J Korean Fract Soc.
2011 Oct;24(4):347-353.
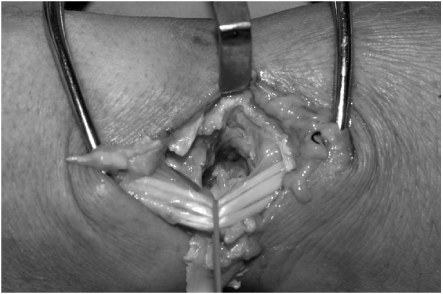
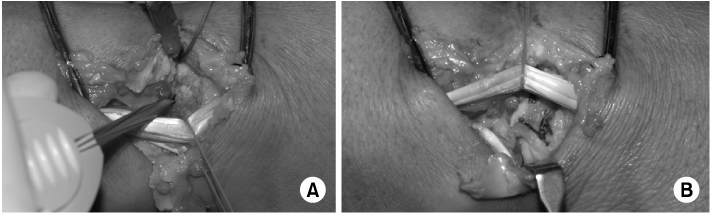
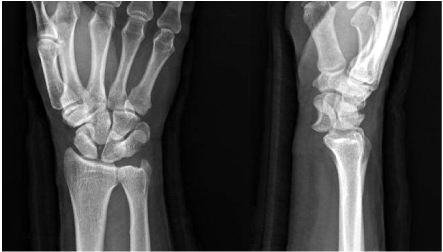
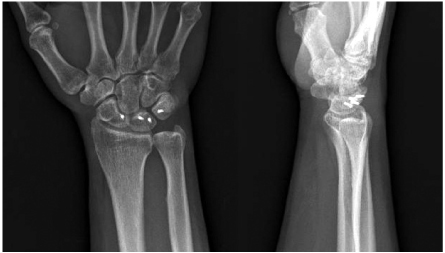
Surgical Treatment of the Perilunate Dislocation and the Lunate Dislocation with Dorsal Approach
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA University CHA Bundang Medical Center, Seongnam, Korea.
- 2Department of Orthopaedic Surgery, CHA University CHA Gumi Medical Center, Gumi, Korea. hsoohong@cha.ac.kr
Abstract
- PURPOSE
To evaluate the clinical and radiologic outcomes of the perilunate dislocation and the lunate dislocation which were managed surgically through a dorsal approach.
MATERIALS AND METHODS
Retrospective reviews of the 13 patients who had minimum 1-year follow-up after surgical treatment through isolated dorsal approach for their perilunate dislocations or the lunate dislocations were performed. The case that dislocated lunate migrated proximally through the wrist was excluded in this series. We evaluated the DASH score in questionnaire method and Mayo wrist score to analyze the clinical outcomes. Radiologic results were investigated by measurement of the scapho-lunate angle, and fracture union was also evaluated in the case of trans-scaphoid dislocation.
RESULTS
The mean DASH Score was 16.3 points (range, 10.8~26.7 points) and the mean Mayo wrist score was 79 points (range, 65~90 points) at the final follow-up. There were 2 cases of excellent, 7 cases of good and 4 cases of fair in the Mayo wrist score. On the radiologic analysis, the mean scapho-lunate angle was 49.0degrees (range, 35~55degrees) and all cases were within the normal range. All cases of the trans-scaphoid perilunate dislocation achieved bone union.
CONCLUSION
Author's cases showed satisfactory outcomes in clinically and radiologically. Isolated dorsal approach could give anatomical reduction and appropriate internal fixation in treatment of the perilunate dislocations and the lunate dislocations except the rare case of proximal migration of the lunate through the wrist.
MeSH Terms
Figure
Reference
-
1. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001. 14:128–146.2. Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am. 2008. 33:1424–1432.
Article3. Chung MS, Lee CS, Suk SI. Clinical study of the trans-scaphoid perilunar dislocation. J Korean Soc Fract. 1988. 1:43–53.
Article4. Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987. 214:136–147.5. Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am. 2010. 35:62–68.
Article6. Green DP, O'Brien ET. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am. 1978. 3:250–265.
Article7. Herzberg G. Acute dorsal trans-scaphoid perilunate dislocations: open reduction and internal fixation. Tech Hand Up Extrem Surg. 2000. 4:2–13.8. Hudak PL, Amadio PC, Bombardier C. The Upper Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. Am J Ind Med. 1996. 29:602–608.
Article9. Inoue G, Imaeda T. Management of trans-scaphoid perilunate dislocations. Herbert screw fixation, ligamentous repair and early wrist mobilization . Arch Orthop Trauma Surg. 1997. 116:338–340.
Article10. Kim DH, Shin JY, Shin KC. The treatment of volar lunate dislocation and perilunar dislocation. J Korean Soc Fract. 1995. 8:902–907.11. Knoll VD, Allan C, Trumble TE. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am. 2005. 30:1145–1152.
Article12. Moneim MS, Hofammann KE 3rd, Omer GE. Transscaphoid perilunate fracture-dislocation. Result of open reduction and pin fixation. Clin Orthop Relat Res. 1984. 190:227–235.13. Park JW, Lee KS, Kim SK, et al. Operative treatment of perilunar fracture dislocation. J Korean Soc Surg Hand. 2002. 7:23–27.14. Sauder DJ, Athwal GS, Faber KJ, Roth JH. Perilunate injuries. Orthop Clin North Am. 2007. 38:279–288.
Article15. Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, Tomaino MM, Herndon JH. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am. 1997. 22:49–56.
Article16. Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004. 29:412–417.
Article17. Viegas SF, Bean JW, Schram RA. Transscaphoid fracture/dislocations treated with open reduction and Herbert screw internal fixation. J Hand Surg Am. 1987. 12:992–999.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Treatment of Volar Iunate Dislocation and Perilunar Dislocation
- Perilunate Dislocation and Perilunate Fracture-Dislocation
- Multiple Flexor Tendon Ruptures with Compression Neuropathy at Neglected Volar Lunate Dislocation
- Volar Perilunate Dislocation: A case report
- Perilunate Dislocations and Fracture-Dislocations