J Korean Ophthalmol Soc.
2015 Jun;56(6):917-924. 10.3341/jkos.2015.56.6.917.
The Effect of Intravitreal Bevacizumab Injection before Trabeculectomy in Patients with Neovascular Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, Keimyung University School of Medicine, Daegu, Korea. changsd@dsmc.or.kr
- KMID: 2339158
- DOI: http://doi.org/10.3341/jkos.2015.56.6.917
Abstract
- PURPOSE
To evaluate the efficacy of preoperative intravitreal bevacizumab injection (IVBI) and prognostic factors of surgical success in neovascular glaucoma patients, who underwent trabeculectomy.
METHODS
A total of 58 patients (58 eyes) diagnosed with neovascular glaucoma who underwent trabeculectomy between 2003 and 2013 were enrolled in this retrospective study. Trabeculectomy with mitomycin C was performed between 2003 and 2006 and additional preoperative IVBI with the above mentioned technique was performed between 2007 and 2013. To evaluate the efficacy of preoperative IVBI, the patients were divided into the preoperative IVBI group and control group. Best corrected visual acuity (BCVA) and intraocular pressure (IOP) were measured from preoperative to postoperative 12 months. To evaluate the prognostic factors related to surgical success, the following was investigated: age, lens status, preoperative IVBI, time interval between preoperative IVBI and trabeculectomy, previous vitrectomy and, postoperative complications.
RESULTS
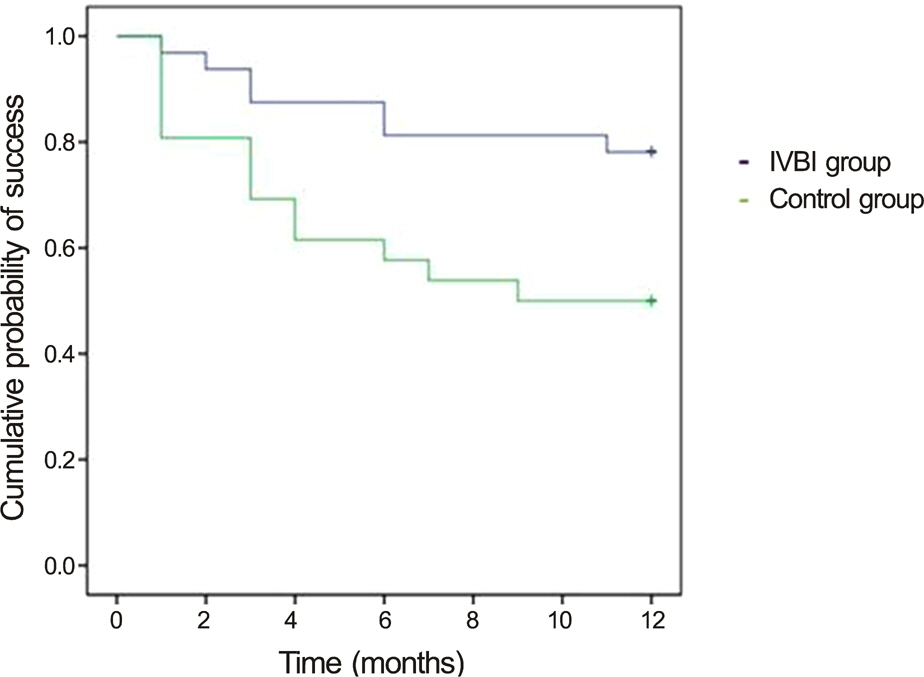
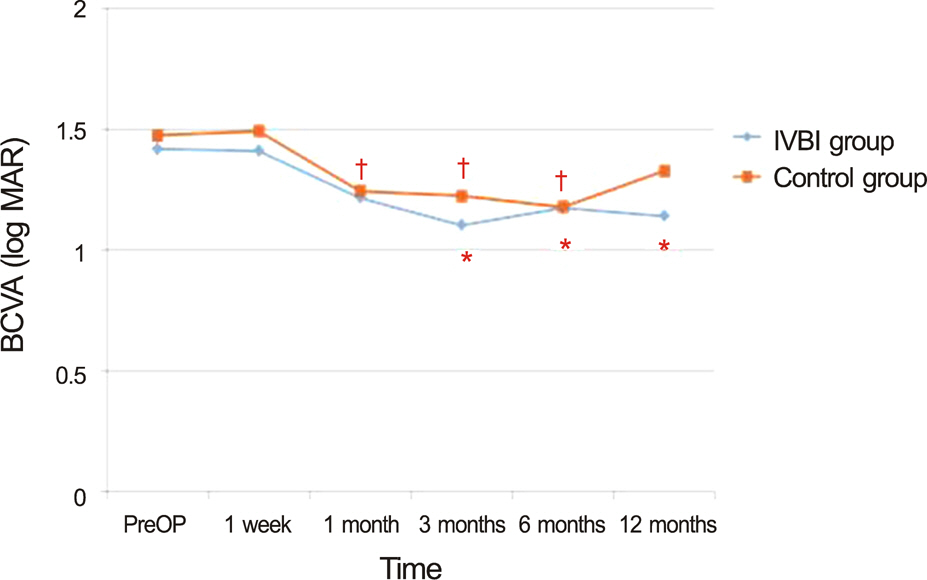
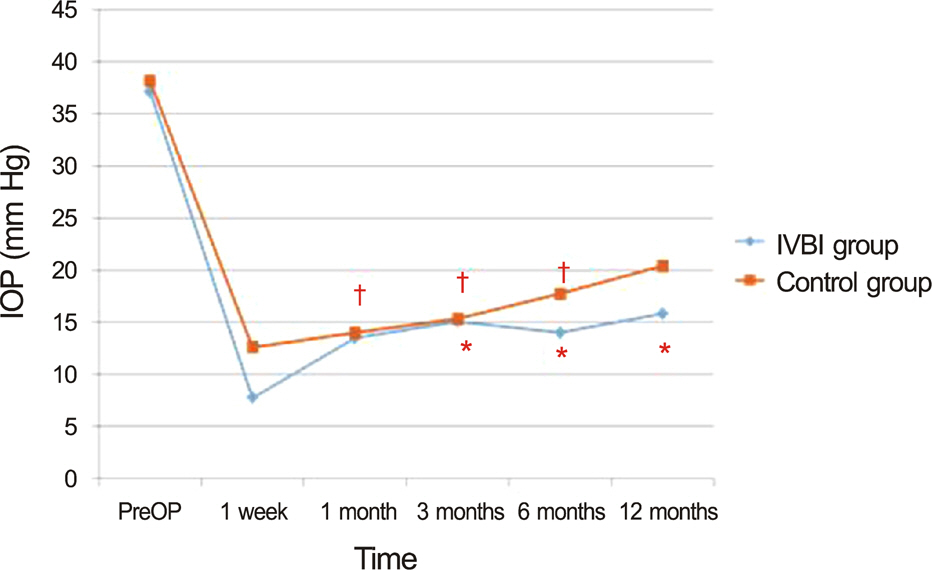
Trabeculectomy with mitomycin C only was performed in 26 eyes and additional preoperative IVBI was performed in 32 eyes. Surgical success was 81.3% in the IVBI group and 57.7% in the control group at postoperative 6 months (p = 0.012), and 78.1% in the IVBI group and 50.0% in the control group at postoperative 12 months (p = 0.021). Statistically significant IOP reduction effect was observed in the IVBI group (p = 0.048), and reduced anti-glaucoma eye drop usage was observed in the IVBI group (0.4) compared with 0.8 in the control group (p = 0.040). Postoperative hyphema (hazard ratio [HR] = 2.872, p = 0.044) and preoperative IVBI (HR = 0.280, p = 0.030) were considered risk factors for surgical failure in univariate analysis, however, only preoperative IVBI was statistically significant in multivariate analysis (p = 0.046).
CONCLUSIONS
In neovascular glaucoma patients, preoperative IVBI before trabeculectomy is a good prognostic factor of surgical success and shows benefit in lowering the IOP and reducing anti-glaucoma eye drop usage at postoperative 1 year.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Intravitreal Bevacizumab and Subsequent Trabeculectomy with Mitomycin C for Neovascular Glaucoma with Previous Sutureless Vitrectomy
Keun Heung Park, Hyo Chul Lim, Ji Woong Lee
J Korean Ophthalmol Soc. 2016;57(4):607-613. doi: 10.3341/jkos.2016.57.4.607.
Reference
-
References
1. Kotecha A, Spratt A, Ogunbowale L, et al. Intravitreal bevacizumab in refractory neovascular glaucoma: a prospective, observational case series. Arch Ophthalmol. 2011; 129:145–50.2. Olmos LC, Lee RK. Medical and surgical treatment of neovascular glaucoma. Int Ophthalmol Clin. 2011; 51:27–36.
Article3. Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994; 331:1480–7.
Article4. Brown GC, Magargal LE, Schachat A, Shah H. Neovascular glaucoma. Etiologic considerations. Ophthalmology. 1984; 91:315–20.5. Tripathi RC, Li J, Tripathi BJ, et al. Increased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucoma. Ophthalmology. 1998; 105:232–7.
Article6. Cashwell LF, Marks WP. Panretinal photocoagulation in the management of neovascular glaucoma. South Med J. 1988; 81:1364–8.
Article7. Mandal AK, Majji AB, Mandal SP, et al. Mitomycin-C-augmented trabeculectomy for neovascular glaucoma. A preliminary report. Indian J Ophthalmol. 2002; 50:287–93.8. Kiuchi Y, Sugimoto R, Nakae K, et al. Trabeculectomy with mitomycin C for treatment of neovascular glaucoma in diabetic patients. Ophthalmologica. 2006; 220:383–8.
Article9. Silva Paula J, Jorge R, Alves Costa R, et al. Short-term results of intravitreal bevacizumab (Avastin) on anterior segment neovascularization in neovascular glaucoma. Acta Ophthalmol Scand. 2006; 84:556–7.
Article10. Iliev ME, Domig D, Wolf-Schnurrbursch U, et al. Intravitreal bevacizumab (Avastin) in the treatment of neovascular glaucoma. Am J Ophthalmol. 2006; 142:1054–6.
Article11. Yazdani S, Hendi K, Pakravan M, et al. Intravitreal bevacizumab for neovascular glaucoma: a randomized controlled trial. J Glaucoma. 2009; 18:632–7.12. Wakabayashi T, Oshima Y, Sakaguchi H, et al. Intravitreal bevacizumab to treat iris neovascularization and neovascular glaucoma secondary to ischemic retinal diseases in 41 consecutive cases. Ophthalmology. 2008; 115:1571–80. 1580.e1-3.
Article13. Nakatake S, Yoshida S, Nakao S, et al. Hyphema is a risk factor for failure of trabeculectomy in neovascular glaucoma: a retrospective analysis. BMC Ophthalmol. 2014; 14:55.
Article14. Saito Y, Higashide T, Takeda H, et al. Beneficial effects of pre-operative intravitreal bevacizumab on trabeculectomy outcomes in neovascular glaucoma. Acta Ophthalmol. 2010; 88:96–102.
Article15. Alkawas AA, Shahien EA, Hussein AM. Management of neovascular glaucoma with panretinal photocoagulation, intravitreal bevacizumab, and subsequent trabeculectomy with mitomycin C. J Glaucoma. 2010; 19:622–6.
Article16. Lee JW, Lai JS, Yick DW, Tse RK. Retrospective case series on the long-term visual and intraocular pressure outcomes of phacomor-phic glaucoma. Eye (Lond). 2010; 24:1675–80.
Article17. Weber PA. Neovascular glaucoma. Current management. Surv Ophthalmol. 1981; 26:149–53.
Article18. Fernández-Vigo J, Castro J, Cordido M, Fernández-Sabugal J. Treatment of diabetic neovascular glaucoma by panretinal ablation and trabeculectomy. Acta Ophthalmol (Copenh). 1988; 66:612–6.
Article19. Parrish R, Herschler J. Eyes with end-stage neovascular glaucoma. Natural history following successful modified filtering operation. Arch Ophthalmol. 1983; 101:745–6.20. Kang JY, Nam KY, Lee SJ, Lee SU. The effect of intravitreal bevacizumab injection before Ahmed valve implantation in patients with neovascular glaucoma. Int Ophthalmol. 2014; 34:793–9.
Article21. Takihara Y, Inatani M, Kawaji T, et al. Combined intravitreal bevacizumab and trabeculectomy with mitomycin C versus trabeculectomy with mitomycin C alone for neovascular glaucoma. J Glaucoma. 2011; 20:196–201.
Article22. Ehlers JP, Spirn MJ, Lam A, et al. Combination intravitreal bevacizumab/panretinal photocoagulation versus panretinal photocoagulation alone in the treatment of neovascular glaucoma. Retina. 2008; 28:696–702.
Article23. Takihara Y, Inatani M, Fukushima M, et al. Trabeculectomy with mitomycin C for neovascular glaucoma: prognostic factors for surgical failure. Am J Ophthalmol. 2009; 147:912–8. 918.e1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Bevacizumab and Subsequent Trabeculectomy with Mitomycin C for Neovascular Glaucoma with Previous Sutureless Vitrectomy
- Effect of Simultaneous Intravitreal Bevacizumab and Retrobulbar Triamcinolone Injection in Refractory Neovascular Glaucoma
- Intraviteal Bevacizumab (Avastin(R)) Injection for the Treatment of Early-Stage Neovascular Glaucoma
- Intravitreal Bevacizumab for the Treatment of Neovascular Glaucoma Associated With Central Retinal Artery Occlusion
- Clinical Course after Intravitreal Bevacizumab Injection in Ischemic Central Retinal Vein Obstruction