J Korean Ophthalmol Soc.
2010 Jan;51(1):8-13.
The Clinical Characteristics of Facial Herpes Zoster in Korean Patients
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University, College of Medicine, Cheonan, Korea. greenizy@lycos.co.kr
Abstract
- PURPOSE
To investigate the clinical characteristics of Korean patients with facial herpes zoster.
METHODS
The present study enrolled patients with facial involvement among the patients with herpes zoster. The percentage of involved branches of the trigeminal nerve, types and frequency of ocular complications, and changes in visual acuity depending on systemic treatment were analyzed.
RESULTS
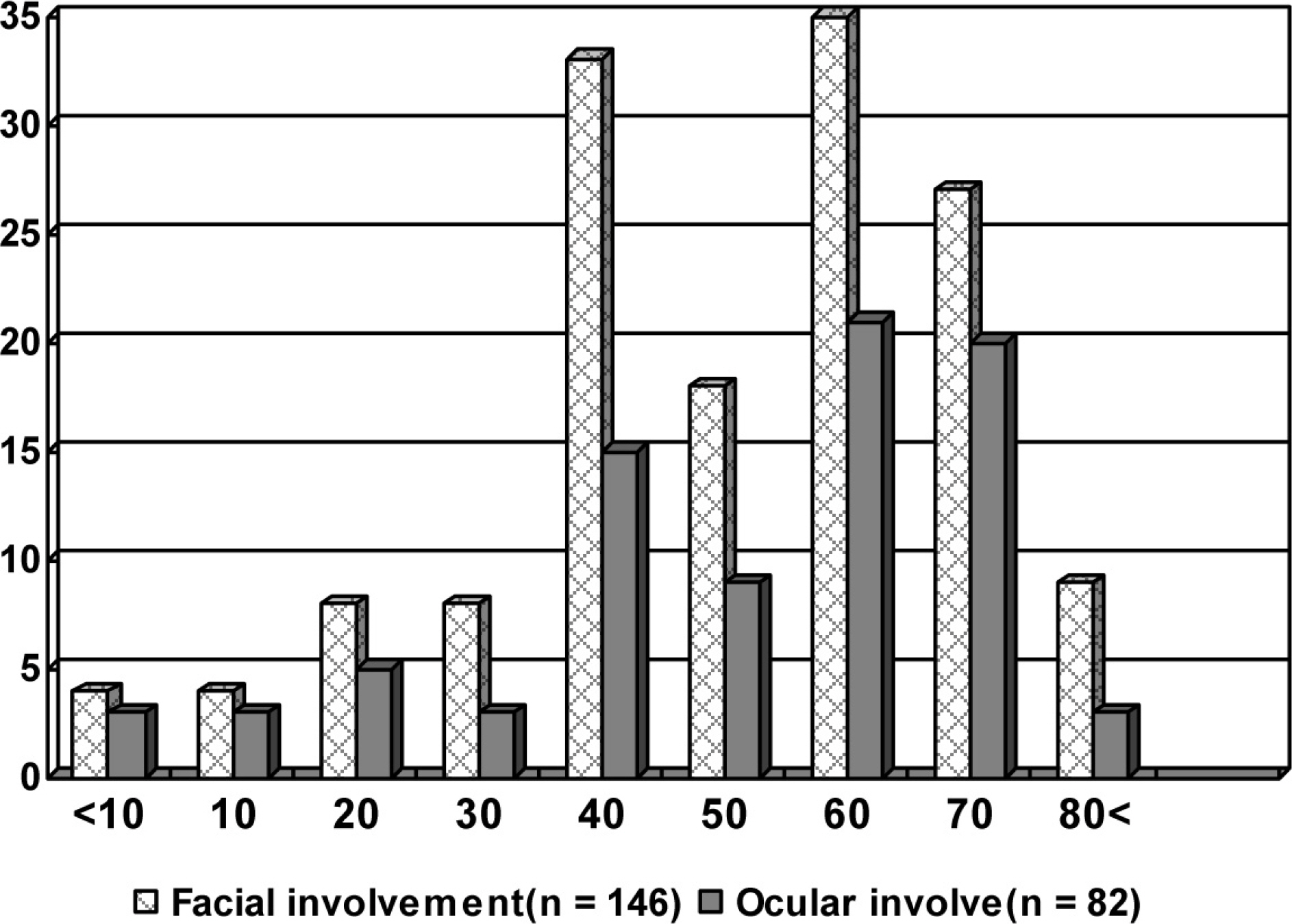
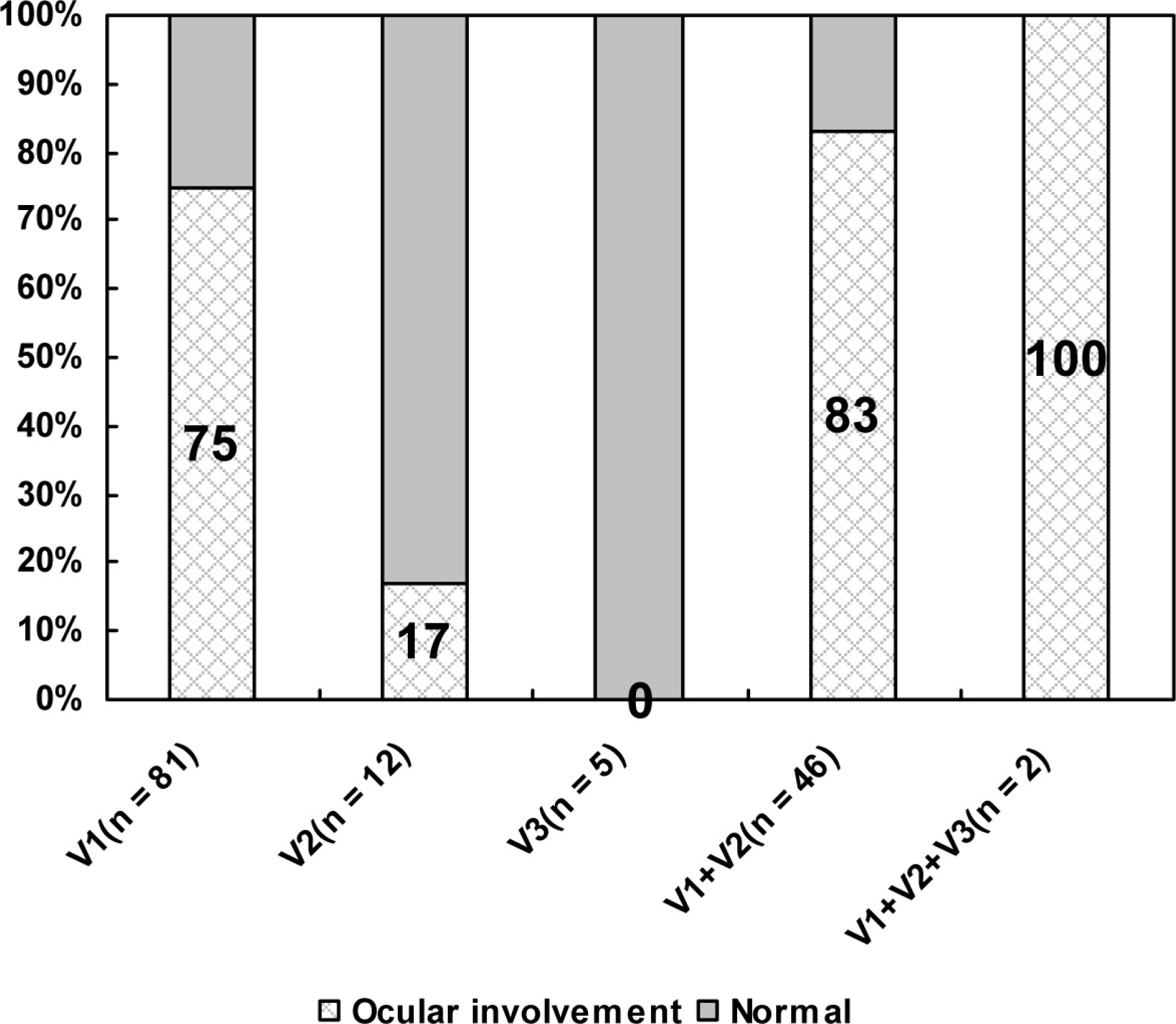
A total of 146 patients (15.9%) out of 916 patients with herpes zoster were diagnosed with facial herpes zoster. The ophthalmic branch was the most frequently involved (55.5%), and coinfection with the ophthalmic and maxillary branch was also common (31.5%). Ocular complications developed in 82 eyes (56.2%) and were most common in the group of coinfection with the ophthalmic and maxillary branch (Fisher's exact test, p=0.003). Conjunctivitis (72.0%) was the most commonly observed ocular complication, while punctate keratitis and endothelitis were also frequent. After treatment with a systemic antiviral agent, visual acuity was significantly improved (paired t test, p=0.001).
CONCLUSIONS
A higher incidence of ophthalmic complications was observed in facial herpes zoster patients with a wider area of involvement, including the ophthalmic branch. There was significant improvement of visual acuity and ocular complications after systemic treatment. Therefore, systemic antiviral treatment should be considered when a broad herpes zoster skin lesion is observed.
MeSH Terms
Figure
Reference
-
References
1. Lesegang TJ. Varicella-zoster virus eye disease. Cornea. 1999; 18:511–31.
Article2. Arvin AM. Varicella-zoster virus. Clin Microbiol Rev. 1996; 9:361–81.
Article3. Pavan-Langston D. Viral disease of the ocular anterior segment: basic science and clinical disease. Foster C, Azar D, Dolhlman C, editors. Smolin and Thoft's the Cornea: Scientific Foundations and Clinical Practice. 4th ed.Philadelphia: Lippincott Williams & Wilkins;2005. chap. 14.4. Park SH, Kim WJ, Yang SW, Kim MS. Herpes zoster aberrations complicated by hyphema, glaucoma and external aberrations. J Korean Ophthalmol Soc. 2007; 48:1573–8.5. Kim J-Y, Ahn M, Lee DW. Two cases of optic neuritis in herpes zoster ophthalmicus. J Korean Ophthalmol Soc. 2008; 49:1028–32.
Article6. Lee HR, Cho BC. A clinical study of herpes zoster ophthalmicus. J Korean Ophthalmol Soc. 1988; 29:387–91.7. McKelvie PA, Francis IC, Watson S, Nuovo G. Multifocal aberrations atrophy associated with herpes zoster ophthalmicus. Clin Experiment Ophthalmol. 2001; 29:429–32.8. de Boer JH, Luyendijk L, Rothova A. et al. Detection of aberrations antibody production to herpes viruses in acute retinal necrosis syndrome. Am J Ophthalmol. 1994; 117:201–10.9. Vazquez M, Shapiro ED. Varicella vaccine and infection with varicella-zoster virus. N Engl J Med. 2005; 352:439–40.
Article10. Hutchinson J. A clinical report on herpes zoster frontalis aberrations (shingles affecting the forehead and nose). Royal London Ophthalmol Hospital Report. 1865; 5:191.11. Womack LW, Liesegang TJ. Complication of herpes zoster ophthalmicus. Arch ophthalmol. 1983; 101:42–5.12. Yawn BP, Saddier P, Wollan PC, et al. A population based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007; 82:1341–9.13. Weksler ME. Immune senescence. Ann Neurol. 1994; 35:S35–7.
Article14. Donahue JG, Choo PW, Manson JE, Platt R. The incidence of herpes zoster. Arch Intern Med. 1995; 155:1605–9.
Article15. Liesegang TJ. Corneal complications of herpes zoster aberrations. Ophthalmology. 1985; 92:316–24.16. Lee WB, Liesegang TJ. Herpes zoster keratitis. Krachmer JH, Mannis MJ, Holland EJ, editors. Corneal. 2nd ed.Philadelphia: aberrations Mosby;2005. chap. 84.
Article17. Liesegang TJ. Herpes zoster virus infection. Curr Opin aberrations. 2004; 15:531–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Herpes Zoster Oticus Involving Glossopharyngeal Nerve without Facial Nerve Palsy
- Herpes Zoster Oticus
- The prognostic factors of the facial nerve paralysis in herpes zoster oticus
- Delayed Facial Paralysis After Middle Ear and Mastoid Surgery due to Reactivation of Herpes-Zoster Virus
- Herpes Zoster Treated with Vidarabine-5-Monophosphate