J Korean Ophthalmol Soc.
2014 Jan;55(1):66-72.
Comparison of Early Clinical Result of Deep Anterior Lamellar Keratoplasty Using FSlaser Versus Manual Trephine
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea School of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
Abstract
- PURPOSE
To compare outcomes of femtosecond laser-enabled deep anterior lamellar keratoplasty (IE-DALK) versus manual trephine using deep anterior lamellar keratoplasty (Manual DALK, M-DALK).
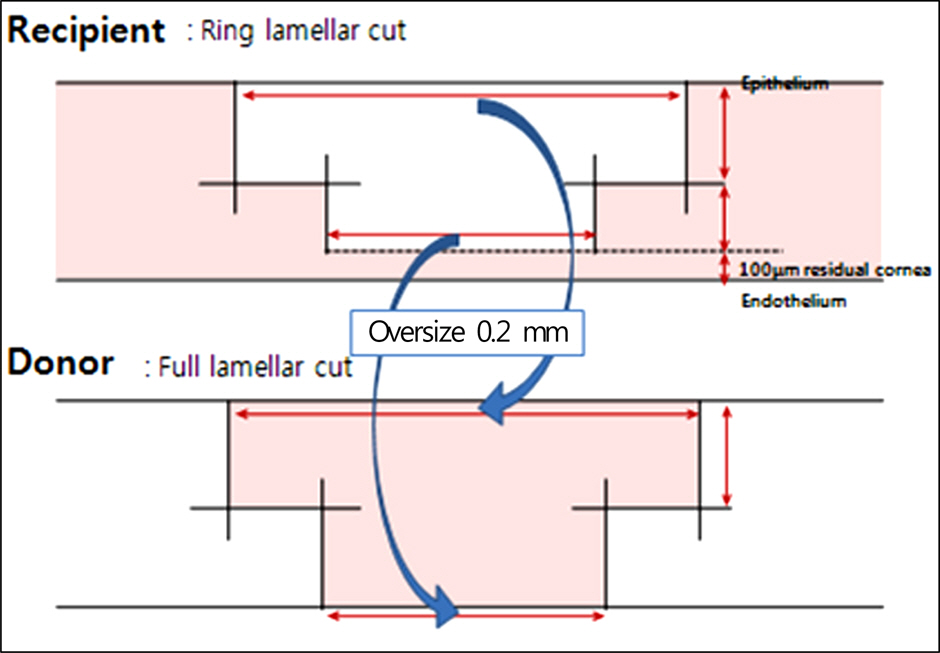
METHODS
Seventeen eyes from 17 patients underwent manual deep anterior lamellar keratoplasty, and femtosecond laser-enabled deep anterior lamellar keratoplasty was performed in 13 eyes of 13 patients. Postoperative clinical outcomes such as best corrected visual acuity, refractive astigmatism, keratometric astigmatism, endothelial cell density were compared between the two groups.
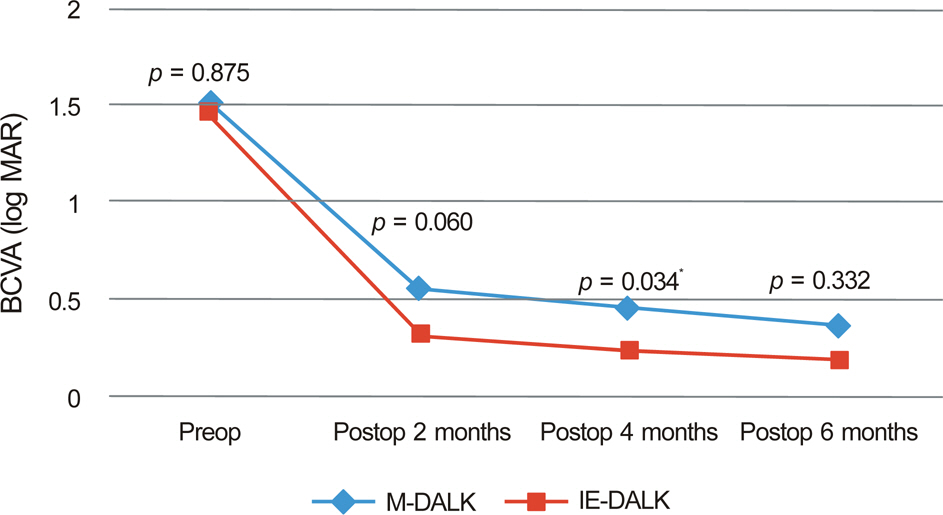
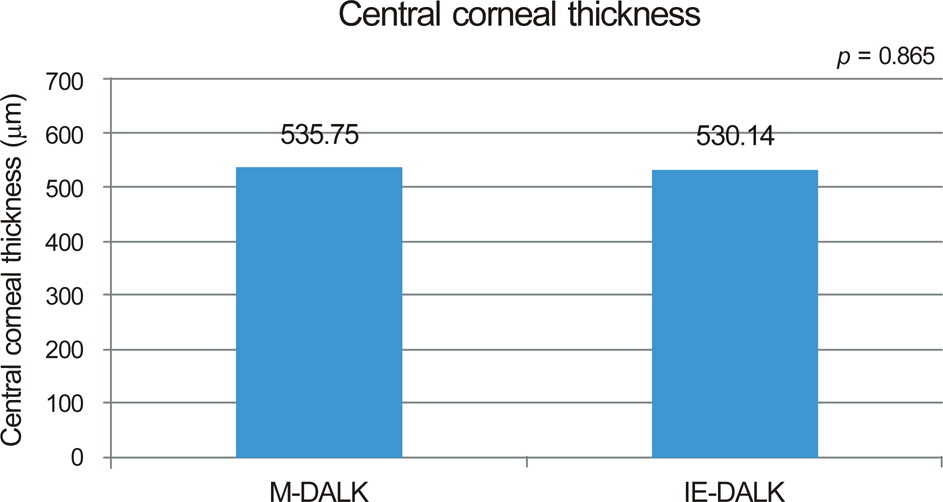
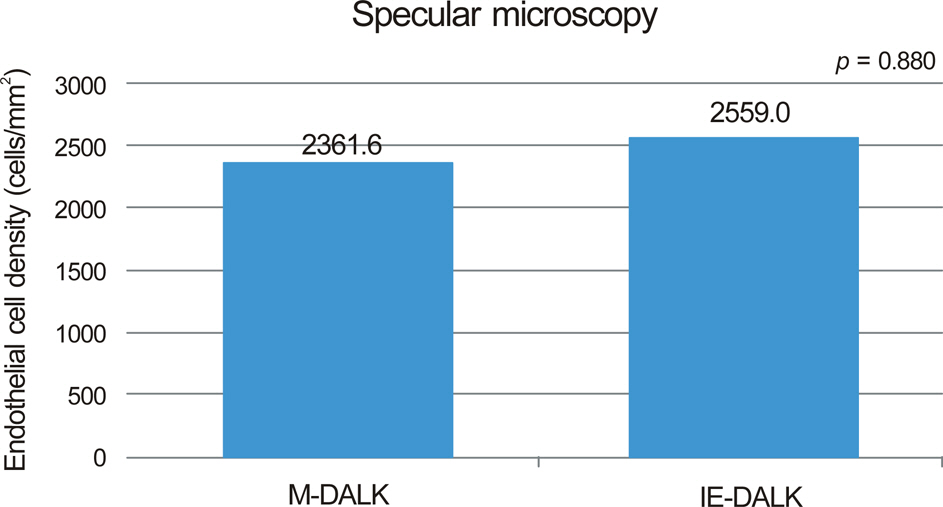
RESULTS
The mean log MAR best spectacle-corrected visual acuity (BSCVA) was 0.31 +/- 0.17, 0.23 +/- 0.15, 0.18 +/- 0.14 in the IE-DALK group, and 0.55 +/- 0.41, 0.45 +/- 0.28, 0.35 +/- 0.22 (p = 0.056, p = 0.025, p = 0.313) in the M-DALK group at postoperative 2, 4, and 6 months respectively. The mean keratometric cylinder was 5.35 +/- 1.57, 4.24 +/- 1.97, 3.65 +/- 1.31 in the IE-DALK, 8.32 +/- 2.75, 6.80 +/- 2.50, 4.54 +/- 1.25 (p = 0.031, p = 0.041, p = 0.370) in the M-DALK group at postoperative 2, 4, and 6 months respectively. Endothelial cell counts in the two groups did not differ significantly at postoperative 6 months.
CONCLUSIONS
The IE-DALK showed better results in BSCVA and keratometric astigmatism in the early postoperative period, in comparison with the M-DALK, and can be considered as a valuable method in deep anterior lamellar keratoplasty.
MeSH Terms
Figure
Reference
-
References
1. Tsubota K, Kaido M, Monden Y. . A new surgical technique for deep lamellar keratoplasty with single running suture adjustment. Am J Ophthalmol. 1998; 126:1–8.
Article2. Stern D, Schoenlein RW, Puliafito CA. . Corneal ablation by nanosecond, picosecond, and femtosecond lasers at 532 and 625 nm. Arch Ophthalmol. 1989; 107:587–92.
Article3. Farid M, Kim M, Steinert RF.Results of penetrating keratoplasty performed with a femtosecond laser zigzag incision initial report. Ophthalmology. 2007; 114:2208–12.
Article4. Ignacio TS, Nguyen TB, Chuck RS. . Top hat wound config-uration for penetrating keratoplasty using the femtosecond laser: a laboratory model. Cornea. 2006; 25:336–40.5. Malta JB, Soong HK, Shtein R. . Femtosecond laser-assisted keratoplasty: laboratory studies in eye bank eyes. Curr Eye Res. 2009; 34:18–25.
Article6. Anwar M, Teichmann KD.Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002; 21:374–83.7. Archila EA.Deep lamellar keratoplasty dissection of host tissue with intrastromal air injection. Cornea. 1984-1985; 3:217–8.
Article8. Benson WH, Goosey CB, Prager TC, Goosey JD.Visual improve-ment as a function of time after lamellar keratoplasty for keratoconus. Am J Ophthalmol. 1993; 116:207–11.
Article9. Panda A, Bageshwar LM, Ray M. . Deep lamellar keratoplasty versus penetrating keratoplasty for corneal lesions. Cornea. 1999; 18:172–5.
Article10. Tan DT, Mehta JS.Future directions in lamellar corneal transplantation. Cornea. 2007; 26(9 Suppl 1):S21–8.
Article11. Watson SL, Ramsay A, Dart JKG. . Comparison of deep la-mellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004; 111:1676–82.
Article12. Amayem AF, Anwar M.Fluid lamellar keratoplasty in keratoconus. Ophthalmology. 2000; 107:76–9.13. Funnell CL, Ball J, Noble BA.Comparative cohort study of the outcomes of deep lamellar keratoplasty and penetrating kerato-plasty for keratoconus. Eye (Lond). 2006; 20:527–32.
Article14. Trimarchi F, Poppi E, Klersy C, Piacentini C.Deep lamellar keratoplasty. Ophthalmologica. 2001; 215:389–93.
Article15. Yoo SH, Kymionis GD, Koreishi A. . Femtosecond laser-as-sisted sutureless anterior lamellar keratoplasty. Ophthalmology. 2008; 115:1303–7.
Article16. Mosca L, Fasciani R, Tamburelli C. . Femtosecond laser-as-sisted lamellar keratoplasty: early results. Cornea. 2008; 27:668–72.17. Noble BA, Agrawal A, Collins C. . Deep Anterior Lamellar Keratoplasty (DALK): visual outcome and complications for a het-erogeneous group of corneal pathologies. Cornea. 2007; 26:59–64.18. Sugita J, Kondo J.Deep lamellar keratoplasty with complete re-moval of pathological stroma for vision improvement. Br J Ophthalmol. 1997; 81:184–8.
Article19. Buratto L, Böhm E.The use of the femtosecond laser in penetrating keratoplasty. Am J Ophthalmol. 2007; 143:737–42.
Article20. Bahar I, Kaiserman I, McAllum P, Rootman D.Femtosecond laser-assisted penetrating keratoplasty: stability evaluation of differ-ent wound configurations. Cornea. 2008; 27:209–11.21. Sarayba MA, Ignacio TS, Tran DB, Binder PS.A 60 kHz IntraLase femtosecond laser creates a smoother LASIK stromal bed surface compared to a Zyoptix XP mechanical microkeratome in human donor eyes. J Refract Surg. 2007; 23:331–7.
Article22. Alió JL, Piñero DP.Very high-frequency digital ultrasound meas-urement of the LASIK flap thickness profile using the IntraLase femtosecond laser and M2 and Carriazo-Pendular microkeratomes. J Refract Surg. 2008; 24:12–23.
Article23. Bourne WM.Cellular changes in transplanted human corneas. Cornea. 2001; 20:560–9.
Article24. van Dooren BT, Mulder PG, Nieuwendaal CP. . Endothelial cell density after deep anterior lamellar keratoplasty (Melles tech-nique). Am J Ophthalmol. 2004; 137:397–400.
Article25. Arentsen JJ.Corneal transplant allograft reaction: possible predis-posing factors. Trans Am Ophthalmol Soc. 1983; 81:361–402.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Anterior Synechiolysis with Lamellar Corneal Dissection in Penetrating Keratoplasty
- Clinical Evaluation of Full-thickness Deep Lamellar Keratoplasty
- Three Cases of Urrets-Zavalia Syndrome Following Deep Lamellar Keratoplasty (DLKP)
- Comparison of the Long-term Clinical Outcomes of Penetrating Keratoplasty Using a Manual Trephine and Femtosecond-Laser Trephination
- Tectonic Deep Anterior Lamellar Keratoplasty in Impending Corneal Perforation Using Cryopreserved Cornea