J Korean Ophthalmol Soc.
2008 Nov;49(11):1717-1722.
Clinical Usefulness of Laser Cystectomy
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. Tsoooo@hanmail.net
Abstract
- PURPOSE
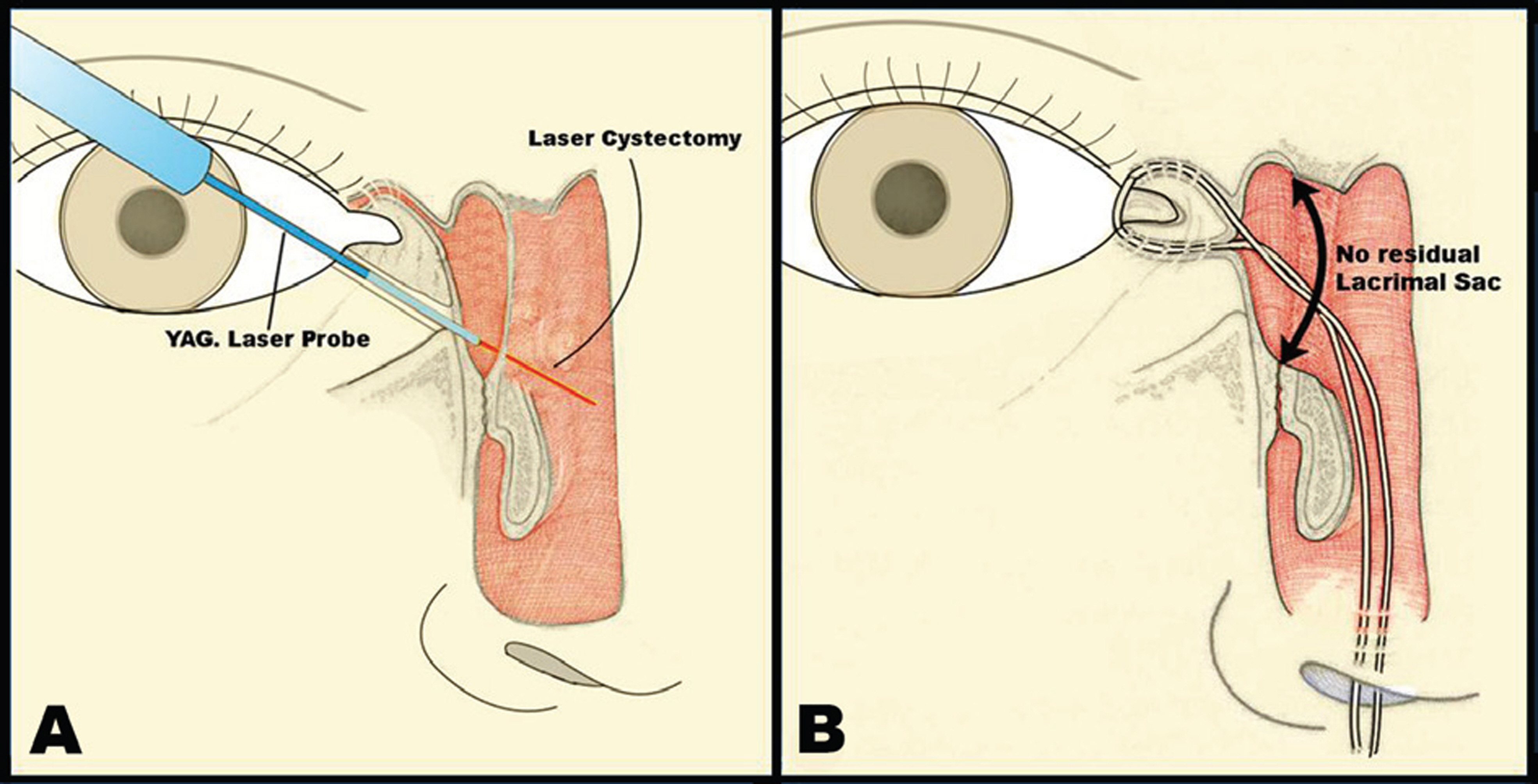
To evaluate the usefulness of laser cystectomy for the treatment of patients with dacryocystitis and sump syndrome.
METHODS
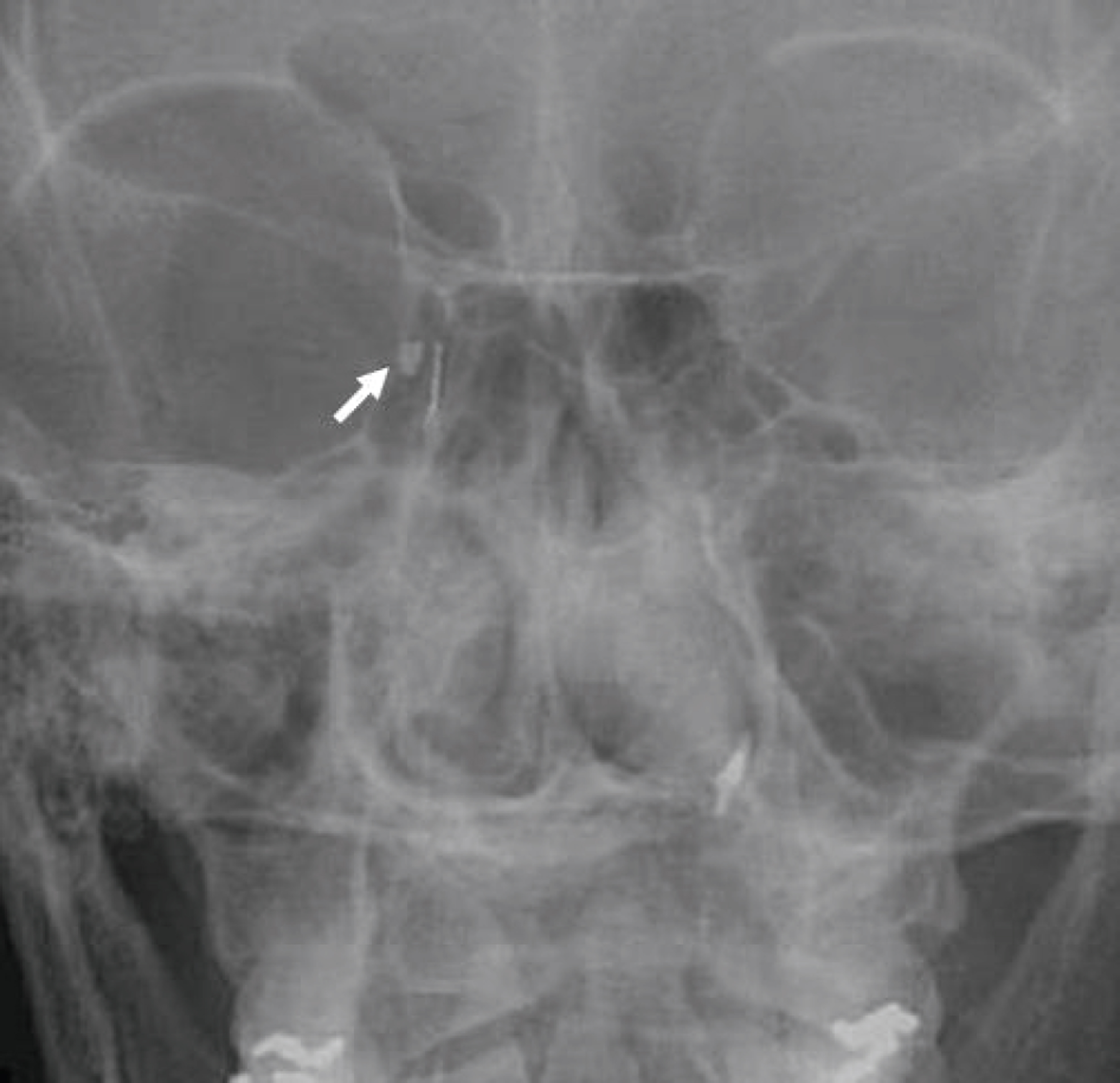
Thirteen patients (13 eyes) diagnosed with acute or chronic dacryocystitis, and nine patients (9 eyes) who developed sump syndrome after dacryocystorhinostomy from 2005 to 2006 underwent laser cystectomy and endonasal dacryocystorhinostomy.
RESULTS
Pain and swelling around the orbit improved immediately after the operation in patients with acute dacryocystitis, and all symptoms of sump syndrome disappeared by 1 month postoperatively. Epiphora reduced in all patients. During the follow-up period, functional nasolacrimal duct obstruction occurred in one eye and membranous obstruction developed in two eyes. In these two eyes with membranous obstruction, revisional surgery was performed successfully. No recurrence of dacryocystitis was noticed.
CONCLUSIONS
Laser cystectomy with endonasal dacryocystorhinostomy is a simple and effective treatment modality for patients with dacryocystitis and sump syndrome that minimizes the risk of recurrence.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Allen KM, Berlin AJ, Levine HL. Intranasal endoscopic analysis of dacryocystorhinostomy failure. Ophthalmic Plast Reconstr Surg. 1988; 4:143–5.2. Welham RA, Wulc AE. Management of unsuccessful lacrimal surgery. Br J Ophthalmol. 1987; 71:152–7.
Article3. Migliori ME. Endoscopic evaluation and management of the lacrimal sump syndrome. Ophthalmic Plast Reconstr Surg. 1997; 13:281–4.
Article4. Jordan DR, McDonald H. Failed dacryocystorhinostomy: the sump syndrome. Ophthalmic Surg. 1993; 100:692–3.
Article5. Kikkawa DO, Heinz GW, Martin RT, et al. Orbital cellulitis and abscess secondary to dacryocystitis. Arch Ophthalmol. 2002; 120:1096–9.6. Molgat YM, Hurwitz JJ. Orbital abscess due to acute dacryocystitis. Can J Ophthalmol. 1993; 28:181–3.
Article7. Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthal Plast Reconstr Surg. 1993; 9:38–41.
Article8. Massaro BM, Gonnering RS, Harris GJ. Endonasal laser dacryocystorhinostomy: a new approach to nasolacrimal duct obstruction. Arch Ophthalmol. 1990; 108:1172–6.9. Woog JJ, Metson R, Puliafito CA. Holmium:YAG endonasal laser dacryocystorhinostomy. Am J Ophthalmol. 1993; 116:1–10.10. Lee TS, Woog JJ. Endonasal dacryocystorhinostomy in the primary treatment of acute dacryocystitis with abscess formation. Ophthal Plast Reconstr Surg. 2000; 17:180–3.
Article11. Paulsen F, Thale A, Kohla G, et al. Functional anatomy of human lacrimal duct epithelium. Anat Embryol. 1998; 198:1–12.
Article12. Paulsen F. The human nasolacrimal ducts. Adv Anat Embryol Cell Biol. 2003; 170:1–106.
Article13. Paulsen FP, Corfield AP, Hinz M, et al. Characterization of mucins in human lacrimal sac and nasolacrimal duct. Invest Ophthalmol Vis Sci. 2003; 44:1807–13.
Article14. Shin HH, Lee TS, Baek SH. The comparison of surgical results of endonasal dacryocystorhinostomy in children and adults. J Korean Ophthalmol Soc. 2006; 47:877–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of CO2 laser vaporization with cystectomy for bartholin's duct cyst
- A Technique of Partial Cystectomy for Carcinoma
- Efficacy of ablation and sclerotherapy for the management of ovarian endometrioma: A narrative review
- Analysis of Postoperative Results According to the Types of Urinary Diversionafter Radical Cystectomy
- Fol1ow-up of Sexual Activity in Bladder Tumor Patients Following Total Cystectomy