J Korean Ophthalmol Soc.
2010 Aug;51(8):1146-1149.
A Case of Bilateral Corneal Wound Dehiscence With Iris Prolapse After Coronary Bypass Surgery
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea School of Medicine, Suwon, Korea. donghyunjee@catholic.ac.kr
Abstract
- PURPOSE
To report a case of bilateral corneal wound dehiscence with iris prolapse after coronary artery bypass surgery.
CASE SUMMARY
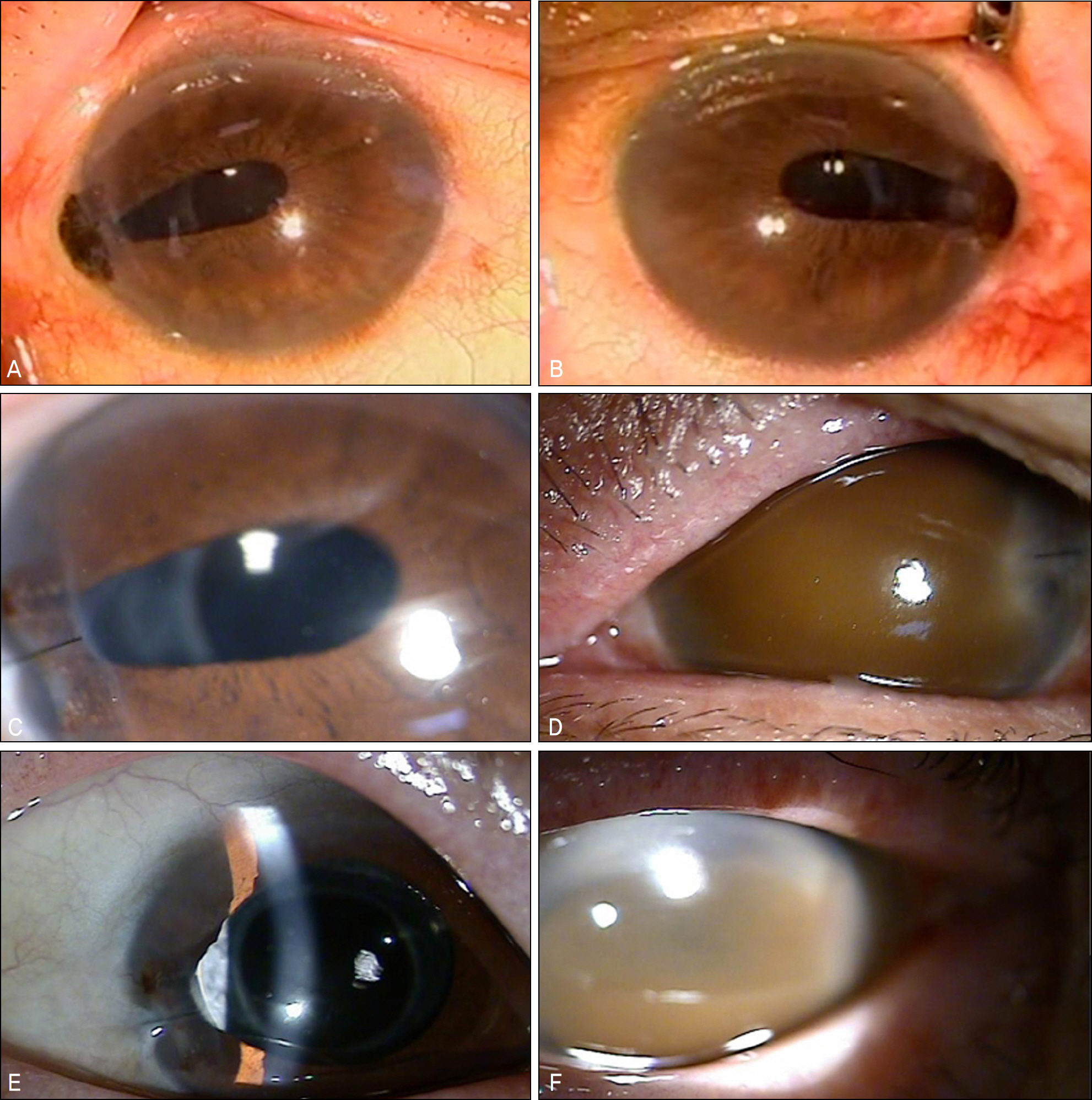
A 65-year-old woman complained of sudden bilateral vision loss. Slit lamp microscope examination showed bilateral corneal wound dehiscence, collapse of the anterior chamber and iris prolapse. The patient had a history of bilateral cataract surgery one-month earlier and a coronary artery bypass surgery one-day previously. The authors resutured the corneal wound and performed an emergency iris repositioning. Postoperative 1 day, the best corrected visual acuity (BCVA) was 0.3 in the right eye and hand motion in the left eye. Total hyphema was observed in the left eye. At postoperative 2 months, the right eye had a BCVA of 0.63 with a sutured state of the corneal wound, and the left eye had a BCVA of light perception with a clotted hemorrhage in the anterior chamber.
CONCLUSIONS
When a patient with a history of a previous sutureless cataract surgery has a coronary bypass surgery under general anesthesia, corneal wound dehiscence and iris prolapse may occur. For those patients, the authors recommend suturing the corneal wound instead of sutureless cataract surgery.
MeSH Terms
Figure
Reference
-
References
1. Taban M, Behrens A, Newcomb RL, et al. Acute endophthalmitis following cataract surgery. Arch Ophthalmol. 2005; 123:613–20.
Article2. Chee SP. Clear corneal incision leakage after phacoemulsifi- cation. Int Ophthalmol. 2005; 26:175–9.3. Lee DY, Kim JK. Changes of astigmatism after Sutureless Cataract Surgery Through 3.2 mm and 5.1 mm Incisions. J Korean Oph- thalmol Soc. 1996; 37:1263–9.4. Walker NJ, Foster A, Apel AJ. Traumatic expulsive iridodialysis after small-incision sutureless cataract surgery. J Cataract Refract Surg. 2004; 30:2223–4.
Article5. Nagdeve NG, Yaddanapudi S, Pandav SS. The effect of different doses of ketamine on intraocular pressure in anesthetized children. J Pediatr Ophthalmol Strabismus. 2006; 43:219–23.
Article6. Schutten WH, Van Horn DL. The effects of ketamine sedation and ketamine-pentobarbital anesthesia upon the intraocular pressure of the rabbit. Invest Opthalmol Vis Sci. 1977; 16:531–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Wound Dehiscence Following Cataract Surgery
- Clinical Manifestations and Prognosis of Traumatic Wound Dehiscence after Penetrating Keratoplasty
- A Case of Epithelial Downgrowth as a Complication of Penetrating Keratoplasty
- Clinical Evaluation of Traumatic Wound Dehiscence Following Cataract Surgery
- Titanium Plate Fixation for a Dehisced Sternum Following Coronary Artery Bypass Grafting: A Case Report