Korean Circ J.
2016 May;46(3):315-323. 10.4070/kcj.2016.46.3.315.
Differential Clinical Implications of High-Degree Atrioventricular Block Complicating ST-Segment Elevation Myocardial Infarction according to the Location of Infarction in the Era of Primary Percutaneous Coronary Intervention
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea. mhjeong@chonnam.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Yeungnam University Hospital, Daegu, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 4Division of Cardiology, Department of Internal Medicine Gwangju Veterans Hospital, Gwangju, Korea.
- KMID: 2344444
- DOI: http://doi.org/10.4070/kcj.2016.46.3.315
Abstract
- BACKGROUND AND OBJECTIVES
The clinical implication of high-degree (second- and third-degree) atrioventricular block (HAVB) complicating ST-segment elevation myocardial infarction (STEMI) is ripe for investigation in this era of primary percutaneous coronary intervention (PCI). We sought to address the incidence, predictors and prognosis of HAVB according to the location of infarct in STEMI patients treated with primary PCI.
SUBJECTS AND METHODS
A total of 16536 STEMI patients (anterior infarction: n=9354, inferior infarction: n=7692) treated with primary PCI were enrolled from a multicenter registry. We compared in-hospital mortality between patients with HAVB and those without HAVB with anterior or inferior infarction, separately. Multivariate analyses were performed to unearth predictors of HAVB and to identify whether HAVB is independently associated with in-hospital mortality.
RESULTS
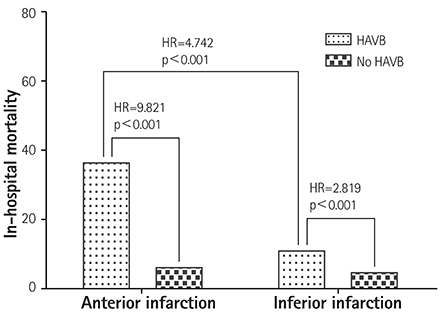
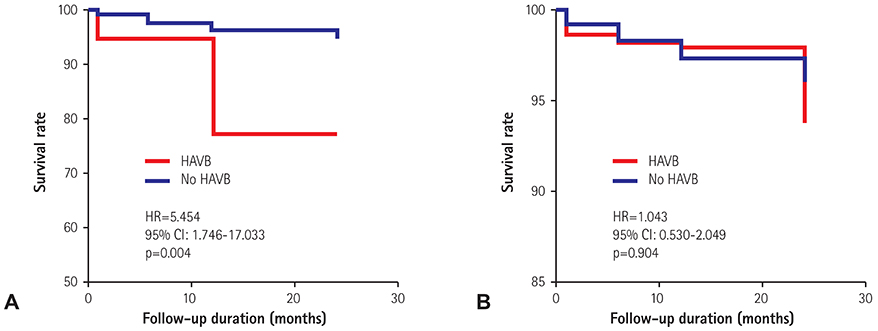
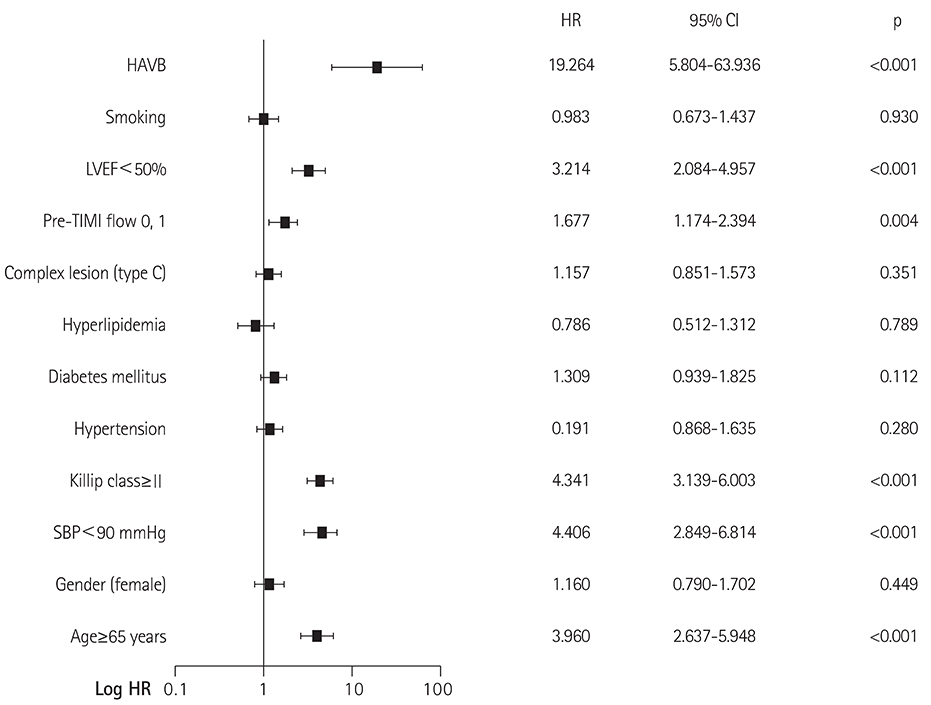
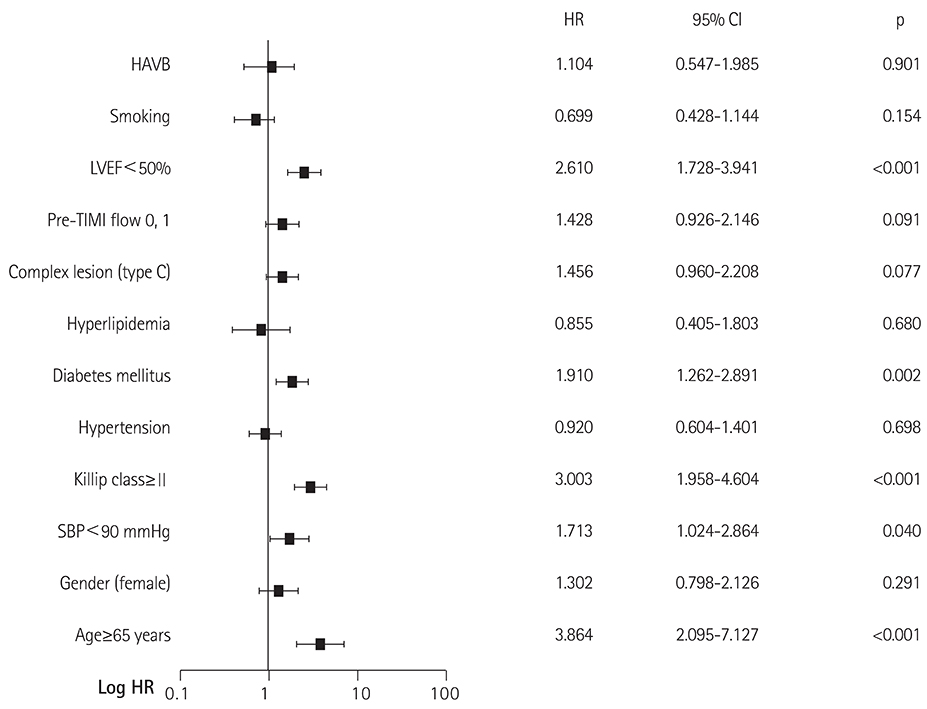
STEMI patients with HAVB showed higher in-hospital mortality than those without HAVB in both anterior (hazard ratio [HR]=9.821, 95% confidence interval [CI]: 4.946-19.503, p<0.001) and inferior infarction (HR=2.819, 95% CI: 2.076-3.827, p<0.001). In multivariate analyses, HAVB was associated with increased in-hospital mortality in anterior myocardial infarction (HR=19.264, 95% CI: 5.804-63.936, p<0.001). However, HAVB in inferior infarction was not an independent predictor of increased in-hospital mortality (HR=1.014, 95% CI: 0.547-1.985, p=0.901).
CONCLUSION
In this era of primary PCI, the prognostic impact of HAVB is different according to the location of infarction. Because of recent improvements in reperfusion strategy, the negative prognostic impact of HAVB in inferior STEMI is no longer prominent.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Clinical Significance of Low-flow Time in Patients Treated with Extracorporeal Cardiopulmonary Resuscitation
Jeong Hoon Yang
Korean Circ J. 2018;48(8):716-718. doi: 10.4070/kcj.2018.0187.Association between Myocardial Infarction Location and In-Hospital Mortality in Iran: A Nationwide Study
Mohammad Shahbaz, Seyed Saeed Hashemi Nazari, Amineh Salehipour, Roya Karimi
Cardiovasc Prev Pharmacother. 2021;3(4):124-133. doi: 10.36011/cpp.2021.3.e16.
Reference
-
1. Goldberg RJ, Zevallos JC, Yarzebski J, et al. Prognosis of acute myocardial infarction complicated by complete heart block (the Worcester Heart Attack Study). Am J Cardiol. 1992; 69:1135–1141.2. Meine TJ, Al-Khatib SM, Alexander JH, et al. Incidence, predictors, and outcomes of high-degree atrioventricular block complicating acute myocardial infarction treated with thrombolytic therapy. Am Heart J. 2005; 149:670–674.3. Aplin M, Engstrom T, Vejlstrup NG, Clemmensen P, Torp-Pedersen C, Køber L. Prognostic importance of complete atrioventricular block complicating acute myocardial infarction. Am J Cardiol. 2003; 92:853–856.4. Gang UJ, Hvelplund A, Pedersen S, et al. High-degree atrioventricular block complicating ST-segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. Europace. 2012; 14:1639–1645.5. Harpaz D, Behar S, Gottlieb S, Boyko V, Kishon Y, Eldar M. Complete atrioventricular block complicating acute myocardial infarction in the thrombolytic era. SPRINT Study Group and the Israeli Thrombolytic Survey Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. J Am Coll Cardiol. 1999; 34:1721–1728.6. Berger PB, Ruocco NA Jr, Ryan TJ, Frederick MM, Jacobs AK, Faxon DP. Incidence and prognostic implications of heart block complicating inferior myocardial infarction treated with thrombolytic therapy: results from TIMI II. J Am Coll Cardiol. 1992; 20:533–540.7. Clemmensen P, Bates ER, Califf RM, et al. Complete atrioventricular block complicating inferior wall acute myocardial infarction treated with reperfusion therapy. TAMI Study Group. Am J Cardiol. 1991; 67:225–230.8. Sgarbossa EB, Pinski SL, Topol EJ, et al. Acute myocardial infarction and complete bundle branch block at hospital admission: clinical characteristics and outcome in the thrombolytic era. GUSTO-I Investigators. Global Utilization of Streptokinase and t-PA [tissue-type plasminogen activator] for Occluded Coronary Arteries. J Am Coll Cardiol. 1998; 31:105–110.9. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013; 82:E1–E27.10. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035.11. Rathore SS, Gersh BJ, Berger PB, et al. Acute myocardial infarction complicated by heart block in the elderly: prevalence and outcomes. Am Heart J. 2001; 141:47–54.12. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators. N Engl J Med. 1993; 329:673–682.13. Hindman MC, Wagner GS. The clinical significance of bundle branch block complicating acute myocardial infarction. 1. Clinical characteristics, hospital mortality, and one-year follow-up. Circulation. 1978; 58:679–688.14. Feigl D, Ashkenazy J, Kishon Y. Early and late atrioventricular block in acute inferior myocardial infarction. J Am Coll Cardiol. 1984; 4:35–38.15. Berger PB, Ryan TJ. Inferior myocardial infarction. High-risk subgroups. Circulation. 1990; 81:401–411.16. Nicod P, Gilpin E, Dittrich H, Polikar R, Henning H, Ross J Jr. Long-term outcome in patients with inferior myocardial infarction and complete atrioventricular block. J Am Coll Cardiol. 1988; 12:589–594.17. Behar S, Zissman E, Zion M, et al. Complete atrioventricular block complicating inferior acute wall myocardial infarction: short- and long-term prognosis. Am Heart J. 1993; 125:1622–1627.18. Abidov A, Kaluski E, Hod H, et al. Influence of conduction disturbances on clinical outcome in patients with acute myocardial infarction receiving thrombolysis (results from the ARGAMI-2 study). Am J Cardiol. 2004; 93:76–80.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ST segment
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Treatment delay and outcomes of ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention during the COVID-19 era in South Korea
- Consecutive Multivessel Myocardial Infarction during Primary Percutaneous Coronary Intervention
- A Case of Coronary Artery Dissection after Blunt Chest Trauma Resulting in ST-Segment Elevation Myocardial Infarction