, Murayama K, et al. Molecular pathomechanism of distal myopathy with rimmed vacuoles. Rinsho Shinkeigaku. 2005; 45:943–945.110. Ishiwata S, Nishiyama S, Seki A, Kojima S. Restrictive cardiomyopathy with complete atrioventricular block and distal myopathy with rimmed vacuoles. Jpn Circ J. 1993; 57:928–933.111. Kimpara T, Imamura T, Tsuda T, Sato K, Tsuburaya K. Distal myopathy with rimmed vacuoles and sudden death--report of two siblings. Rinsho Shinkeigaku. 1993; 33:886–890.112. Krendel DA, Gilchrist JM, Bossen EH. Distal vacuolar myopathy with complete heart block. Arch Neurol. 1988; 45:698–699.113. Maffé S, Signorotti F, Perucca A, et al. Atypical arrhythmic complications in familial hypokalemic periodic paralysis. J Cardiovasc Med (Hagerstown). 2009; 10:68–71.114. Green DS, Hayward LJ, George AL Jr, Cannon SC. A proposed mutation, Val781Ile, associated with hyperkalemic periodic paralysis and cardiac dysrhythmia is a benign polymorphism. Ann Neurol. 1997; 42:253–256.115. Stunnenberg BC, Deinum J, Links TP, Wilde AA, Franssen H, Drost G. Cardiac arrhythmias in hypokalemic periodic paralysis: Hypokalemia as only cause? Muscle Nerve. 2014; 50:327–332.116. Caballero PE. Becker myotonia congenita associated with Wolff-Parkinson-White syndrome. Neurologist. 2011; 17:38–40.117. Benhayon D, Lugo R, Patel R, Carballeira L, Elman L, Cooper JM. Long-term arrhythmia follow-up of patients with myotonic dystrophy. J Cardiovasc Electrophysiol. 2015; 26:305–310.118. Brembilla-Perrot B, Schwartz J, Huttin O, et al. Atrial flutter or fibrillation is the most frequent and life-threatening arrhythmia in myotonic dystrophy. Pacing Clin Electrophysiol. 2014; 37:329–335.119. Pambrun T, Bortone A, Bois P, et al. Unmasked Brugada pattern by ajmaline challenge in patients with myotonic dystrophy type 1. Ann Noninvasive Electrocardiol. 2015; 20:28–36.120. Russo V, Di Meo F, Rago A, et al. Paroxysmal atrial fibrillation in myotonic dystrophy type 1 patients: P wave duration and dispersion analysis. Eur Rev Med Pharmacol Sci. 2015; 19:1241–1248.121. Finsterer J, Stöllberger C, Gencik M, Höftberger R, Rahimi J, Mokocki J. Syncope and hyperCKemia as minimal manifestations of short CTG repeat expansions in myotonic dystrophy type 1. Rev Port Cardiol. 2015; 34:361.e1–361.e4.122. Finsterer J, Rudnik-Schöneborn S. Myotonic dystrophies: clinical presentation, pathogenesis, diagnostics and therapy. Fortschr Neurol Psychiatr. 2015; 83:9–17.123. Kilic T, Vural A, Ural D, et al. Cardiac resynchronization therapy in a case of myotonic dystrophy (Steinert's disease) and dilated cardiomyopathy. Pacing Clin Electrophysiol. 2007; 30:916–920.124. Finsterer J, Stölberger C, Kopsa W. Noncompaction in myotonic dystrophy type 1 on cardiac MRI. Cardiology. 2005; 103:167–168.125. Petri H, Ahtarovski KA, Vejlstrup N, et al. Myocardial fibrosis in patients with myotonic dystrophy type 1: a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson. 2014; 16:59.126. Petri H, Witting N, Ersbøll MK, et al. High prevalence of cardiac involvement in patients with myotonic dystrophy type 1: a crosssectional study. Int J Cardiol. 2014; 174:31–36.127. Bu'Lock FA, Sood M, De Giovanni JV, Green SH. Left ventricular diastolic function in congenital myotonic dystrophy. Arch Dis Child. 1999; 80:267–270.128. Viitasalo MT, Kala R, Karli P, Eisalo A. Ambulatory electrocardiographic recording in mild or moderate myotonic dystrophy and myotonia congenita (Thomsen's disease). J Neurol Sci. 1983; 62:181–190.129. Kim HN, Cho YK, Cho JH, Yang EM, Song ES, Choi YY. Transient complete atrioventricular block in a preterm neonate with congenital myotonic dystrophy: case report. J Korean Med Sci. 2014; 29:879–883.130. Rudnik-Schöneborn S, Schaupp M, Lindner A, et al. Brugada-like cardiac disease in myotonic dystrophy type 2: report of two unrelated patients. Eur J Neurol. 2011; 18:191–194.131. Lee TM, Maurer MS, Karbassi I, Braastad C, Batish SD, Chung WK. Severe dilated cardiomyopathy in a patient with myotonic dystrophy type 2 and homozygous repeat expansion in ZNF9. Congest Heart Fail. 2012; 18:183–186.132. Wahbi K, Meune C, Bassez G, et al. Left ventricular non-compaction in a patient with myotonic dystrophy type 2. Neuromuscul Disord. 2008; 18:331–333.133. Brunetti-Pierri N, Pignatelli R, Fouladi N, et al. Dilation of the aortic root in mitochondrial disease patients. Mol Genet Metab. 2011; 103:167–170.134. Finsterer J. Is atherosclerosis a mitochondrial disorder? Vasa. 2007; 36:229–240.135. Dominic EA, Ramezani A, Anker SD, Verma M, Mehta N, Rao M. Mitochondrial cytopathies and cardiovascular disease. Heart. 2014; 100:611–618.136. Yajima N, Yazaki Y, Yoshida K, et al. A case of mitochondrial cardiomyopathy with pericardial effusion evaluated by (99m)Tc-MIBI myocardial scintigraphy. J Nucl Cardiol. 2009; 16:989–994.137. Barisić N, Kleiner IM, Malcić I, Papa J, Boranić M. Spinal dysraphism associated with congenital heart disorder in a girl with MELAS syndrome and point mutation at mitochondrial DNA nucleotide 3271. Croat Med J. 2002; 43:37–41.138. Barragán-Campos HM, Barrera-Ramírez CF, Iturralde Torres P, et al. Kearns-Sayre syndromes an absolute indication for prophylactic implantation of definitive pacemaker? Arch Inst Cardiol Mex. 1999; 69:559–565.139. Aimo A, Giannoni A, Piepoli MF, et al. Myocardial damage in a mitochondrial myopathy patient with increased ergoreceptor sensitivity and sympatho-vagal imbalance. Int J Cardiol. 2014; 176:1396–1398.140. Brecht M, Richardson M, Taranath A, Grist S, Thorburn D, Bratkovic D. Leigh syndrome daused by the MT-ND5 m.13513G>A mutation: a case present ing wi th WPW-l ike conduct ion defect , cardiomyopathy, hypertension and hyponatraemia. JIMD Rep. 2015; 19:95–100.141. Limongelli G, Tome-Esteban M, Dejthevaporn C, Rahman S, Hanna MG, Elliott PM. Prevalence and natural history of heart disease in adults with primary mitochondrial respiratory chain disease. Eur J Heart Fail. 2010; 12:114–121.142. Watanabe Y, Odaka M, Hirata K. Case of Leber's hereditary optic neuropathy with mitochondrial DNA 11778 mutation exhibiting cerebellar ataxia, dilated cardiomyopathy and peripheral neuropathy. Brain Nerve. 2009; 61:309–312.143. Florian A, Ludwig A, Stubbe-Dräger B, et al. Characteristic cardiac phenotypes are detected by cardiovascular magnetic resonance in patients with different clinical phenotypes and genotypes of mitochondrial myopathy. J Cardiovasc Magn Reson. 2015; 17:40.144. Brea-Calvo G, Haack TB, Karall D, et al. COQ4 mutations cause a broad spectrum of mitochondrial disorders associated with CoQ10 deficiency. Am J Hum Genet. 2015; 96:309–317.145. Kopajtich R, Nicholls TJ, Rorbach J, et al. Mutations in GTPBP3 cause a mitochondrial translation defect associated with hypertrophic cardiomyopathy, lactic acidosis, and encephalopathy. Am J Hum Genet. 2014; 95:708–720.146. Distelmaier F, Haack TB, Catarino CB, et al. MRPL44 mutations cause a slowly progressive multisystem disease with childhood-onset hypertrophic cardiomyopathy. Neurogenetics. 2015; 16:319–323.147. Brisca G, Fiorillo C, Nesti C, et al. Early onset cardiomyopathy associated with the mitochondrial tRNALeu((UUR)) 3271T>C MELAS mutation. Biochem Biophys Res Commun. 2015; 458:601–604.148. Wortmann SB, Champion MP, van den Heuvel L, et al. Mitochondrial DNA m.3242G > A mutation, an under diagnosed cause of hypertrophic cardiomyopathy and renal tubular dysfunction. Eur J Med Genet. 2012; 55:552–556.149. Wang SB, Weng WC, Lee NC, Hwu WL, Fan PC, Lee WT. Mutation of mitochondrial DNA G13513A presenting with Leigh syndrome, Wolff-Parkinson-White syndrome and cardiomyopathy. Pediatr Neonatol. 2008; 49:145–149.150. Menotti F, Brega A, Diegoli M, Grasso M, Modena MG, Arbustini E. A novel mtDNA point mutation in tRNA(Val) is associated with hypertrophic cardiomyopathy and MELAS. Ital Heart J. 2004; 5:460–465.151. Homan DJ, Niyazov DM, Fisher PW, et al. Heart transplantation for a patient with Kearns-Sayre syndrome and end-stage heart failure. Congest Heart Fail. 2011; 17:102–104.152. Malfatti E, Laforêt P, Jardel C, et al. High risk of severe cardiac adverse events in patients with mitochondrial m.3243A>G mutation. Neurology. 2013; 80:100–105.153. Finsterer J, Stöllberger C, Sehnal E, Valentin A, Huber J, Schmiedel J. Apical ballooning (Takotsubo syndrome) in mitochondrial disorder during mechanical ventilation. J Cardiovasc Med (Hagerstown). 2007; 8:859–863.154. Sacconi S, Wahbi K, Theodore G, et al. Atrio-ventricular block requiring pacemaker in patients with late onset Pompe disease. Neuromuscul Disord. 2014; 24:648–650.155. Mogahed EA, Girgis MY, Sobhy R, Elhabashy H, Abdelaziz OM, El-Karaksy H. Skeletal and cardiac muscle involvement in children with glycogen storage disease type III. Eur J Pediatr. 2015; 174:1545–1548.156. Sentner CP, Caliskan K, Vletter WB, Smit GP. Heart failure due to severe hypertrophic cardiomyopathy reversed by low calorie, high protein dietary adjustments in a glycogen storage disease type IIIa patient. JIMD Rep. 2012; 5:13–16.157. Austin SL, Proia AD, Spencer-Manzon MJ, Butany J, Wechsler SB, Kishnani PS. Cardiac pathology in glycogen storage disease type III. JIMD Rep. 2012; 6:65–72.158. LaBarbera M, Milechman G, Dulbecco F. Premature coronary artery disease in a patient with glycogen storage disease III. J Invasive Cardiol. 2010; 22:E156–E158.159. Magoulas PL, El-Hattab AW. Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Dolan CR, Fong CT, Smith RJH, Stephens K, editors. Glycogen Storage Disease Type IV. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle;1993-2015. 2013 Jan 03. Available from http://www.ncbi.nlm.nih.gov/books/NBK115333/.160. Moustafa S, Patton DJ, Connelly MS. Unforeseen cardiac involvement in McArdle's disease. Heart Lung Circ. 2013; 22:769–771.161. Amit R, Bashan N, Abarbanel JM, Shapira Y, Sofer S, Moses S. Fatal familial infantile glycogen storage disease: multisystem phosphofructokinase deficiency. Muscle Nerve. 1992; 15:455–458.162. Schoser B, Bruno C, Schneider HC, et al. Unclassified polysaccharidosis of the heart and skeletal muscle in siblings. Mol Genet Metab. 2008; 95:52–58.163. Baruteau J, Sachs P, Broué P, et al. Clinical and biological features at diagnosis in mitochondrial fatty acid beta-oxidation defects: a French pediatric study of 187 patients. J Inherit Metab Dis. 2013; 36:795–803.164. Ojala T, Nupponen I, Saloranta C, et al. Fetal left ventricular noncompaction cardiomyopathy and fatal outcome due to complete deficiency of mitochondrial trifunctional protein. Eur J Pediatr. 2015; 174:1689–1692.165. Zhang RN, Li YF, Qiu WJ, et al. Clinical features and mutations in seven Chinese patients with very long chain acyl-CoA dehydrogenase deficiency. World J Pediatr. 2014; 10:119–125.166. Eminoglu TF, Tumer L, Okur I, Ezgu FS, Biberoglu G, Hasanoglu A. Very long-chain acyl CoA dehydrogenase deficiency which was accepted as infanticide. Forensic Sci Int. 2011; 210:e1–e3.167. Missaglia S, Tasca E, Angelini C, Moro L, Tavian D. Novel missense mutations in PNPLA2 causing late onset and clinical heterogeneity of neutral lipid storage disease with myopathy in three siblings. Mol Genet Metab. 2015; 115:110–117.168. Kaneko K, Kuroda H, Izumi R, et al. A novel mutation in PNPLA2 causes neutral lipid storage disease with myopathy and triglyceride deposit cardiomyovasculopathy: a case report and literature review. Neuromuscul Disord. 2014; 24:634–641.169. Iacobazzi V, Invernizzi F, Baratta S, et al. Molecular and functional analysis of SLC25A20 mutations causing carnitine-acylcarnitine translocase deficiency. Hum Mutat. 2004; 24:312–320.170. Yilmaz BS, Kor D, Mungan NO, Erdem S, Ceylaner S. Primary systemic carnitine deficiency: a Turkish case with a novel homozygous SLC22A5 mutation and 14 years follow-up. J Pediatr Endocrinol Metab. 2015; 28:1179–1181.171. Ronvelia D, Greenwood J, Platt J, Hakim S, Zaragoza MV. Intrafamilial variability for novel TAZ gene mutation: barth syndrome with dilated cardiomyopathy and heart failure in an infant and left ventricular noncompaction in his great-uncle. Mol Genet Metab. 2012; 107:428–432.172. Van Der Starre P, Deuse T, Pritts C, Brun C, Vogel H, Oyer P. Late profound muscle weakness following heart transplantation due to Danon disease. Muscle Nerve. 2013; 47:135–137.173. Miani D, Taylor M, Mestroni L, et al. Sudden death associated with danon disease in women. Am J Cardiol. 2012; 109:406–411.174. Oliveira J, Negrão L, Fineza I, et al. New splicing mutation in the choline kinase beta (CHKB) gene causing a muscular dystrophy detected by whole-exome sequencing. J Hum Genet. 2015; 60:305–312.175. Dittrich S, Tuerk M, Haaker G, et al. Cardiomyopathy in duchenne muscular dystrophy: current value of clinical, electrophysiological and imaging findings in children and teenagers. Klin Padiatr. 2015; 227:225–231.176. van Westering TL, Betts CA, Wood MJ. Current understanding of molecular pathology and treatment of cardiomyopathy in duchenne muscular dystrophy. Molecules. 2015; 20:8823–8855.177. Wochna K, Jurczyk AP, Krajewski W, Berent J. Sudden death due to malignant hyperthermia during general anesthesia. Arch Med Sadowej Kryminol. 2013; 63:11–14. 7–10.178. Finsterer J, Cripe L. Treatment of dystrophin cardiomyopathies. Nat Rev Cardiol. 2014; 11:168–179.179. Dec GW. Steroid therapy effectively delays Duchenne's cardiomyopathy. J Am Coll Cardiol. 2013; 61:955–956.180. But WM, Lee SH, Chan AO, Lau GT. Enzyme replacement therapy for infantile Pompe disease during the critical period and identification of a novel mutation. Hong Kong Med J. 2009; 15:474–477.181. Prater SN, Banugaria SG, DeArmey SM, et al. The emerging phenotype of long-term survivors with infantile Pompe disease. Genet Med. 2012; 14:800–810.182. Yoda M, Tanabe H, Nishino I, Suma H. Left ventriculoplasty for dilated cardiomyopathy in Fukuyama-type muscular dystrophy. Eur J Cardiothorac Surg. 2011; 40:514–516.183. Jefferies JL, Wilkinson JD, Sleeper LA, et al. Cardiomyopathy phenotypes and outcomes for children with left ventricular myocardial noncompaction: results from the pediatric cardiomyopathy registry. J Card Fail. 2015; 21:877–884.184. Authors/Task Force members. Elliott PM, Anastasakis A, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014; 35:2733–2779.185. Gdynia HJ, Kurt A, Endruhn S, Ludolph AC, Sperfeld AD. Cardiomyopathy in motor neuron diseases. J Neurol Neurosurg Psychiatry. 2006; 77:671–673.186. Hattori T, Ikeda S, Yoshida K, Yanagisawa N, Furihata K, Yoshida K. A patient with Kennedy-Alter-Sung syndrome showing cardiomyopathy. Rinsho Shinkeigaku. 1995; 35:1246–1249.187. Al-Thihli K, Ebrahim H, Hughes DA, et al. A variant of unknown significance in the GLA gene causing diagnostic uncertainty in a young female with isolated hypertrophic cardiomyopathy. Gene. 2012; 497:320–322.188. Nussinovitch U, Katz U, Nussinovitch M, Nussinovitch N. Beat-to-beat QT interval dynamics and variability in familial dysautonomia. Pediatr Cardiol. 2010; 31:80–84.189. Ergül Y, Ekici B, Keskin S. Cardiac arrest after anesthetic management in a patient with hereditary sensory autonomic neuropathy type IV. Saudi J Anaesth. 2011; 5:93–95.190. Losito L, De Rinaldis M, Gennaro L, et al. Charcot-Marie-Tooth type 1a in a child with Long QT syndrome. Eur J Paediatr Neurol. 2009; 13:459–462.191. Millaire A, Warembourg A, Leys D, et al. Refsum's disease. Apropos of 2 cases disclosed by myocardiopathy. Ann Cardiol Angeiol (Paris). 1990; 39:173–178.192. Nakagawa H, Okayama S, Kamon D, et al. Refractory high output heart failure in a patient with primary mitochondrial respiratory chain disease. Intern Med. 2014; 53:315–319.193. Palecek T, Tesarova M, Kuchynka P, et al. Hypertrophic cardiomyopathy due to the mitochondrial DNA mutation m.3303C>T diagnosed in an adult male. Int Heart J. 2012; 53:383–387.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Muscle and Nerve Biopsy in Various Neuromuscular Disorders
- Comparison between the Electric and Magnetic Stimulations for a Repetitive Nerve Stimulation Test
- Autoantibody Testing in Neuromuscular Disorders
- Neuromuscular Ultrasound of Cranial Nerves
- Nerve conduction studies: basic principal and clinical usefulness