J Korean Ophthalmol Soc.
2007 Dec;48(12):1623-1629.
Factors Associated with the Successful Separation of Corneal Epithelium in Epi-LASIK
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine Korea University, Seoul, Korea. hyomkim@kumc.or.kr
Abstract
-
PURPOSE: To determine the incidence and perioperative factors of flap-related complications from Epi-LASIK.
METHODS
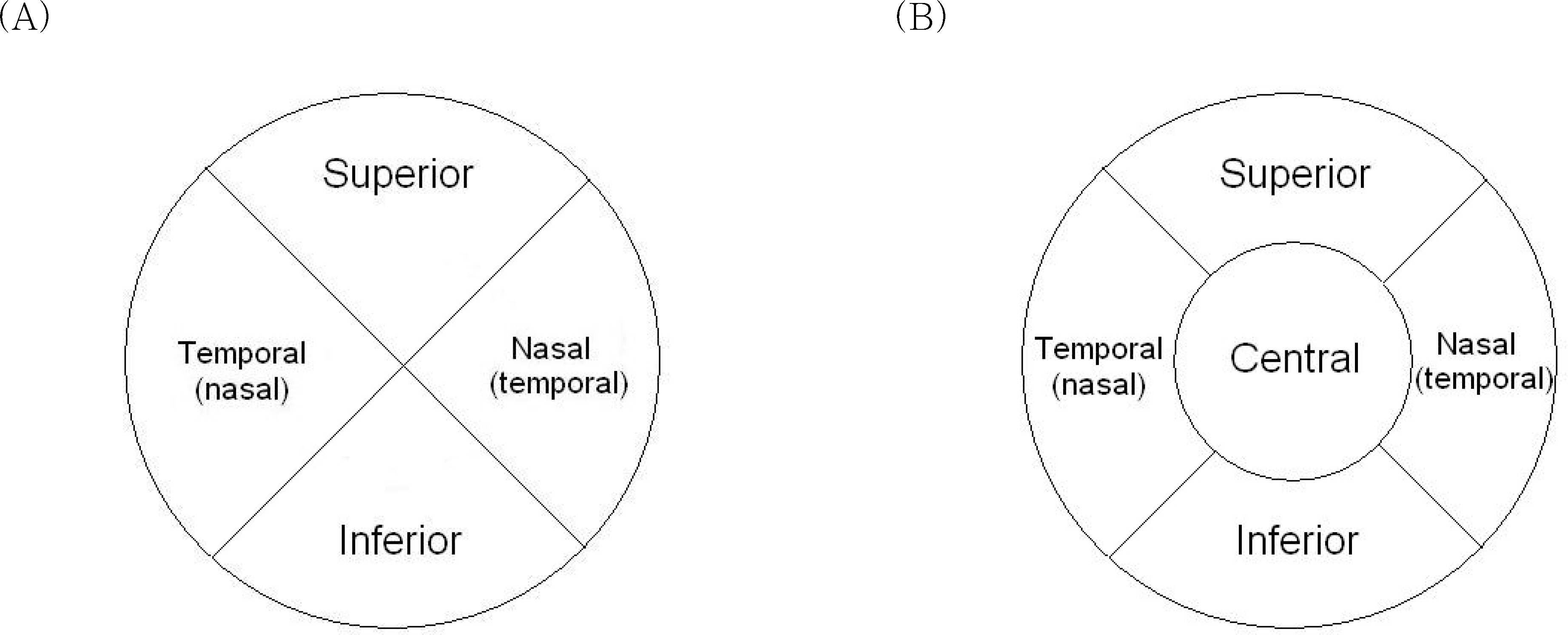
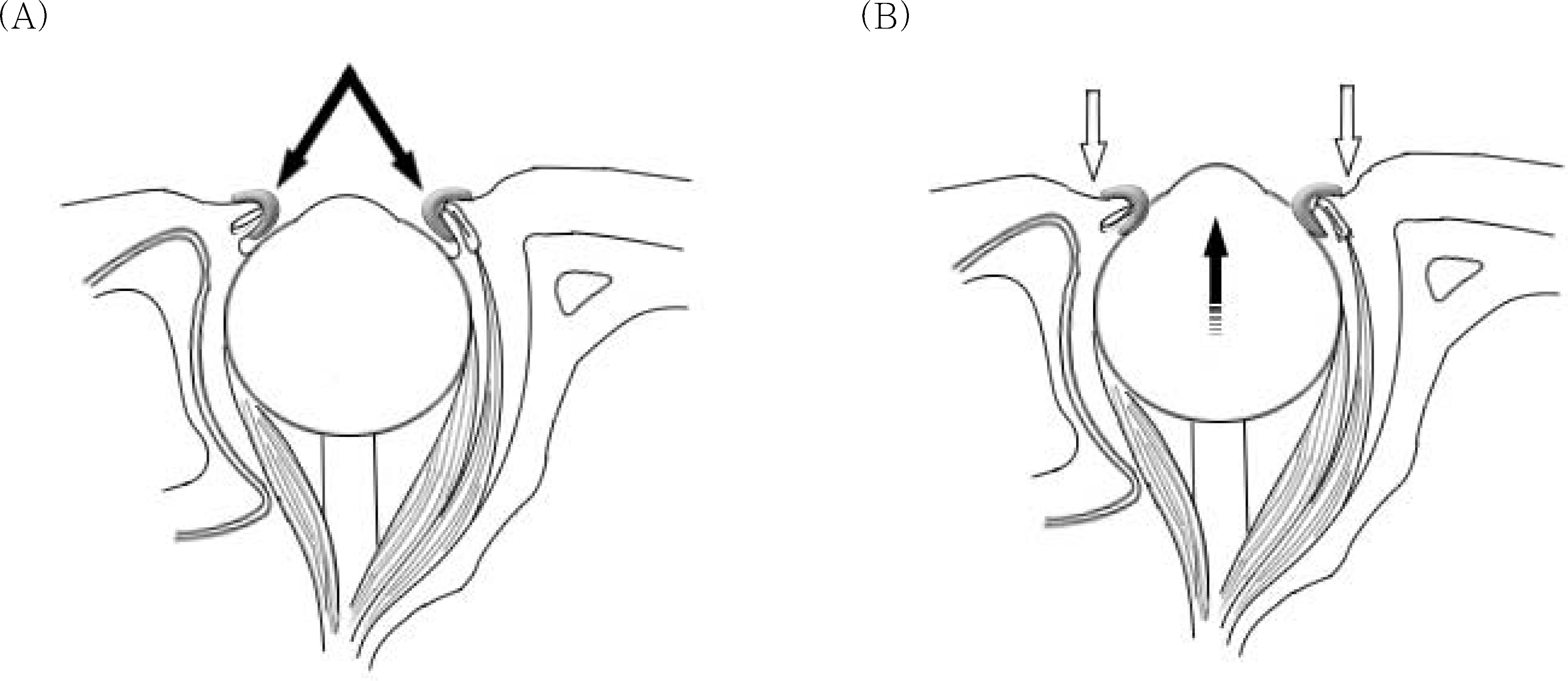
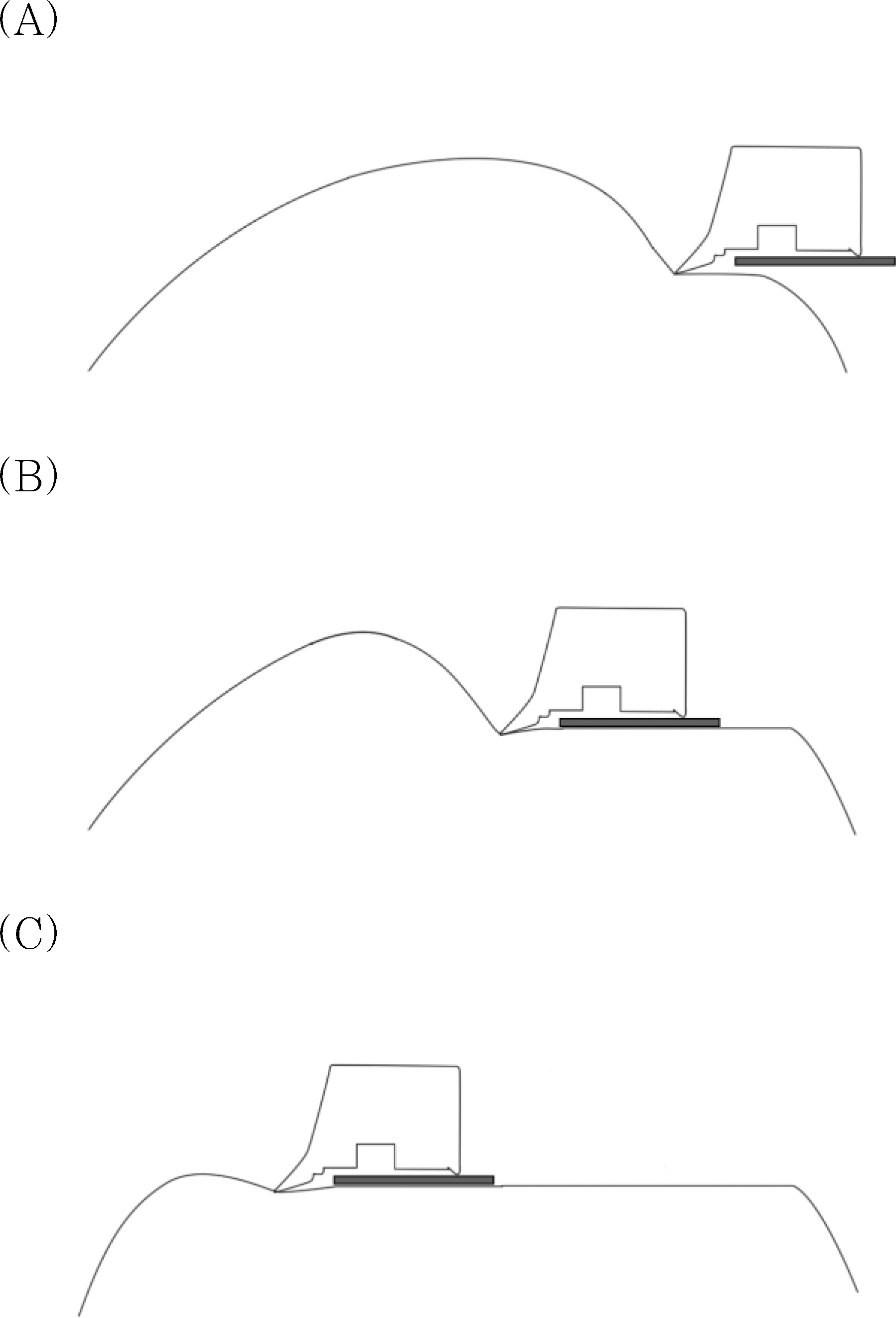
In this study, 122 eyes of 66 patients who had Epi-LASIK using Centurion SES(TM) epikeratome (Norwood Eye Care, Australia) were enrolled. Associations of pre-operative corneal curvature, white-to-white distance, central corneal thickness, refractive error, dry eye, punctate corneal erosion, pannus, and history of wearing contact lenses with flap-related complications were investigated. To decrease flap-related complications, surgeons pressed patients' eyelids with a speculum during epithelial separation, and the effect of this method was verified.
RESULTS
Complete epithelial separation was achieved in 74 eyes (60.6%), incomplete separation in 29 eyes (23.8%), and free epithelial sheet in 19 eyes (15.6%). Thin corneas (P=.041), a history of wearing contact lenses (P=.008), and the duration of contact lens use (P=.003) significantly decreased the incidence of successful epithelial separation. Pressing down the eyelids with a speculum while separating the epithelial sheet increased the incidence of complete separation from 50.6% to 83.8% (P=.003).
CONCLUSIONS
The risk of flap-related complications from Epi-LASIK may be higher in people who use contact lenses and in people who have thin corneas. The risk can be reduced by pressing the eyelids with a speculum during epithelial separation.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Duffey RJ, Leaming D. US trends in refractive surgery:2003 ISRS/AAO survey. J Refract Surg. 2005; 21:87–91.2. Lee JB, Seong GJ, Lee JH, et al. Comparison of laser epithelial keratomileusis and photorefractive keratectomy for low to moderate myopia. J Cataract Refract Surg. 2001; 27:565–70.
Article3. Chen CC, Chang JH, Lee JB, et al. Human corneal epithelial cell viability and morphology after dilute alcohol exposure. Invest Iphthalmol Vis Sci. 2002; 43:2593–602.4. Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003; 14:207–12.
Article5. Pallikaris IG, Kalyvianaki MI, Katsanevaki VJ, Ginis HS. Epi-LASIK:preliminary clinical results of an alternative surface ablation procedure. J Cataract Refract Surg. 2005; 31:879–85.6. Azar DT, Ang RT, Lee JB, et al. Laser subepithelial keratomileusis: electron microscopy and visual outcomes of flap photorefractive keratectomy. Curr Opin Ophthalmol. 2001; 12:323–8.
Article7. Nichols KK, Nichols JJ, Mitchell L. The relation between tear film tests in patients with dry eye disease. Ophthalmic Physiol Opt. 2003; 23:553–60.
Article8. Kim JH, Oh CH, Song JS, Kim HM. Inadvertent stromal dissection during mechanical separation of the corneal epithelium using an epikeratome. J Cataract Refract Surg. 2006; 32:1759–63.
Article9. Matsumoto JC, Chu YS. Epi-LASIK update:overview of techniques and patient management. Int Ophthalmol Clin. 2006; 46:105–15.10. Shah S, Sebai Sarhan AR, Doyle SJ, et al. The epithelial flap for photorefractive keratectomy. Br J Ophthalmol. 2001; 85:393–6.
Article11. Vesaluoma M, Perez-Santonja J, Petroll WM, et al. Corneal stromal changes induced by myopic LASIK. Invest Ophthalmol Vis Sci. 2000; 41:369–76.12. Holden BA, Sweeney DF, Vannas A, et al. Effects of long-term extended contact lens wear on the human cornea. Invest Ophthalmol Vis Sci. 1985; 26:1489–501.13. Vannas A, Holden BA, Makitie J. The ultrastructure of contact lens induced changes. Acta Ophthalmol. 1984; 62:320–33.
Article14. Bourne WM, Hodge DO, McLaren JW. Estimation of corneal endothelial pump function in long-term contact lens wearers. Invest Ophthalmol Vis Sci. 1999; 40:603–11.15. Bruce AS, Brennan NA. Corneal pathophysiology with contact lens wear. Surv Ophthalmol. 1990; 35:25–58.
Article16. Liesegang TJ. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002; 28:12–27.17. Liu Z, Pflugfelder SC. The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity. Ophthalmology. 2000; 107:105–11.18. Braun DA, Anderson Penno EE. Effect of contact lens wear on central corneal thickness measurements. J Cataract Refract Surg. 2003; 29:1319–22.
Article19. Madigan MC, Holden BA. Reduced epithelial adhesion after extended contact lens wear correlates with reduced hemidesmosome density in cat cornea. Invest Ophthalmol Vis Sci. 1992; 33:314–23.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corneal Epithelial Separation and Corneal Wound Healing Effect between Alcohol and Mechanical Device for Epithelial Flap
- Short Term Clinical Results of Laser Epithelial Keratomileusis and Epi-Laser in Situ Keratomileusis for Moderate and High Myopia
- Early Postoperative Pain and Visual Outcomes Following Epipolis-Laser In Situ Keratomileusis and Photorefractive Keratectomy
- Comparison of Laser Epithelial Keratomileusis Versus Epipolis-Laser in Situ Keratomileusis for Moderate to High Myopia
- Comparison of Short Term Clinical Results Between Epi-LASIK and Femtosecond LASIK