J Korean Ophthalmol Soc.
2014 Dec;55(12):1800-1807. 10.3341/jkos.2014.55.12.1800.
Comparison of Continuous Curvilinear Capsulorhexis Parameters between Femtosecond Laser and Conventional Cataract Surgery
- Affiliations
-
- 1Busan Sungmo Eye Hospital, Busan, Korea. hanwave2@gmail.com
- KMID: 2338963
- DOI: http://doi.org/10.3341/jkos.2014.55.12.1800
Abstract
- PURPOSE
To compare parameters of femtosecond laser and manual continuous curvilinear capsulorhexis (CCC) using anterior segment optical coherence tomography (AS-OCT).
METHODS
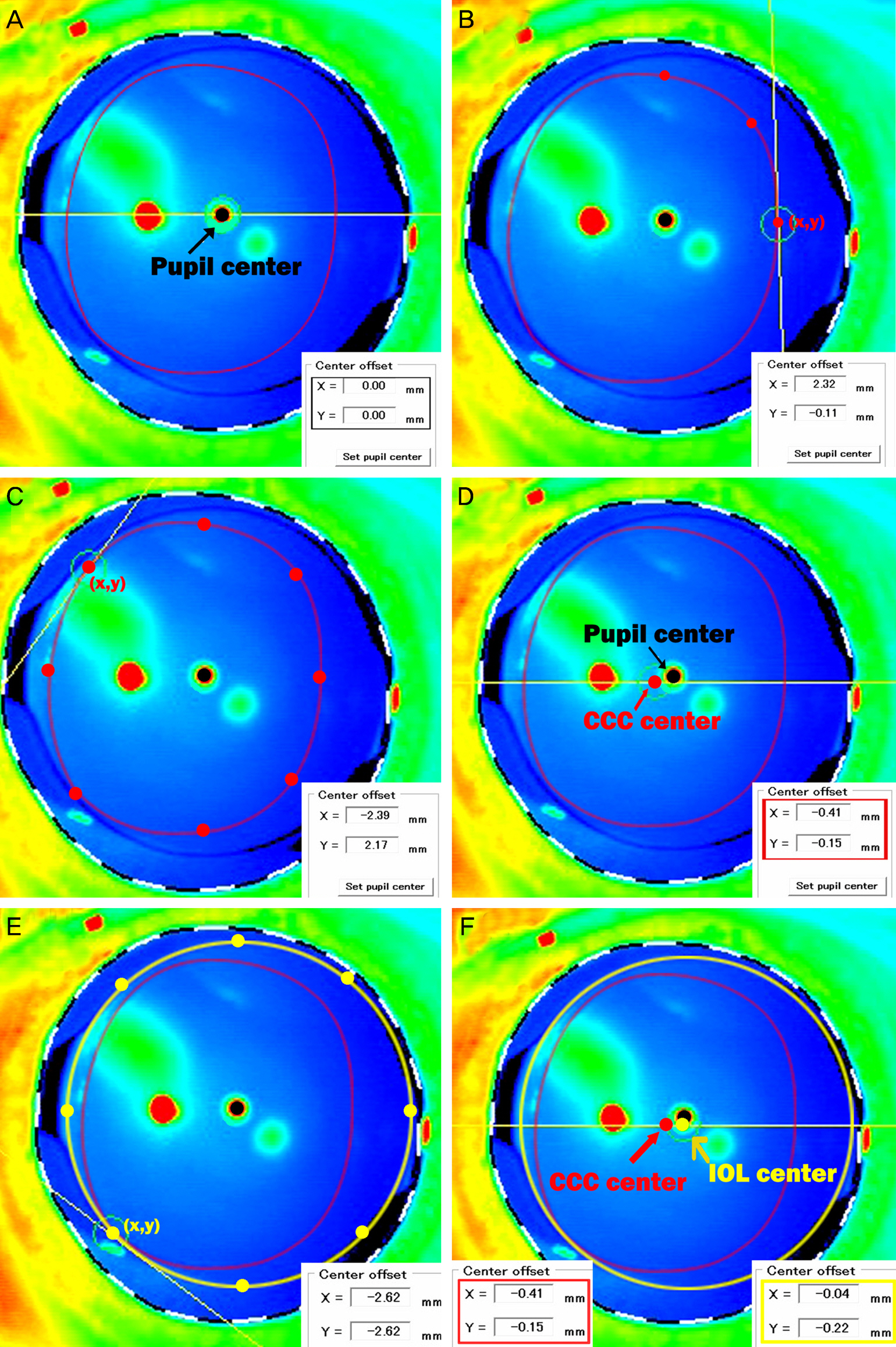
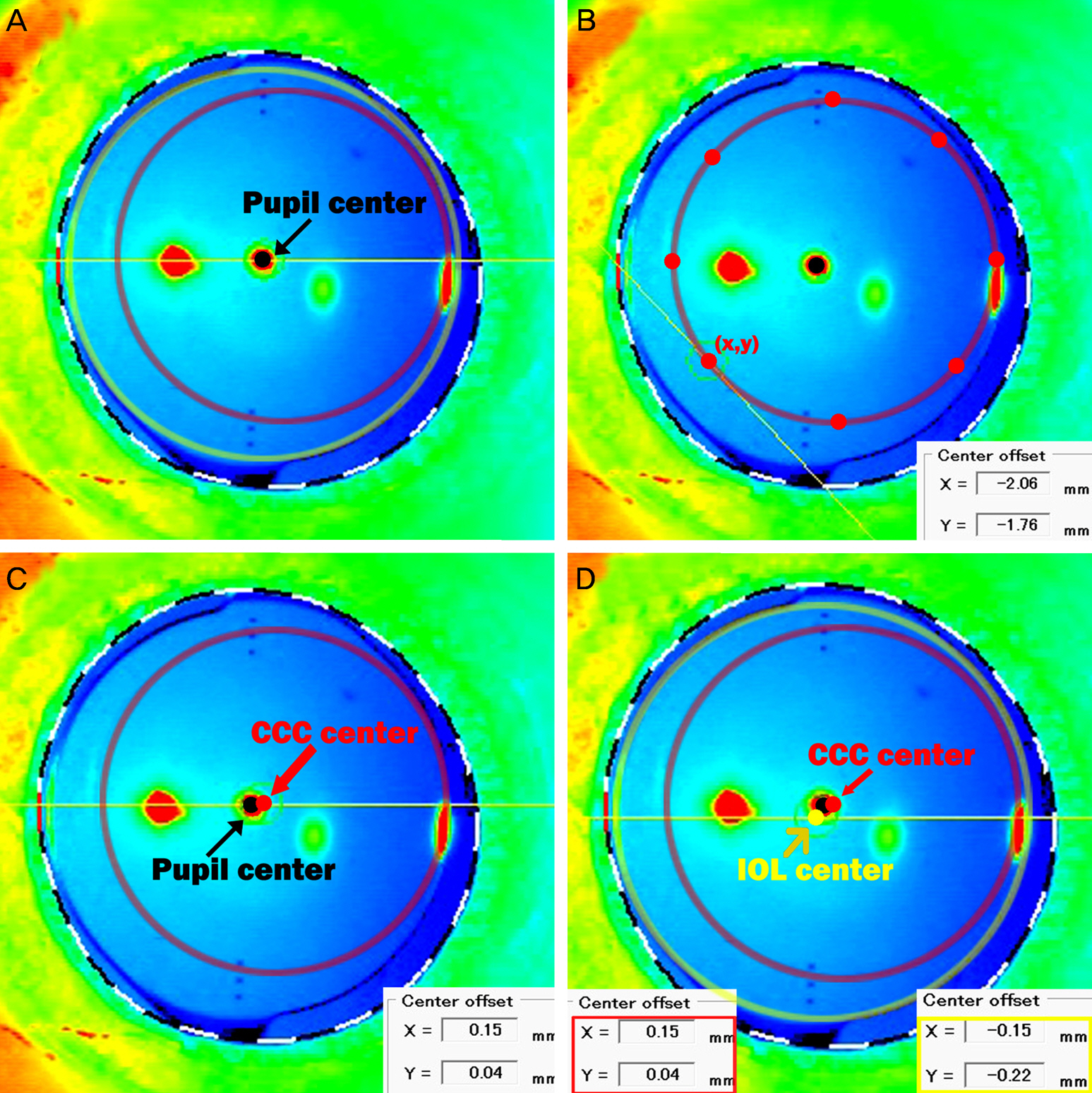
Femtosecond laser cataract surgery was performed in 30 eyes of 30 patients, and conventional cataract surgery with a manual CCC in 30 eyes of 30 patients. One month after surgery, CCC diameters, circularity of capsulotomy, and distance between the CCC and pupil center were analyzed using the AS-OCT.
RESULTS
Mean maximal CCC diameter was 4.96 +/- 0.23 mm in the femtosecond laser group, and 4.70 +/- 0.82 mm in the manual CCC group. Mean minimal CCC diameter was 4.91 +/- 0.23 mm in the femtosecond group, and 4.48 +/- 0.64 mm in the manual CCC group showing significant difference between the two groups (p = 0.000). Circularity of capsulotomy was 0.99 +/- 0.01 in the femtosecond group and 0.91 +/- 0.13 in the manual CCC group and was statistically different between the 2 groups (p = 0.000). The distance from the CCC center to the pupil center was 0.18 +/- 0.09 mm in the femtosecond group and 0.26 +/- 0.17 mm in the manual CCC group. The CCC center was closer to the pupil center in the femtosecond than in the manual CCC group (p = 0.038).
CONCLUSIONS
Properly sized and shaped capsulotomy can be expected in femtosecond laser CCC compared with manual CCC.
Figure
Cited by 2 articles
-
Analysis of Positional Relationships of Various Centers in Cataract Surgery
Woo Keun Song, Jin Ah Lee, Jae Yong Kim, Myoung Joon Kim, Hungwon Tchah
Korean J Ophthalmol. 2019;33(1):70-81. doi: 10.3341/kjo.2018.0085.Comparison of Effective Phacoemulsification Time between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract Surgery
Dong Seob Ahn, Sang Youp Han, Kyung Heon Lee
J Korean Ophthalmol Soc. 2016;57(2):236-242. doi: 10.3341/jkos.2016.57.2.236.
Reference
-
References
1. Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg. 2009; 25:1053–60.
Article2. Ratkay-Traub I, Ferincz IE, Juhasz T, et al. First clinical results with the femtosecond neodynium-glass laser in refractive surgery. J Refract Surg. 2003; 19:94–103.
Article3. Nordan LT, Slade SG, Baker RN, et al. Femtosecond laser flap creation for laser in situ keratomileusis: six-month follow-up of initial U. S. clinical series. J Refract Surg. 2003; 19:8–14.4. Tran DB, Sarayba MA, Bor Z, et al. Randomized prospective clinical study comparing induced aberrations with IntraLase and Hansatome flap creation in fellow eyes: potential impact on wave-front-guided laser in situ keratomileusis. J Cataract Refract Surg. 2005; 31:97–105.5. Gimbel HV, Neuhann T. Development, advantages, and methods of the continuous circular capsulorhexis technique. J Cataract Refract Surg. 1990; 16:31–7.
Article6. Gimbel HV, Neuhann T. Continuous curvilinear capsulorhexis. J Cataract Refract Surg. 1991; 17:110–1.
Article7. Subramaniam S, Tuft SJ. Early decentration of plate-haptic silicone intraocular lenses. J Cataract Refract Surg. 2001; 27:330–2.
Article8. Taketani F, Matuura T, Yukawa E, Hara Y. Influence of intraocular lens tilt and decentration on wavefront aberrations. J Cataract Refract Surg. 2004; 30:2158–62.
Article9. Baumeister M, Bühren J, Kohnen T. Tilt and decentration of spherical and aspheric intraocular lenses: effect on higher-order aberrations. J Cataract Refract Surg. 2009; 35:1006–12.
Article10. Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2008; 19:13–7.
Article11. Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. Formula choice: Hoffer Q, Holladay 1, or SRK/T and refractive outcomes in 8108 eyes after cataract surgery with biometry by partial coherence interferometry. J Cataract Refract Surg. 2011; 37:63–71.
Article12. Assia EI, Apple DJ, Tsai JC, Morgan RC. Mechanism of radial tear formation and extension after anterior capsulectomy. Ophthalmology. 1991; 98:432–7.
Article13. Hollick EJ, Spalton DJ, Meacock WR. The effect of capsulorhexis size on posterior capsular opacification: one-year results of a randomized prospective trial. Am J Ophthalmol. 1999; 128:271–9.
Article14. Peng Q, Apple DJ, Visessook N, et al. Surgical prevention of posterior capsule opacification. Part 2: Enhancement of cortical cleanup by focusing on hydrodissection. J Cataract Refract Surg. 2000; 26:188–97.15. Aasuri MK, Kompella VB, Majji AB. Risk factors for and management of dropped nucleus during phacoemulsification. J Cataract Refract Surg. 2001; 27:1428–32.
Article16. Kránitz K, Takacs A, Miháltz K, et al. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorrhexis parameters and their effects on intraocular lens centration. J Refract Surg. 2011; 27:558–63.
Article17. Nagy ZZ, Kránitz K, Takacs AI, et al. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg. 2011; 27:564–9.
Article18. Eppig T, Scholz K, Löffler A, et al. Effect of decentration and tilt on the image quality of aspheric intraocular lens designs in a model eye. J Cataract Refract Surg. 2009; 35:1091–100.
Article19. Ravalico G, Tognetto D, Palomba M, et al. Capsulorhexis size and posterior capsule opacification. J Cataract Refract Surg. 1996; 22:98–103.
Article20. Aykan U, Bilge AH, Karadayi K, Akin T. The effect of capsulorhexis size on development of posterior capsule opacification: small (4.5 to 5.0 mm) versus large (6.0 to 7.0 mm). Eur J Ophthalmol. 2003; 13:541–5.
Article21. Hollick EJ, Spalton DJ, Meacock WR. The effect of capsulorhexis size on posterior capsular opacification: one-year results of a randomized prospective trial. Am J Ophthalmol. 1999; 128:271–9.
Article22. Ram J, Pand, ey SK, Apple DJ, et al. Effect of in-the-bag intraocular lens fixation on the prevention of posterior capsule opacification. J Cataract Refract Surg. 2001; 27:1039–46.23. Hayashi K, Hayashi H, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens decentration and tilt after hydrogel lens implantation. Br J Ophthalmol. 2001; 85:1294–7.
Article24. Hayashi H, Hayashi K, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Br J Ophthalmol. 1998; 82:1429–32.
Article25. Baumeister M, Bühren J, Kohnen T. Tilt and decentration of spherical and aspheric intraocular lenses: effect on higher-order aberrations. J Cataract Refract Surg. 2009; 35:1006–12.
Article26. Miháltz K, Knorz MC, Alió JL, et al. Internal aberrations and optical quality after femtosecond laser anterior capsulotomy in cataract surgery. J Refract Surg. 2011; 27:711–6.
Article27. Filkorn T, Kovács I, Takács A, et al. Comparison of IOL power calculation and refractive outcome after laser refractive cataract surgery with a femtosecond laser versus conventional phacoemulsification. J Refract Surg. 2012; 28:540–4.
Article28. Kim SA, Lee YE, Hwang KY, Joo CK. Usefulness of open ring guider for continuous curvilinear capsulorrhexis. J Korean Ophthalmol Soc. 2013; 54:1494–500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Laser Refractive Cataract Surgery with a Femtosecond Laser Versus Conventional Phacoemulsification
- A Case of Capsule Contraction Syndrome following Continuous Curvilinear Capsulorhexis
- Comparison of Effective Phacoemulsification Time between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract Surgery
- Short-term Clinical Outcomes of Femtosecond Laser-assisted Cataract Surgery: Comparison with Conventional Phacoemulsification
- The Clinical Outcomes of Manual Continuous Curvilinear Capsulorhexis and Precision Pulse Capsulotomy