J Korean Ophthalmol Soc.
2013 Sep;54(9):1463-1468.
Presumed Ocular Toxoplasmosis Presenting as Isolated Unilateral Papillitis
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea. amario@naver.com
Abstract
- PURPOSE
To report an atypical case of ocular toxoplasmosis presenting as isolated unilateral papillitis.
CASE SUMMARY
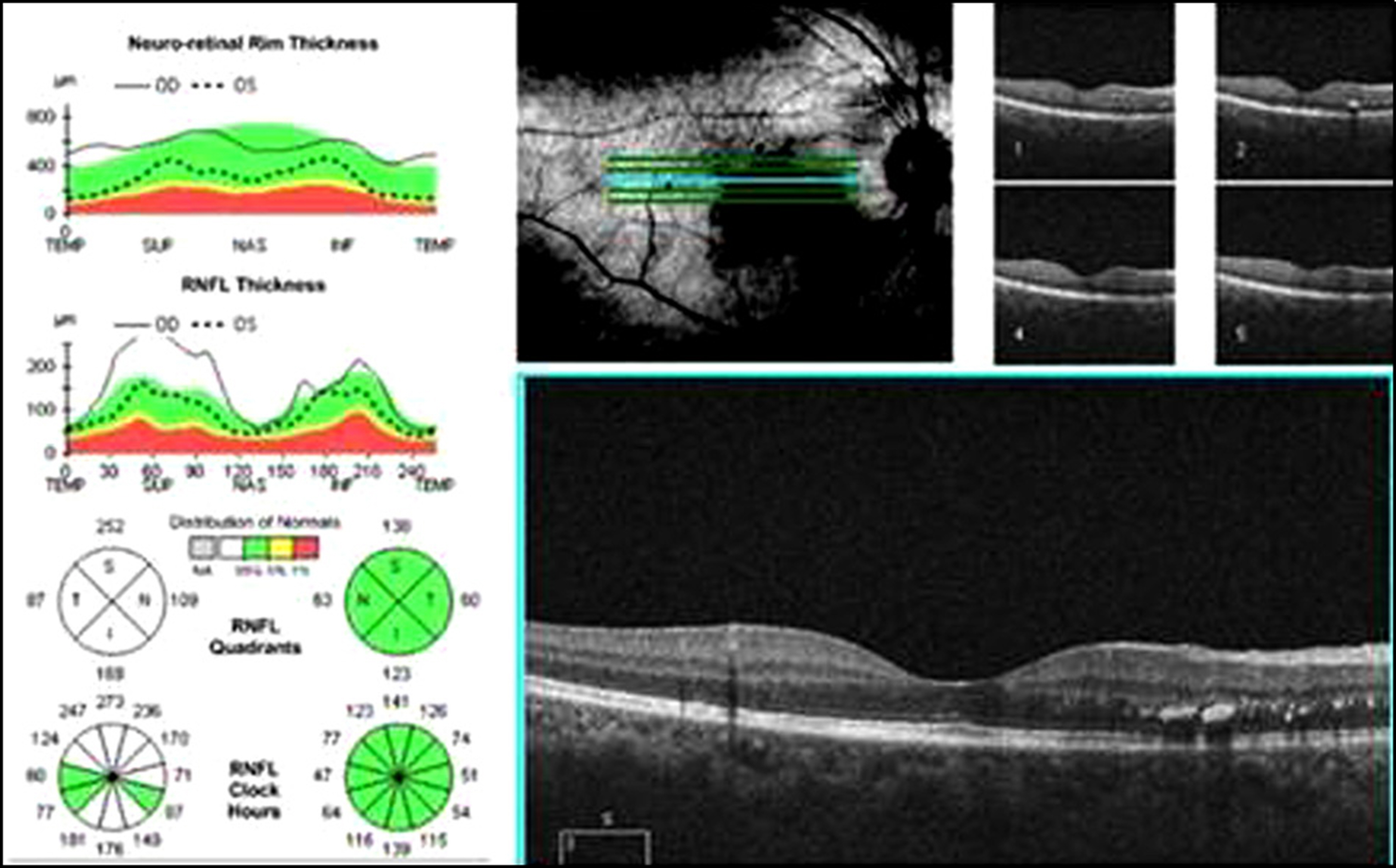
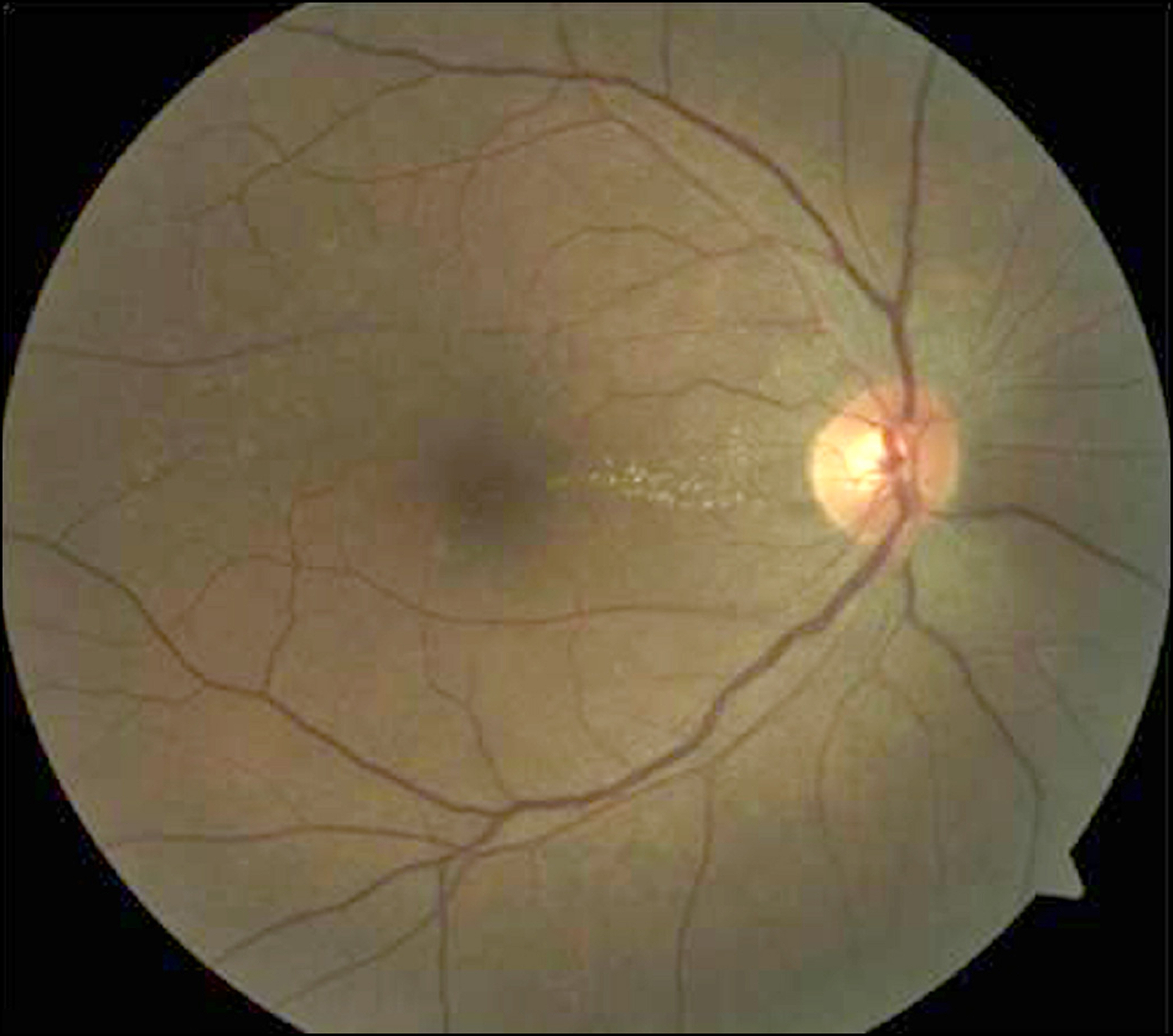
A 53-year-old female presented with visual difficulty in her right eye that had begun 1 week previously. Best corrected visual acuity was 0.8 in the right eye and 1.0 in the left eye. On fundoscopic examination, optic disc swelling and focal edema with hard exudates in the nasal parapapillary retina were found in her right eye. Fluorescein angiography revealed marked leakage of dye from the swollen optic disc. There was no evidence of vasculitis and chorioretinitis. Pupillary light reflex and color vision were normal. Visual field (VF) showed generalized reduction in the right eye, and was normal in the left eye. Optical coherence tomography (OCT) revealed right optic disc swelling. Serology was positive for toxoplasma IgM and IgG. The patient was treated with oral steroids and antitoxoplasma antibiotics. Two months later, visual acuity was 1.0 in the right eye. There was no disc swelling on fundoscopy or OCT and VF was normal.
CONCLUSIONS
Ocular toxoplasmosis can present atypically as isolated papillitis without chorioretinitis and mimic idiopathic optic neuritis. A thorough serologic examination for toxoplasmosis along with proper treatment should be performed.
MeSH Terms
-
Anti-Bacterial Agents
Chorioretinitis
Color Vision
Edema
Exudates and Transudates
Eye
Female
Fluorescein Angiography
Humans
Hydrazines
Immunoglobulin G
Immunoglobulin M
Light
Middle Aged
Optic Neuritis
Papilledema
Reflex
Retina
Retinitis
Steroids
Tomography, Optical Coherence
Toxoplasma
Toxoplasmosis
Toxoplasmosis, Ocular
Vasculitis
Visual Acuity
Visual Fields
Anti-Bacterial Agents
Hydrazines
Immunoglobulin G
Immunoglobulin M
Steroids
Figure
Reference
-
References
1. Holland GN. Ocular toxoplasmosis: a global reassessment. Part I: epidemiology and course of disease. Am J Ophthalmol. 2003; 136:973–88.2. Atmaca LS, Simsek T, Batioglu F. Clinical features and prognosis in ocular toxoplasmosis. Jpn J Ophthalmol. 2004; 48:386–91.
Article3. Biswas J, Narain S, Das D, Ganesh SK. Pattern uveitis in a referral uveitis clinic in India. Int Ophthalmol. 1996-1997; 20:223–8.
Article4. Holland GN. Ocular toxoplasmosis; a global assessment part II: disease manifestations and management. Am J Ophthalmol. 2004; 137:1–17.5. Tandon R, Menon V, Das GK, Verna L. Toxoplasmic papillitis with central retinal artery occlusion. Can J Ophthalmol. 1995; 30:374–6.6. Song A, Scott IU, Davis JL, Lam BL. Atypical anterior optic neu-ropathy caused by toxoplasmosis. Am J Ophthalmol. 2002; 133:162–4.
Article7. Wong R, dell’Omo R, Marino M. . Toxoplasma gondii: an atypical presentation of toxoplasma as optic disc swelling and hemispherical retinal vein occlusion treated with intravitreal clindamycin. Int Ophthalmol. 2009; 29:195–8.
Article8. Lee M, Fong KS, Hsu LY, Lim WK. Optic nerve toxoplasmosis and orbital inflammation as initial presentation of AIDS. Graefes Arch Clin Exp Ophthalmol. 2006; 244:1542–4.
Article9. Folk JC, Lobes LA. Presumed Toxoplasmic papillitis. Ophthalmology. 1984; 91:64–7.
Article10. Shenoy R, Al Hinai A. Presumed ocular toxoplasmosis presenting as papillitis. Indian J Ophthalmol. 2003; 51:357–9.11. Sanderfeld L, Petersen E, Sousa S. . Bilateral papillitis in ocu-lar toxoplsmosis. Eye (Lond). 2010; 24:188–9.12. Alipanahi R, Sayyahmelli S. Acute papillitis in young female with toxoplasmosis. Middle East Afr J Ophthalmol. 2011; 18:249–51.
Article13. Lee DC, Ha MS, Chang MH, Choi WS. A case of congenital tox-oplasmosis in the neonate. J Korean Ophthalmol Soc. 1999; 40:1415–20.14. Park S, Lew HM, Song JH. Intravitreal clindamycin injection for toxoplasmic retinochoroiditis. J Korean Ophthalmol Soc. 2012; 53:1046–52.
Article15. Eckert GU, Melamed J, Menegaz B. Optic nerve changes in ocular toxoplasmosis. Eye (Lond). 2007; 21:746–51.
Article16. Dubey JP, Graham DH, Blackston CR. . Biological and genetic characterisation of Toxoplasma gondii isolates from chickens from Sao Paulo, Brazil: unexpected findings. Int J Parasitol. 2002; 32:99–105.