Korean Circ J.
2016 Jul;46(4):490-498. 10.4070/kcj.2016.46.4.490.
Long-Term Clinical Outcomes of Transient and Persistent No Reflow Phenomena following Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea. cecilyk@hanmail.net
- 2Department of Cardiology, Seoul St Mary's Hospital, The Catholic University School of Medicine, Seoul, Korea.
- KMID: 2344423
- DOI: http://doi.org/10.4070/kcj.2016.46.4.490
Abstract
- BACKGROUND AND OBJECTIVES
There is limited information on the transient or persistent no reflow phenomenon in patients with acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI).
SUBJECTS AND METHODS
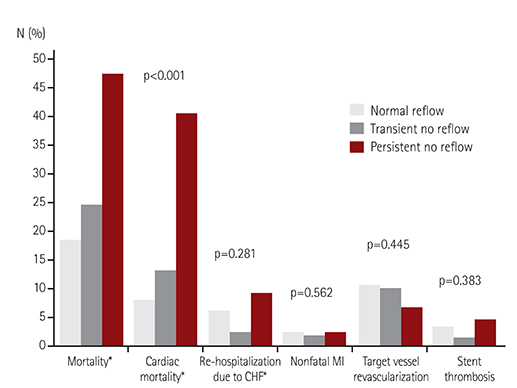
The study analyzed 4329 patients with AMI from a Korean multicenter registry who underwent PCI using coronary stents (2668 ST-elevation and 1661 non-ST-elevation myocardial infarction [MI] patients): 4071 patients without any no reflow, 213 with transient no reflow (no reflow with final thrombolysis in myocardial infarction [TIMI] flow grade 3), and 45 with persistent no reflow (no reflow with final TIMI flow grade≤2). The primary endpoint was all-cause mortality during 3-year follow-up. We also analyzed the incidence of cardiac mortality, non-fatal MI, re-hospitalization due to heart failure, target vessel revascularization, and stent thrombosis.
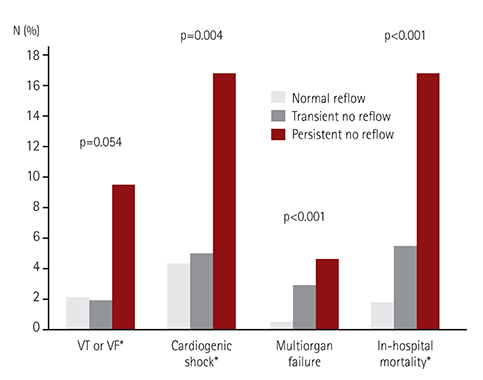
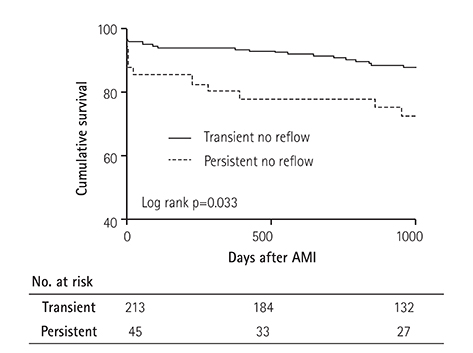
RESULTS
The persistent no reflow group was associated with higher all-cause mortality (hazard ratio [HR] 1.98, 95% confidence interval [CI] 1.08-3.65, p=0.028) and cardiac mortality (HR 3.28, 95% CI 1.54-6.95, p=0.002) compared with the normal reflow group. Transient no reflow increased all-cause mortality only when compared with normal reflow group (HR 1.58, 95% CI 1.11-2.24, p=0.010). When comparing transient and persistent no reflow, persistent no reflow was associated with increased all-cause mortality (46.7 vs. 24.4%, log rank p=0.033).
CONCLUSION
The persistent no reflow phenomenon was associated with a poor in-hospital outcome and increased long-term mortality mainly driven by increased cardiac mortality compared to the transient no reflow phenomenon or normal reflow.
MeSH Terms
Figure
Reference
-
1. Jaffe R, Charron T, Puley G, Dick A, Strauss BH. Microvascular obstruction and the no-reflow phenomenon after percutaneous coronary intervention. Circulation. 2008; 117:3152–3156.2. Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009; 54:281–292.3. Morishima I, Sone T, Okumura K, et al. Angiographic no-reflow phenomenon as a predictor of adverse long-term outcome in patients treated with percutaneous transluminal coronary angioplasty for first acute myocardial infarction. J Am Coll Cardiol. 2000; 36:1202–1209.4. Ndrepepa G, Tiroch K, Keta D, et al. Predictive factors and impact of no reflow after primary percutaneous coronary intervention in patients with acute myocardial infarction. Circ Cardiovasc Interv. 2010; 3:27–33.5. Ndrepepa G, Tiroch K, Fusaro M, et al. 5-year prognostic value of no-reflow phenomenon after percutaneous coronary intervention in patients with acute myocardial infarction. J Am Coll Cardiol. 2010; 55:2383–2389.6. Brosh D, Assali AR, Mager A, et al. Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on six-month mortality. Am J Cardiol. 2007; 99:442–445.7. Harrison RW, Aggarwal A, Ou FS, et al. Incidence and outcomes of no-reflow phenomenon during percutaneous coronary intervention among patients with acute myocardial infarction. Am J Cardiol. 2013; 111:178–184.8. Mehta RH, Harjai KJ, Boura J, et al. Prognostic significance of transient no-reflow during primary percutaneous coronary intervention for ST-elevation acute myocardial infarction. Am J Cardiol. 2003; 92:1445–1447.9. Lee CH, Wong HB, Tan HC, et al. Impact of reversibility of no reflow phenomenon on 30-day mortality following percutaneous revascularization for acute myocardial infarction-insights from a 1,328 patient registry. J Interv Cardiol. 2005; 18:261–266.10. Chan W, Stub D, Clark DJ, et al. Usefulness of transient and persistent no reflow to predict adverse clinical outcomes following percutaneous coronary intervention. Am J Cardiol. 2012; 109:478–485.11. Jinnouchi H, Sakakura K, Wada H, et al. Transient no reflow following primary percutaneous coronary intervention. Heart Vessels. 2014; 29:429–436.12. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002; 39:2 Suppl 1. S1–S266.13. The TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial: phase 1 findings. N Engl J Med. 1985; 312:932–936.14. Khattab AA, Hamm CW, Senges J, et al. Prognostic value of the modified American College of Cardiology/American Heart Association lesion morphology classification for clinical outcome after sirolimus-eluting stent placement (results of the prospective multicenter German Cypher Registry). Am J Cardiol. 2008; 101:477–482.15. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.16. Abbo KM, Dooris M, Glazier S, et al. Features and outcome of no-reflow after percutaneous coronary intervention. Am J Cardiol. 1995; 75:778–782.17. Al Suwaidi J, Holmes DR Jr, Salam AM, Lennon R, Berger PB. Impact of coronary artery stents on mortality and nonfatal myocardial infarction: meta-analysis of randomized trials comparing a strategy of routine stenting with that of balloon angioplasty. Am Heart J. 2004; 147:815–822.18. Claessen BE, Smits PC, Kereiakes DJ, et al. Impact of lesion length and vessel size on clinical outcomes after percutaneous coronary intervention with everolimus- versus paclitaxel-eluting stents: pooled analysis from the SPIRIT (clinical evaluation of the XIENCE V everolimus eluting coronary stent system) and COMPARE (second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice) randomized trials. JACC Cardiovasc Interv. 2011; 4:1209–1215.19. Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010; 121:1235–1243.20. Brodie B, Pokharel Y, Garg A, et al. Predictors of early, late, and very late stent thrombosis after primary percutaneous coronary intervention with bare-metal and drug-eluting stents for ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2012; 5:1043–1051.21. Hong SN, Ahn Y, Hwang SH, et al. Usefulness of preprocedural N-terminal pro-brain natriuretic peptide in predicting angiographic no-reflow phenomenon during stent implantation in patients with ST-segment elevation acute myocardial infarction. Am J Cardiol. 2007; 100:631–634.22. Jeong YH, Kim WJ, Park DW, et al. Serum B-type natriuretic peptide on admission can predict the 'no-reflow' phenomenon after primary drug-eluting stent implantation for ST-segment elevation myocardial infarction. Int J Cardiol. 2010; 141:175–181.23. Magro M, Nauta ST, Simsek C, et al. Usefulness of the SYNTAX score to predict "no reflow" in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol. 2012; 109:601–606.24. Wu X, Mintz GS, Xu K, et al. The relationship between attenuated plaque identified by intravascular ultrasound and no-reflow after stenting in acute myocardial infarction: the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) trial. JACC Cardiovasc Interv. 2011; 4:495–502.25. Hong YJ, Jeong MH, Choi YH, et al. Impact of plaque components on no-reflow phenomenon after stent deployment in patients with acute coronary syndrome: a virtual histology-intravascular ultrasound analysis. Eur Heart J. 2011; 32:2059–2066.26. Iijima R, Shinji H, Ikeda N, et al. Comparison of coronary arterial finding by intravascular ultrasound in patients with "transient no-reflow" versus "reflow" during percutaneous coronary intervention in acute coronary syndrome. Am J Cardiol. 2006; 97:29–33.27. Alhadramy O, Westerhout CM, Brener SJ, Granger CB, Armstrong PW. APEX AMI Investigators. Is visual interpretation of coronary epicardial flow reliable in patients with ST-elevation myocardial infarction undergoing primary angioplasty? Insights from the angiographic substudy of the Assessment of Pexelizumab in Acute Myocardial Infarction (APEX-AMI) trial. Am Heart J. 2010; 159:899–904.28. Brener SJ, Moliterno DJ, Aylward PE, et al. Reperfusion after primary angioplasty for ST-elevation myocardial infarction: predictors of success and relationship to clinical outcomes in the APEX-AMI angiographic study. Eur Heart J. 2008; 29:1127–1135.29. Brener SJ, Cristea E, Lansky AJ, Fahy M, Mehran R, Stone GW. Operator versus core laboratory assessment of angiographic reperfusion markers in patients undergoing primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2012; 5:563–569.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- Percutaneous Cardiopulmonary Support in Refractory No-Reflow with Cardiogenic Shock after Coronary Stenting in Acute Myocardial Infarction
- Acute Profound Thrombocytopenia after Using Abciximab for No-Reflow during Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction
- Coronary Flow Doppler Profile in No-Reflex Phenomenon after Direct PTCA in Acute Myocardial Infarction
- The Effect of Intra-coronary Nicorandil Prior to Reperfusion in Acute ST Segment Elevation Myocardial Infarction