J Korean Ophthalmol Soc.
2014 Jun;55(6):902-907.
A Case of Chronic Osteomyelitis of the Orbit
- Affiliations
-
- 1Department of Ophthalmology, Chonnam National University Medical School, Gwangju, Korea. kcyoon@jnu.ac.kr
Abstract
- PURPOSE
To report a case of chronic osteomyelitis of the orbit.
CASE SUMMARY
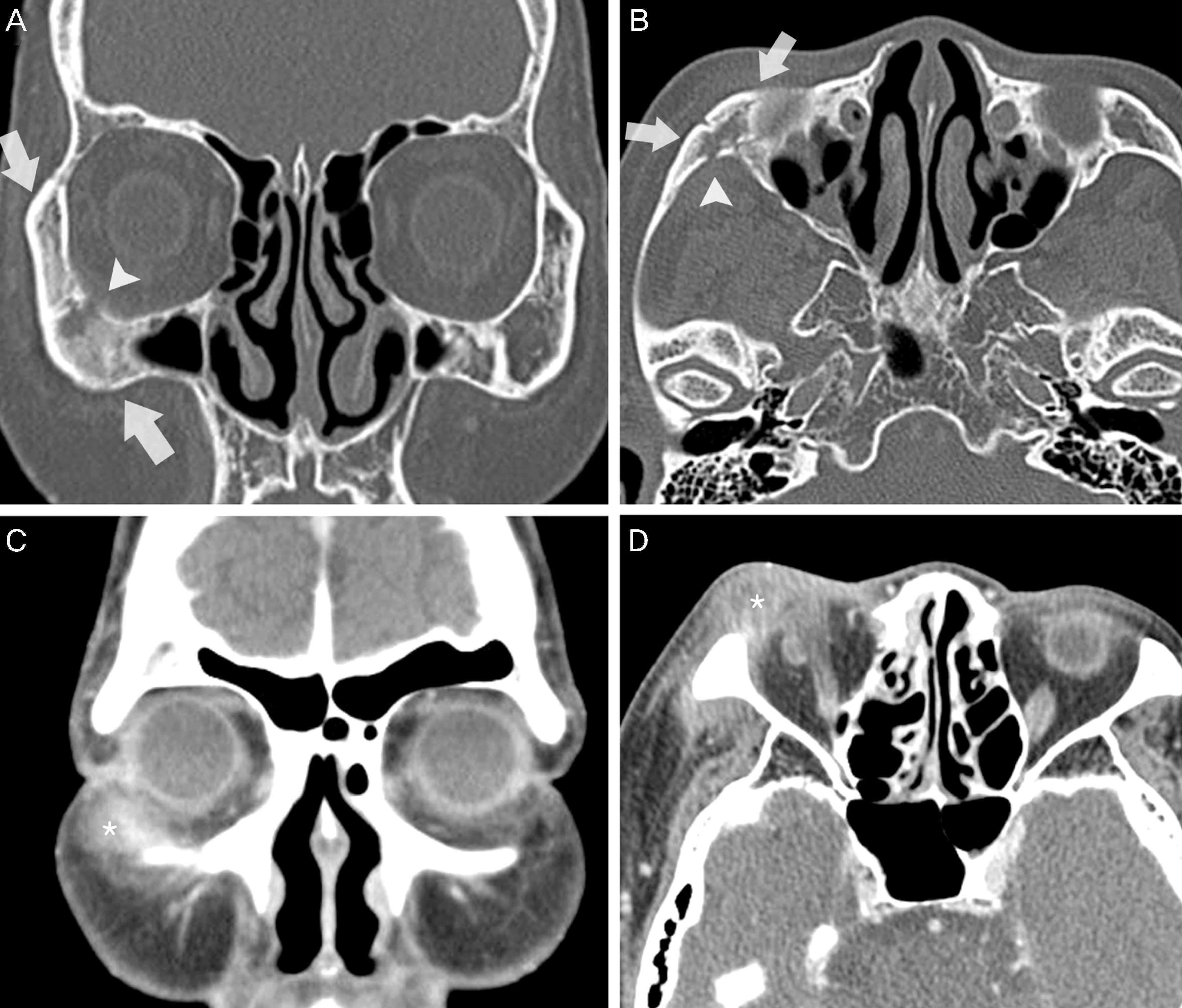
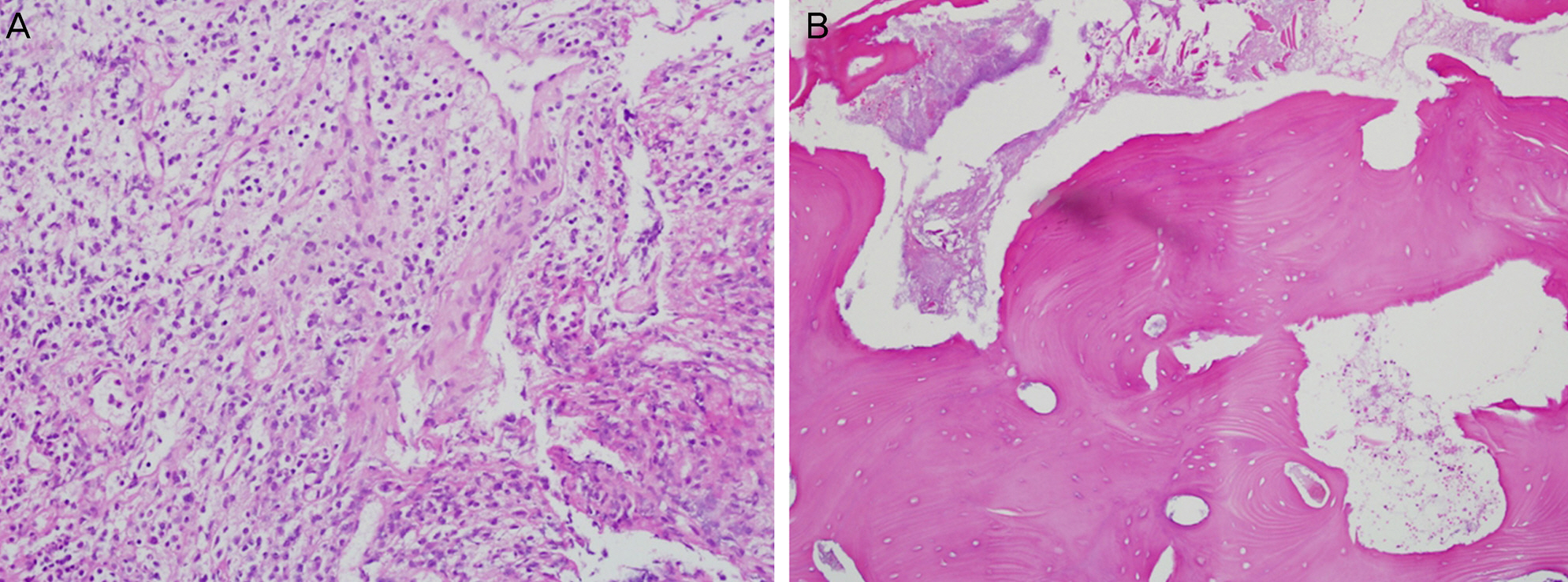
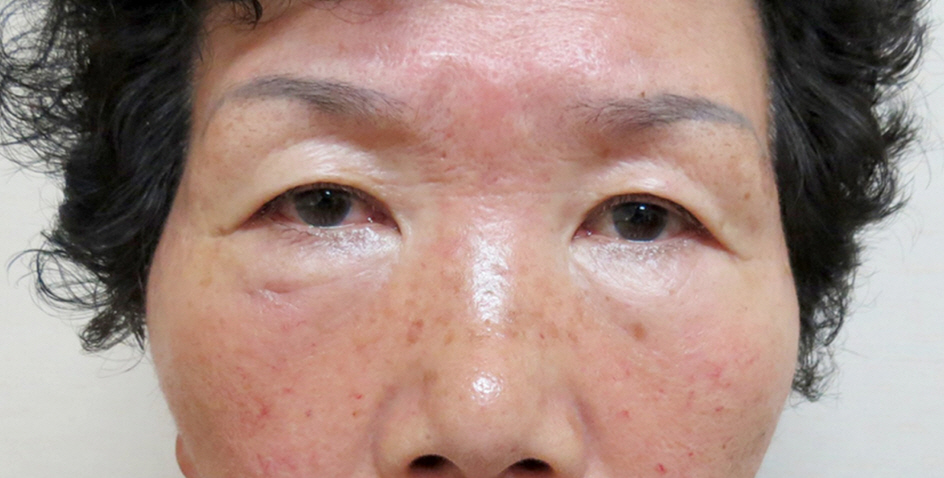
A 61-year-old woman visited the ophthalmology clinic with a 3-month history of right periorbital swelling and pain. She had a history of ondontitis treated with oral antibiotics three months previously. A hard, tender, swollen mass was palpated near the right lower eyelid extending to the floor of the right orbit. Otherwise, there were no other clinically-specific ocular signs. Orbital computed tomography and bone scan findings suggested right periorbital soft tissue inflammation with underlying osteomyelitis of maxillar and zygomatic bones involving the inferior and lateral orbital walls. The patient was admitted and treated with broad spectrum systemic antibiotics. After 7 days, periorbital soft tissue swelling and pain were improved, but the size of the hard mass was unchanged. Seven days after admission, incision and drainage of the periorbital hard mass near the lower eyelid and debridement of the necrotic and pyogenic tissue were performed. Histologic examination showed chronic granulomatous inflammation and bony necrosis of the mass. The patient was discharged after receiving systemic antibiotics for 7 more days. At the 6-month follow-up, no recurrence or abnormal findings in the right periorbital region were observed.
CONCLUSIONS
Chronic orbital osteomyelitis should be treated with combined systemic antibiotics and surgical intervention.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Koorbusch GF, Fotos P, Goll KT. Retrospective assessment of osteomyelitis. Etiology, demographics, risk factors, and manage-ment in 35 cases. Oral Surgery, Oral Medicine, Oral Pathology. 1992; 74:149–54.2. Pincus DJ, Armstrong MB, Thaller SR. Osteomyelitis of the cra-niofacial skeleton. Seminars in Plastic Surgery. 2009; 23:73–9.
Article3. Kapoor S, Kapoor MS, Sood GC. Osteomyelitis of orbital bones. J Pediatr Ophthalmol. 1977; 14:171–5.
Article4. el-Toukhy E, Szal M, Levine MR, Levine HL. Osteomyelitis of the orbit. Ophthal Plast Reconstr Surg. 1997; 13:68–71.
Article5. Sethi A, Sethi D, Agarwal AK, et al. Tubercular and chronic pyo-genic osteomyelitis of cranio-facial bones: a retrospective analysis. J Laryngol Otol. 2008; 122:799–804.
Article6. Prasad KC, Prasad SC, Mouli N, Agarwal S. Osteomyelitis in the head and neck. Acta Otolaryngol. 2007; 127:194–205.7. Chang PC, Fischbein NJ, Holliday RA. Central skull base osteo-myelitis in patients without otitis externa: imaging findings. AJNR Am J Neuroradiol. 2003; 24:1310–6.8. Kim SG, Jang HS. Treatment of chronic osteomyelitis in Korea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:394–8.
Article9. Arunkumar JS, Naik AS, Prasad KC, Santhosh SG. Role of nasal endoscopy in chronic osteomyelitis of maxilla and zygoma: a case report. Case Reports in Medicine. 2011; 2011:802964.
Article10. Kosaka Y, Yanai A, Katayama M. Idiopathic osteomyelitis of the zygoma. Plast Reconstr Surg. 1996; 97:1305–6.
Article11. Hudson JW. Osteomyelitis of the jaws: a 50-year perspective. J Oral Maxillofac Surg. 1993; 51:1294–301.
Article12. Peravali RK, Jayade B, Joshi A, et al. Osteomyelitis of maxilla in poorly controlled diabetics in a rural Indian population. J Oral Maxillofac Surg. 2012; 11:57–66.
Article13. Das JC, Singh K, Sharma P, Singla R. Tuberculous osteomyelitis and optic neuritis. Ophthalmic Surgery, Lasers and Imaging. 2003; 34:409–12.
Article14. O'Doherty M, Hannan M, Fulcher T. Voriconazole in the treatment of fungal osteomyelitis of the orbit in the immunocompromised host. Orbit. 2005; 24:285–9.15. Spoor TC, Harding SA. Orbital tuberculosis. Am J Ophthalmol. 1981; 91:644–7.
Article16. Baker AS. Role of anaerobic bacteria in sinusitis and its complications. Ann Otol Rhinol Laryngol Suppl. 1991; 154:17–22.
Article17. Bamberger DM. Osteomyelitis. A commonsense approach to anti-biotic and surgical treatment. Postgrad Med. 1993; 94:177–82. 184.18. Mader JT, Shirtliff ME, Bergquist SC, et al. Antimicrobial treat-ment of chronic osteomyelitis. Clin Orthop. 1999; 360:47–65.
Article19. Yeoh SC, MacMahon S, Schifter M. Chronic suppurative osteo-myelitis of the mandible: case report. Australian Dental Journal. 2005; 50:200–3.
Article20. Goldberg AN, Oroszlan G, Anderson TD. Complications of frontal sinusitis and their management. Otolaryngol Clin North Am. 2001; 34:211–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Recurrent Multifocal Osteomyelitis: A Case Report
- Treatment of Chronic Osteomyelitis by Transplantation of Autogenous Omentum with Microvascular Anastomosis
- Chronic Osteomyelitis in Distraction Osteogenesis Area of Tibial Shaft: A Case Report
- Chronic Recurrent Multifocal Osteomyelitis of The Shoulder: A Case Report
- Chronic Recurrent Multifocal Osteomyelitis