J Korean Ophthalmol Soc.
2011 Nov;52(11):1269-1274.
The Inhibitory Effect of Myopic and Astigmatic Progression by Orthokeratology Lens
- Affiliations
-
- 1Lee and Park's Eye Clinic, Seoul, Korea. leeeye47@hanmail.net
- 2Department of Electrical Engineering, College of Engineering, Seoul National University, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University Hospital, Seoul, Korea.
- 4Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea.
Abstract
- PURPOSE
To investigate the clinical effects of orthokeratology lens wear on inhibition of the progression of Korean myopia and astigmatism.
METHODS
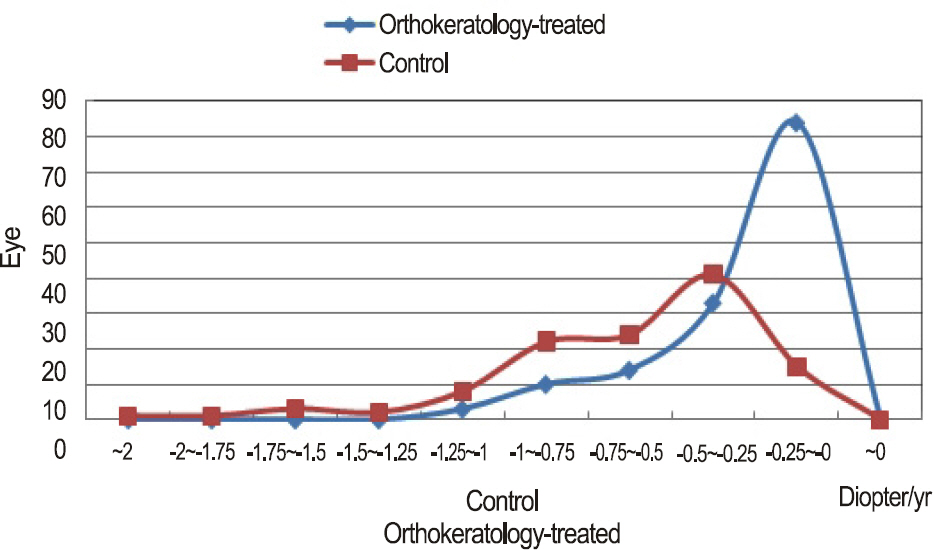
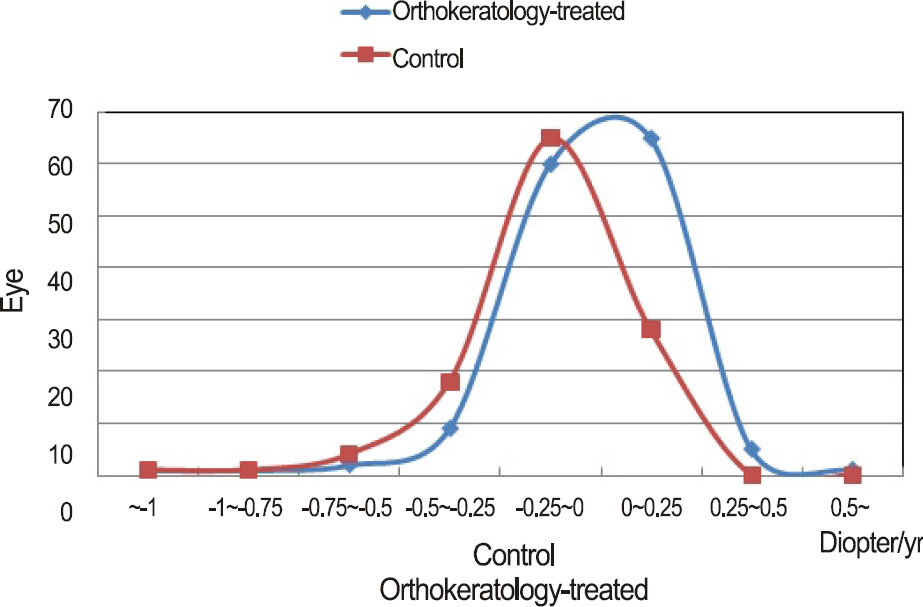
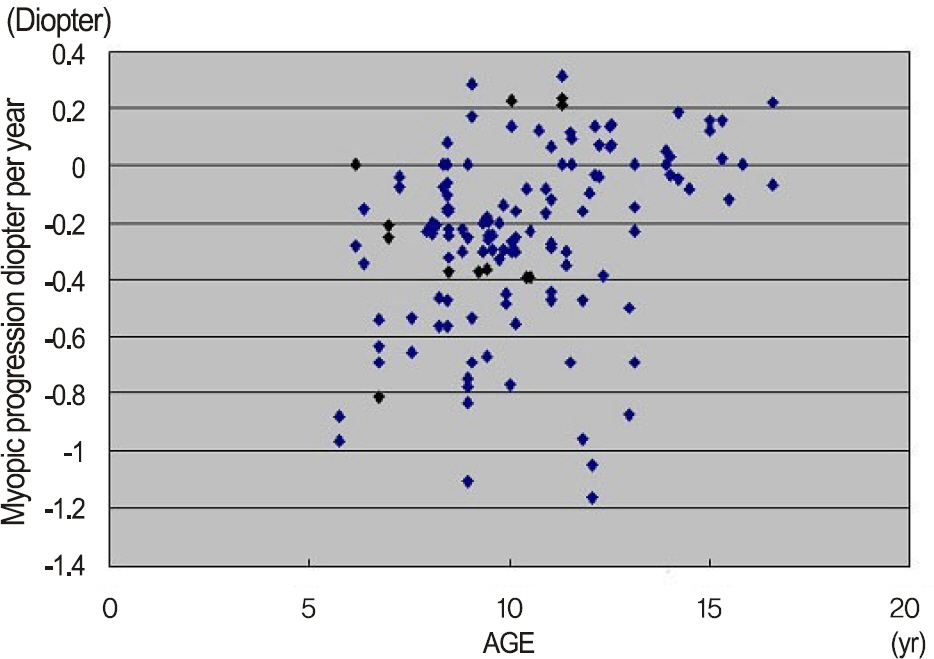
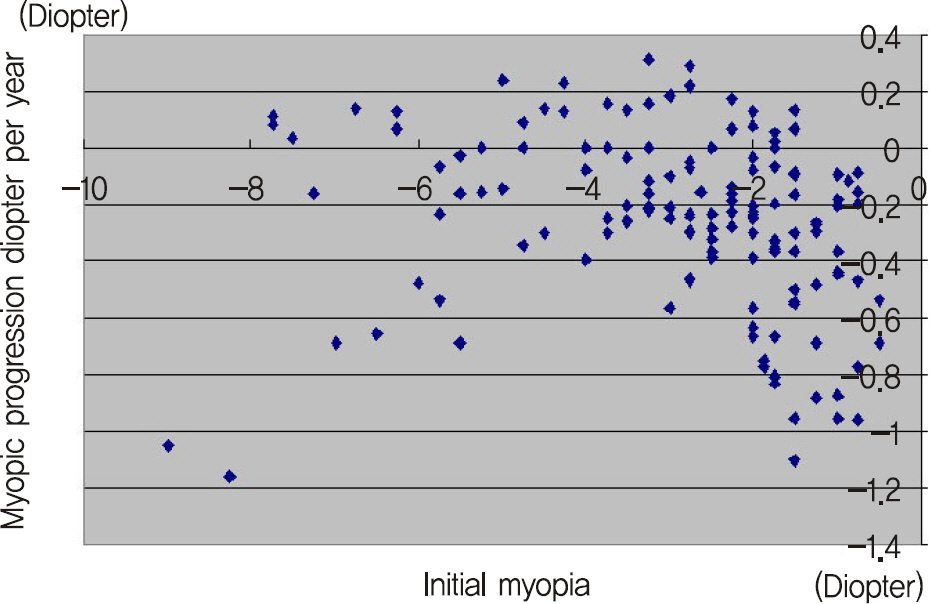
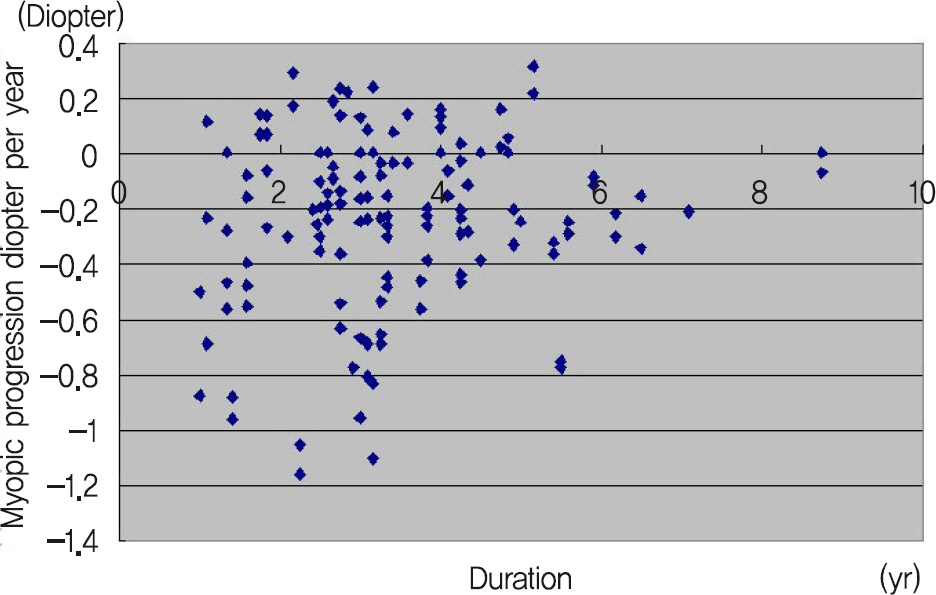
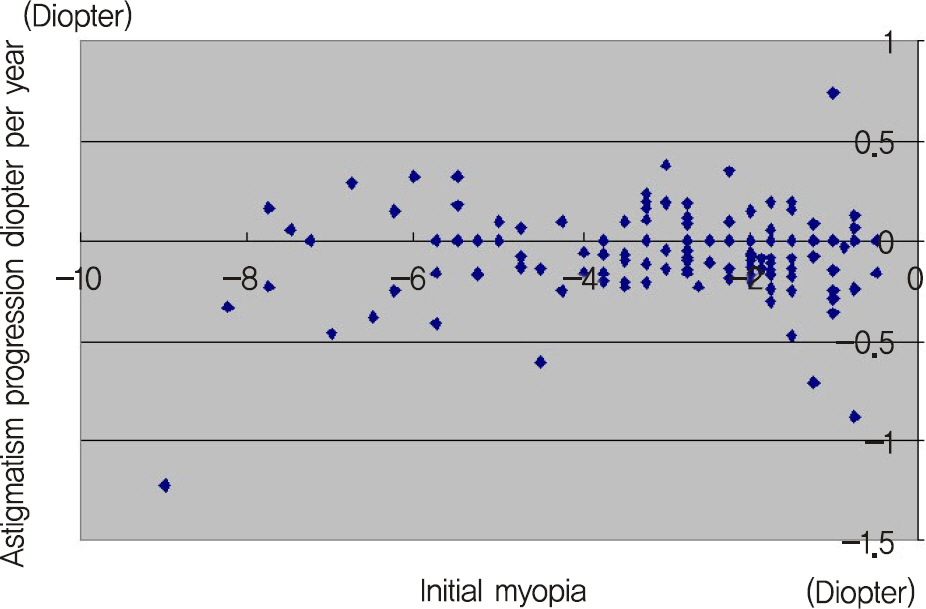
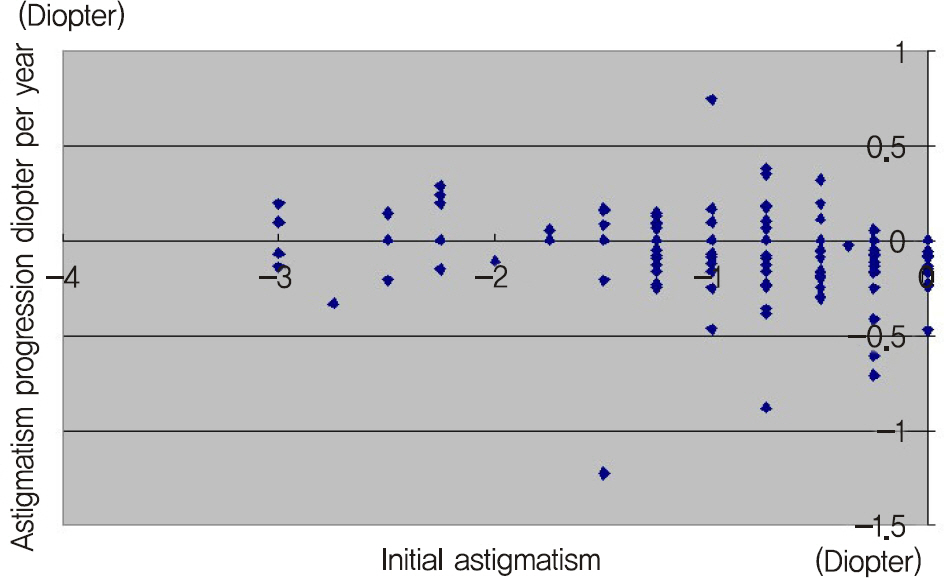
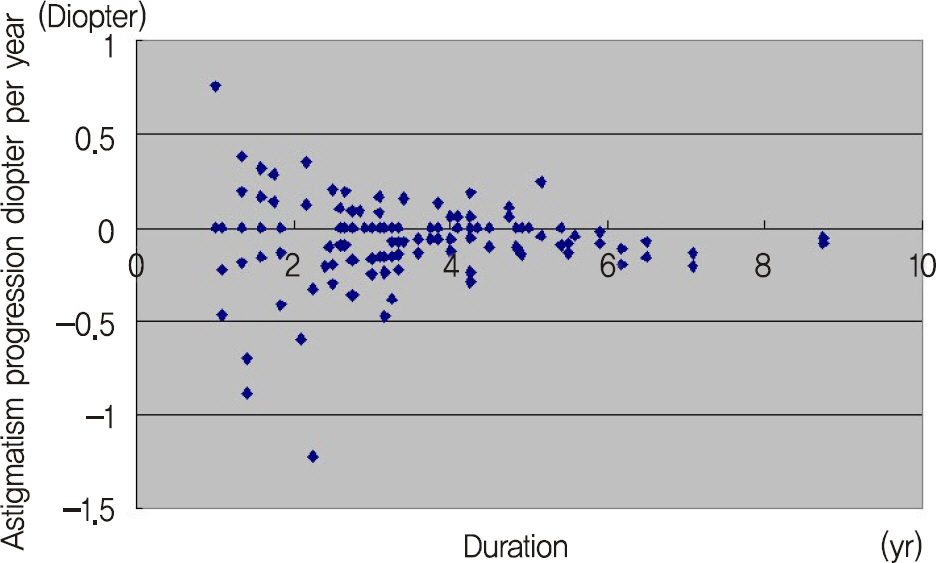
The authors reviewed out-patient records of 144 eyes of 74 patients wearing orthokeratology lenses. The cycloplegic refraction and keratometry before and after wearing the lens were compared. The 190 eyes wearing spectacles were included into the control group. We evaluated the relationship between orthokeratology lens wear and control group according to age, initial myopia, initial astigmatism, myopic progression, astigmatic progression and duration of orthokeratology lens wearing.
RESULTS
The mean cycloplegic refractive error of spherical equivalent was -3.36 +/- 1.96 diopters (D) in the patients wearing orthokeratology lenses, the mean astigmatism was -0.86 +/- 0.72 D, and the mean wearing period was 3.41 +/- 1.5 years. The mean myopic progression was 0.25 +/- 0.31 D in lens wearing, and 0.62 +/- 0.39 D in glasses wearing, respectively. There were statistically significant differences between lens and glasses wearing group (t-test, p < 0.01). The mean astigmatic progression was 0.06 +/- 0.22 D in lens wearing, and 0.15 +/- 0.21 D in glasses wearing control group respectively, and the results also show statistically significant differences (t-test, p < 0.01). There were no relationships between two groups as for age, initial myopia, initial astigmatism and duration of orthokeratology lens wearing (t-test, p > 0.01).
CONCLUSIONS
The orthokeratology lens was found to be effective in suppression of the progression of Korean myopia and astigmatism, compared with the glasses.
Keyword
Figure
Reference
-
References
1. Kim JC, Koo BS. A study of prevailing features and causes of myopia and visual impairment in urban school children. J Korean Ophthalmol Soc. 1988; 29:165–81.2. Han ER, Kang JE, Jun RM, Choi KR. Changes of refractive errors and optometric values in fourth graders at an urban elementary school in Korea. J Korean Ophthalmol Soc. 2007; 48:1119–25.
Article3. Quek TP, Chua CG, Chong CS, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. 2004; 24:47–55.
Article4. Lee MJ, Lee YH, Shyn KH. The progression of myopia with age. J Korean Ophthalmol Soc. 1987; 28:151–5.5. Kim SY, Min BM. Myopic progression according to the age of onset in childhoods. J Korean Ophthalmol Soc. 1998; 39:721–7.6. Edwards MH, Li RW, Lam CS, et al. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci. 2002; 43:2852–8.7. Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003; 44:1492–500.
Article8. Gwiazda JE, Hyman L, Norton TT, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004; 45:2143–51.
Article9. Siatkowski RM, Cotter S, Miller JM, et al. Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: a 1-year, multicenter, double-masked, placebo-controlled parallel study. Arch Ophthalmol. 2004; 122:1667–74.10. Siatkowski RM, Cotter SA, Crockett RS, et al. Two-year multicenter, randomized, double-masked, placebo-controlled parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. J AAPOS. 2008; 12:332–9.11. Adler D, Millodot M. The possible effect of under correction on myoic progression in children. Clin Exp Optom. 2006; 89:315–21.12. Katz J, Schein OD, Levy B, et al. A randomized trial of rigid gas permeable contact lenses to reduce progression of children's myopia. Am J Ophthalmol. 2003; 136:82–90.
Article13. Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomized trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004; 122:1760–9.14. Cheung SW, Cho P, Fan D. Asymmetrical increase in axial length in the two eyes of a monocular orthokeratology patient. Optom Vis Sci. 2004; 81:653–6.
Article15. Charman WN, Mountford J, Atchison DA, Markwell EL. Peripheral refraction in orthokeratology patients. Optom Vis Sci. 2006; 83:641–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Myopic Progression before and after Orthokeratology Lens Treatment
- Patient Evaluation for Orthothokeratology Lens
- Clinical Characteristics of Prescribing Orthokeratology Lenses in Adult
- Influence of Orthokeratology Lens on Axial length Elongation and Myopic Progression in Childhood Myopia
- Major Complications of Overnight Orthokeratology Lens for Myopic Correction