Korean Circ J.
2016 Jul;46(4):507-514. 10.4070/kcj.2016.46.4.507.
Thirty-Year Trends in Mortality from Cerebrovascular Diseases in Korea
- Affiliations
-
- 1Department of Public Health, Yonsei University Graduate School, Seoul, Korea.
- 2Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea. hckim@yuhs.ac
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2344425
- DOI: http://doi.org/10.4070/kcj.2016.46.4.507
Abstract
- BACKGROUND AND OBJECTIVES
Cerebrovascular disease is a leading cause of mortality and morbidity in Korea. Understanding of cerebrovascular disease mortality trends is important to reduce the health burden from cerebrovascular diseases. We examined the changing pattern of mortality related to cerebrovascular disease in Korea over 30 years from 1983 to 2012.
SUBJECTS AND METHODS
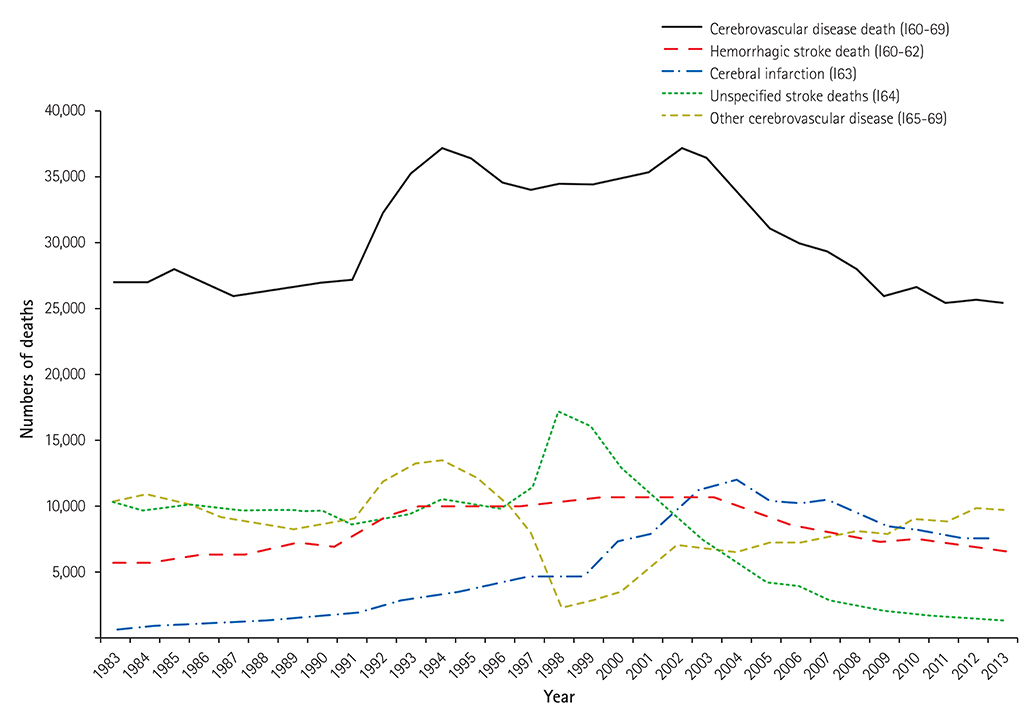
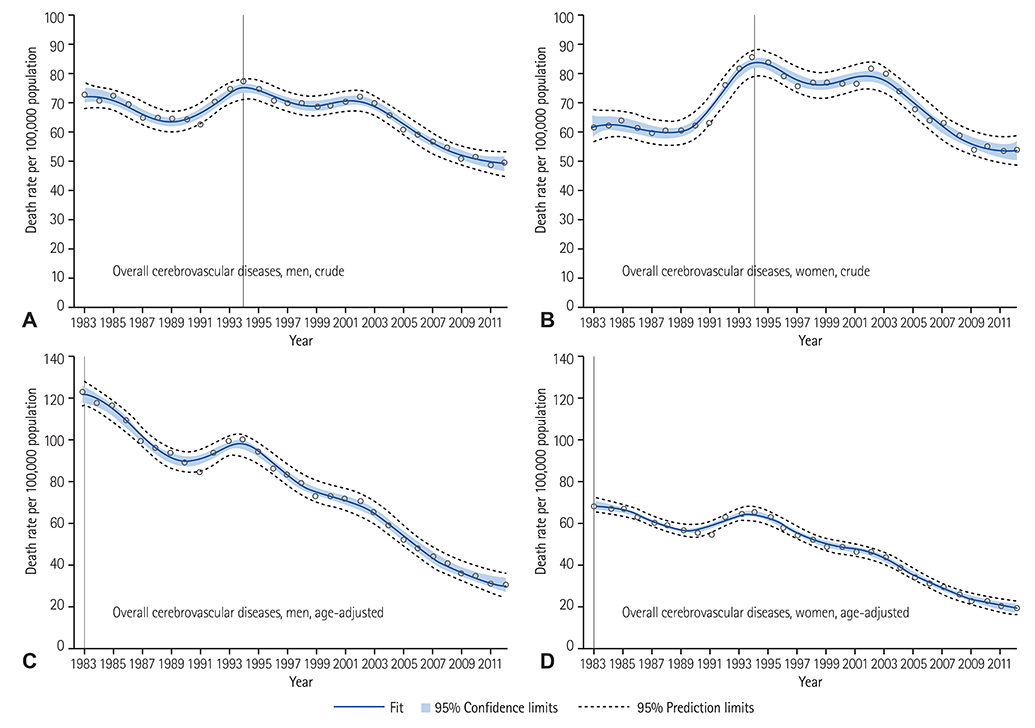
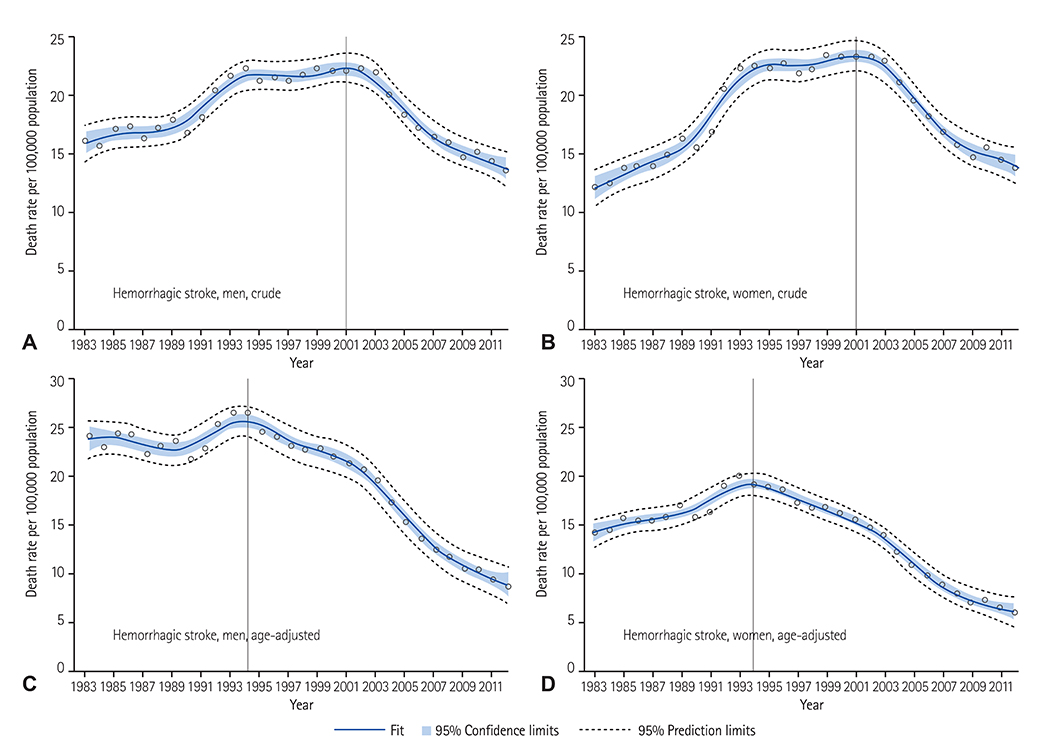
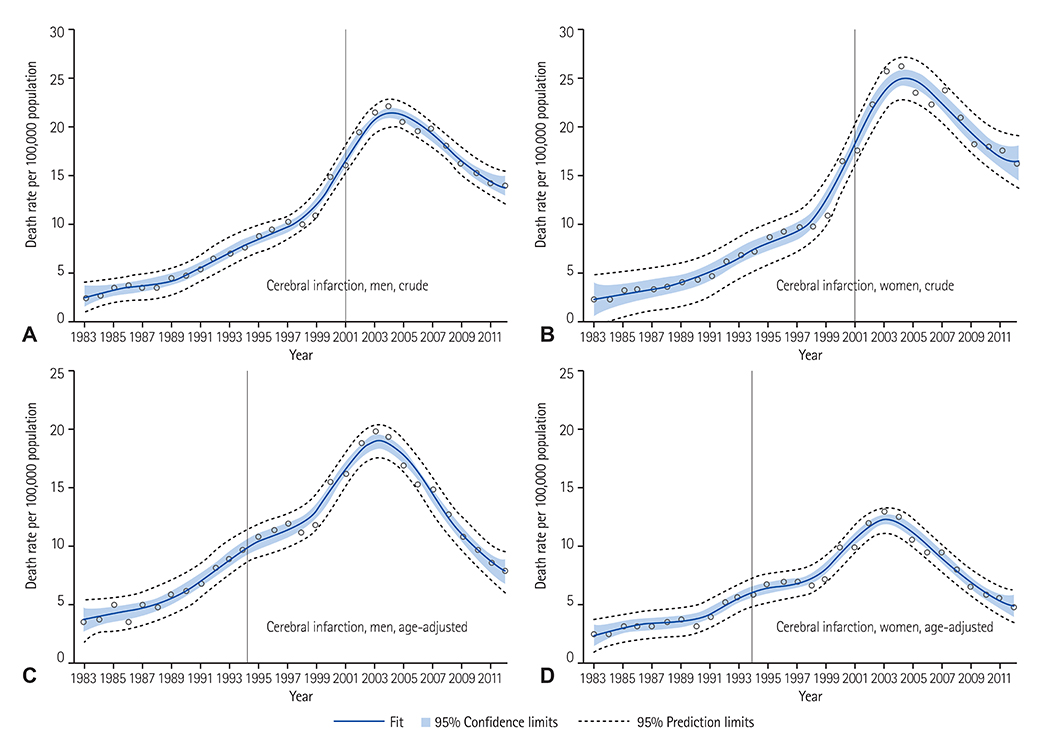
Numbers of deaths from cerebrovascular disease, hemorrhagic stroke, and cerebral infarction were obtained from the national Cause of Death Statistics. Crude and age-adjusted mortality rates were calculated for men and women for each year. Penalized B-spline methods, which reduce bias and variability in curve fitting, were used to identify the trends of 30-year mortality and identify the year of highest mortality.
RESULTS
During the 30 years, cerebrovascular disease mortality has markedly declined. The age-adjusted cerebrovascular disease mortality rate has decreased by 78% in men and by 68% in women. In the case of hemorrhagic stroke, crude mortality peaked in 2001 but age-adjusted mortality peaked in 1994. Between 1994 and 2012, age-adjusted mortality from hemorrhagic stroke has decreased by 68% in men and 59% in women. In the case of cerebral infarction, crude and age-adjusted mortality rates steeply increased until 2004 and 2003, respectively, and both rates decreased rapidly thereafter.
CONCLUSION
Cerebrovascular disease mortality rate has significantly decreased over the last 30 years in Korea, but remains a health burden. The prevalence of major cardiovascular risk factors are still highly prevalent in Korea.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Epidemiology of dyslipidemia in Korea
Hyeon Chang Kim
J Korean Med Assoc. 2016;59(5):352-357. doi: 10.5124/jkma.2016.59.5.352.Korea Heart Disease Fact Sheet 2020: Analysis of Nationwide Data
Hyeok-Hee Lee, So Mi Jemma Cho, Hokyou Lee, Jongmin Baek, Jang-Ho Bae, Wook-Jin Chung, Hyeon Chang Kim
Korean Circ J. 2021;51(6):495-503. doi: 10.4070/kcj.2021.0097.Prevalence and Clinical Characteristics of Dyslipidemia in Koreans
Jee-Sun Jeong, Hyuk-Sang Kwon
Endocrinol Metab. 2017;32(1):30-35. doi: 10.3803/EnM.2017.32.1.30.Trends in Mortality from Hemorrhagic Stroke in Korea from 2012 to 2020
Kwang-Chun Cho, Hasung Kim, Sang Hyun Suh
Neurointervention. 2022;17(2):87-92. doi: 10.5469/neuroint.2022.00220.
Reference
-
1. Deaton C, Froelicher ES, Wu LH, Ho C, Shishani K, Jaarsma T. The global burden of cardiovascular disease. Eur J Cardiovasc Nurs. 2011; 10:Suppl 2. S5–S13.2. Hong KS, Bang OY, Kang DW, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean stroke society and clinical research center for stroke. J Stroke. 2013; 15:2–20.3. Lee KS, Park JH. Burden of disease in Korea during 2000-10. J Public Health (Oxf). 2014; 36:225–234.4. Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014; 174:64–72.5. Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. Eur J Cardiovasc Prev Rehabil. 2009; 16:333–350.6. Sarti C, Rastenyte D, Cepaitis Z, Tuomilehto J. International trends in mortality from stroke, 1968 to 1994. Stroke. 2000; 31:1588–1601.7. Towfighi A, Saver JL. Stroke declines from third to fourth leading cause of death in the United States: historical perspective and challenges ahead. Stroke. 2011; 42:2351–2355.8. Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015; 45:202–209.9. Costa MJ. Penalized spline models and applications [dissertation]. Coventry (UK): University of Warwick;2008.10. Mirzaei M, Truswell AS, Arnett K, Page A, Taylor R, Leeder SR. Cerebrovascular disease in 48 countries: secular trends in mortality 1950–2005. J Neurol Neurosurg Psychiatry. 2012; 83:138–145.11. Thom TJ, Epstein FH. Heart disease, cancer, and stroke mortality trends and their interrelations. An international perspective. Circulation. 1994; 90:574–582.12. Klag MJ, Whelton PK, Seidler AJ. Decline in US stroke mortality. Demographic trends and antihypertensive treatment. Stroke. 1989; 20:14–21.13. Suh I. Cardiovascular mortality in Korea: a country experiencing epidemiologic transition. Acta Cardiol. 2001; 56:75–81.14. Garraway WM, Whisnant JP, Drury I. The continuing decline in the incidence of stroke. Mayo Clin Proc. 1983; 58:520–523.15. Harmsen P, Tsipogianni A, Wilhelmsen L. Stroke incidence rates were unchanged, while fatality rates declined, during 1971-1987 in Göteborg, Sweden. Stroke. 1992; 23:1410–1415.16. Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014; 45:315–353.17. Carter KN, Anderson CS, Hackett ML, Barber PA, Bonita R. Auckland Regional Community Stroke Study Group. Improved survival after stroke: is admission to hospital the major explanation? Trend analyses of the Auckland Regional Community Stroke Studies. Cerebrovasc Dis. 2007; 23:162–168.18. Kannel WB. Framingham study insights into hypertensive risk of cardiovascular disease. Hypertens Res. 1995; 18:181–196.19. Neaton JD, Wentworth DN, Cutler J, Stamler J, Kuller L. Risk factors for death from different types of stroke. Multiple Risk Factor Intervention Trial Research Group. Ann Epidemiol. 1993; 3:493–499.20. O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010; 376:112–123.21. Kim HC, Oh SM. Noncommunicable diseases: current status of major modifiable risk factors in Korea. J Prev Med Public Health. 2013; 46:165–172.22. Park TH, Kim MK, Lee KB, et al. Population attributable risk of major risk factors for ischemic stroke in the Korean population. Korean J Stroke. 2008; 10:125–133.23. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–1913.24. Bonita R, Beaglehole R. Increased treatment of hypertension does not explain the decline in stroke mortality in the United States, 1970-1980. Hypertension. 1989; 13:5 Suppl. I69–I73.25. Thijs L, Fagard R, Lijnen P, Staessen J, Van Hoof R, Amery A. A meta-analysis of outcome trials in elderly hypertensives. J Hypertens. 1992; 10:1103–1109.26. Lever AF, Ramsay LE. Treatment of hypertension in the elderly. J Hypertens. 1995; 13:571–579.27. Ní Chróinín D, Asplund K, Åsberg S, et al. Statin therapy and outcome after ischemic stroke: systematic review and meta-analysis of observational studies and randomized trials. Stroke. 2013; 44:448–456.28. Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014; 312:259–268.29. Jung KH, Lee SH, Kim BJ, et al. Secular trends in ischemic stroke characteristics in a rapidly developed country: results from the Korean Stroke Registry Study (secular trends in Korean stroke). Circ Cardiovasc Qual Outcomes. 2012; 5:327–334.30. Won TY, Kang BS, Im TH, Choi HJ. The study of accuracy of death statistics. J Korean Soc Emerg Med. 2007; 18:256–262.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thirty-six Year Trends in Mortality from Diseases of Circulatory System in Korea
- Thirty-Year Trends in Mortality from Cardiovascular Diseases in Korea
- The Proportional Mortality Ratios of Specific-cause Mortality by Occupation and Education among Men Aged 20-64 in Korea (1993-2004)
- Trends in the Leading Causes of Death in Korea, 1983-2012
- Age-period-cohort Analysis of Cardiovascular Disease Mortality in Japan, 1995-2018