J Korean Ophthalmol Soc.
2007 Nov;48(11):1583-1587.
A Case of Intravitreal Voriconazole for the Treatment of Drug-resistant Penicillium Endophthalmitis
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Chungnam National University, Korea. kimjy@cnu.ac.kr
- 2Cancer Research Institute, Chungnam National University Hospital, Korea.
- 3Research Institute for Medical Science, Chungnam National University, Daejeon, Korea.
Abstract
-
PURPOSE: To report a case of a drug-resistant Penicillium endophthalmitis that was treated with intravitreal voriconazole injection.
CASE SUMMARY
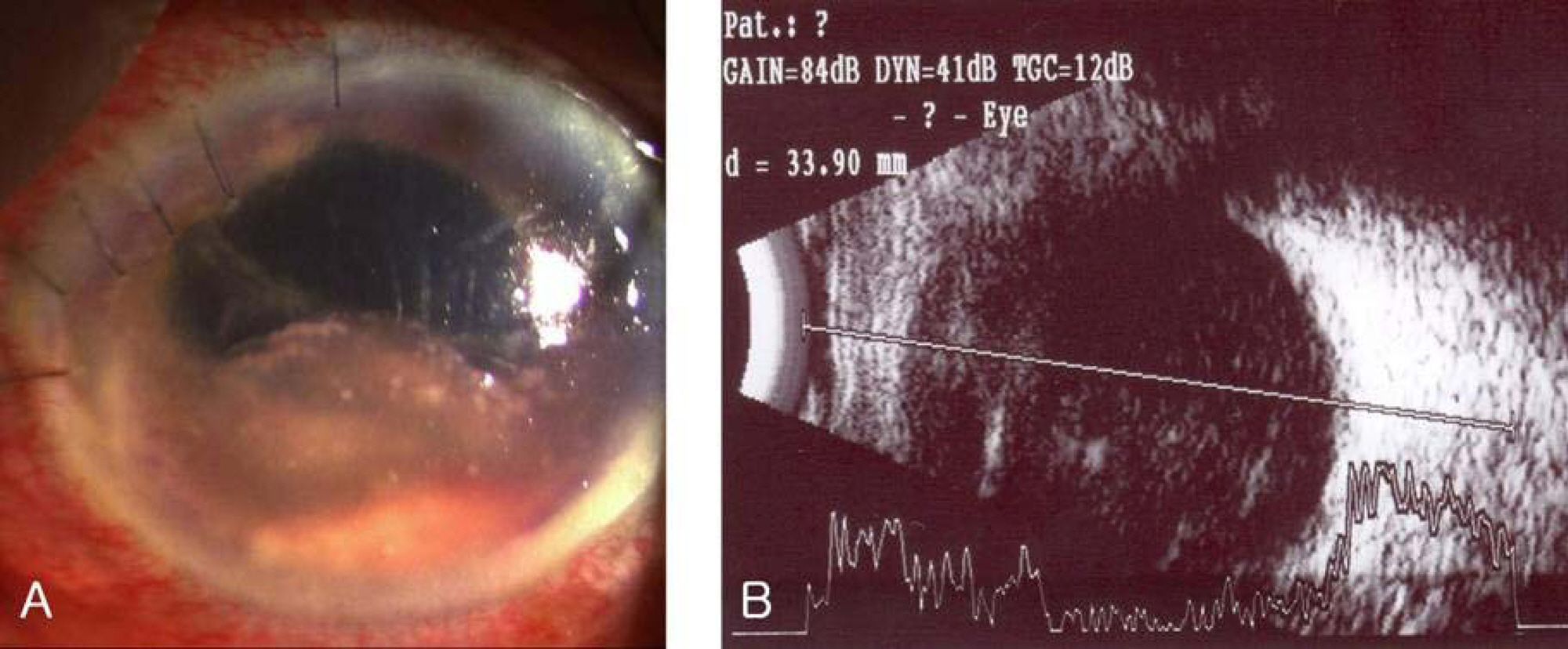
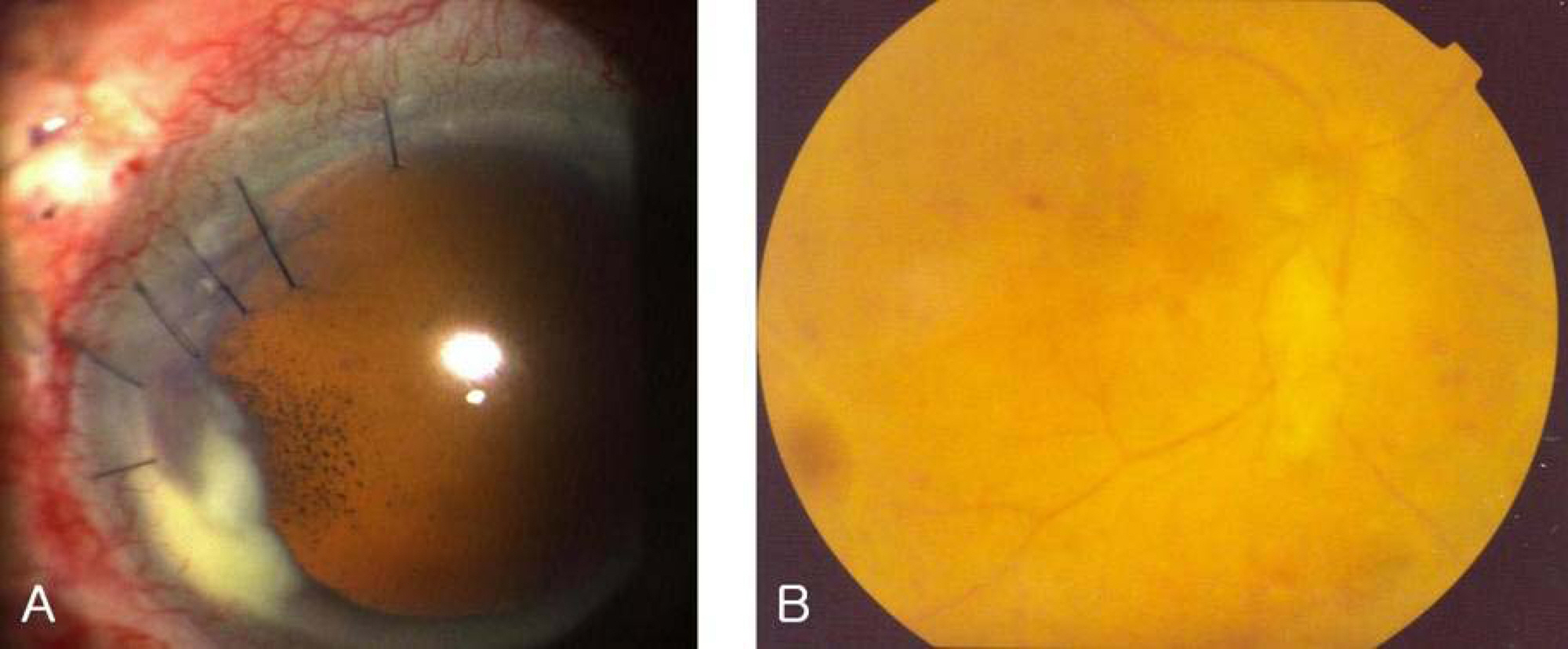
A 73-year-old male who developed endophthalmitis after cataract surgery was treated with intravitreal vancomycin and ceftazidime injection after aqueous and vitreous cultures were done. The condition were not improve after intravitreal injection, and the culture showed Penicillium species. Fungal endophthalmitis was diagnosed and pars plana vitrectomy, intraocular lens removal, and intravitreal amphotericin B injection were performed. However, a progressive worsening of the ocular condition was observed, and the patient was transferred to our hospital. At initial visit, the best corrected visual activity was hand movement. The hypopyon and thick exudative membrane filled the anterior chamber. Pars plana vitrectomy and intravitreal voriconazole injection were performed under the diagnosis of drug-resistant Penicillium endophthalmitis. The condition improved after the operation, and there was no recurrence of endophthalmitis until four months after vitrectomy.
CONCLUSIONS
Voriconazole is useful in the treatment of drug-resistant fungal endophthalmitis.
MeSH Terms
Figure
Reference
-
References
1. Aaberg TM Jr, Flynn HW Jr, Schiffman J, Newton J. Nosocomial acute-onset postoperative endophthalmitis survey. A 10-year review of incidence and outcomes. Ophthalmology. 1998; 105:1004–10.2. Kresloff MS, Castellarin AA, Zarbin MA. Endophthalmitis. Surv Ophthalmol. 1998; 43:193–224.
Article3. Narang S, Gupta A, Gupta V, et al. Fungal endophthalmitis following cataract surgery: clinical presentation, microbiological spectrum, and outcome. Am J Ophthalmol. 2001; 132:609–17.
Article4. Souri EN, Green WR. Intravitreal amphotericin B toxicity. Am J Ophthalmol. 1974; 78:77–81.
Article5. O'Day DM, Foulds G, Williams TE, et al. Ocular uptake of fluconazole following oral administration. Arch Ophthalmol. 1990; 108:1006–8.6. Schulman JA, Peyman G, Fiscella R, et al. Toxicity of intravitreal injection of fluconazole in the rabbit. Can J Ophthalmol. 1987; 22:304–6.7. O'Day DM, Head WS, Robinson RD, et al. Intraocular penetration of systemically administered antifungal agents. Curr Eye Res. 1985; 4:131–4.8. Savani DV, Perfect JR, Cobo LM, Durack DT. Penetration of new azole compounds into the eye and efficacy in experimental Candida endophthalmitis. Antimicrob Agents Chemother. 1987; 31:6–10.
Article9. Marangon FB, Miller D, Giaconi JA, Alfonso EC. In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. Am J Ophthalmol. 2004; 137:820–5.
Article10. Espinel-Ingroff A, Boyle K, Sheehan DJ. In vitro antifungal activities of voriconazole and reference agents as determined by NCCLS methods: review of literature. Mycopathologia. 2001; 150:101–15.11. Hariprasad SM, Mieler WF, Holz ER, et al. Determination of vitreous, aqueous, and plasma concentration of orally administered voriconazole in humans. Arch Ophthalmol. 2004; 122:42–7.12. Rippon JW. Medical mycology. 2nd ed.1. Philadelphia: WB Saunders;1982. p. 659–94.13. Yang KJ, Kim SJ, Park BI. Mycotic flora in normal conjunctival sac. J Korean Ophthalmol Soc. 1989; 30:9–16.14. Arora R, Gupta S, Raina UK, et al. Penicillium keratitis in vernal Keratoconjunctivitis. Indian J Ophthalmol. 2002; 50:215–6.15. Hahn YH, Byun KS, Chang MW. A case of penicillium keratitis. J Korean Ophthalmol Soc. 1995; 36:373–7.16. Galland F, le Goff L, Conrath J, Ridings B. Penicillium chrysogenum endophthalmitis: a case report. J Fr Ophtalmol. 2004; 27:264–6.17. Eschete ML, King JW, West BC, Oberle A. Penicillium chrysogenum endophthalmitis. Mycopathologia. 1981; 74:125–7.
Article18. Savir H, Henig E, Lehrer N. Exogenous mycotic infections of the eye and adnexia. Ann Ophthalmol. 1978; 10:1013–8.19. Kappe R. Antifungal activity of the new azole UK-109, 496 (voriconazole). Mycoses. 1999; 42:S83–6.
Article20. Imwidthaya P, Thipsuvan K, Chaiprasert A, et al. Penicillium marneffei: types and drug susceptibility. Mycopathologia. 2001; 149:109–15.21. McGinnis MR, Nordoff NG, Ryder NS, Nunn GB. In vitro comparison of terbinafine and itraconazole against Penicillium marneffei. Antimicrob Agents Chemother. 2000; 44:1407–8.22. Ghannoum MA, Kuhn DM. Voriconazole-better chances for patients with invasive mycosis. Eur J Med Res. 2002; 7:242–56.23. Gao H, Pennesi ME, Shah K, et al. Intravitreal voriconazole: an electroretinographic and histopathologic study. Arch Ophthalmol. 2004; 122:1687–92.24. Sen P, Gopal L, Sen PR. Intravitreal voriconazole for drug-resistant fungal endophthalmitis: case series. Retina. 2006; 26:935–9.25. Kramer M, Kramer MR, Blau H, et al. Intravitreal voriconazole for the treatment of endogenous Aspergillus endophthalmitis. Ophthalmology. 2006; 113:1184–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Topical and Oral Voriconazole in the Treatment of Fungal Keratitis
- A Case of Postoperative Bacterial Endophthalmitis after Successful Treatment of Suspected Iatrogenic Fungal Endophthalmitis
- A Case of Fungal Endophthalmitis after Having Received Extraction of Wisdom Tooth in Healthy Woman
- Two Cases of Ischemic Retinopathy due to Intravitreal Gentamicin Toxicity after Vitrectomy
- A Case of Pseudomonas Aeruginosa Endophthalmitis Treated with Intravitreal Ceftazidime Injection