J Periodontal Implant Sci.
2013 Dec;43(6):283-290.
Association of gingival biotype with the results of scaling and root planing
- Affiliations
-
- 1Department of Periodontology, Wonkwang University School of Dentistry, Iksan, Korea. hkperio@wku.ac.kr
- 2Wonkwang Dental Research Institute, Wonkwang University School of Dentistry, Iksan, Korea.
Abstract
- PURPOSE
The concept of gingival biotype has been used as a predictor of periodontal therapy outcomes since the 1980s. In the present study, prospective and controlled experiments were performed to compare periodontal pocket depth (PPD) reduction and gingival shrinkage (GSH) after scaling and root planing (SRP) according to gingival biotype.
METHODS
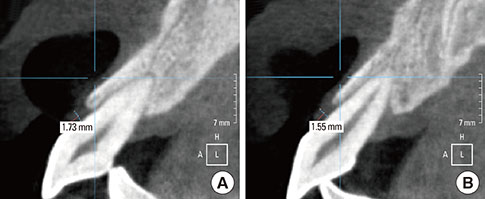
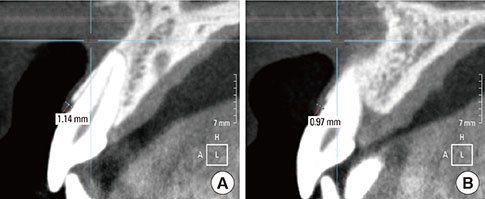
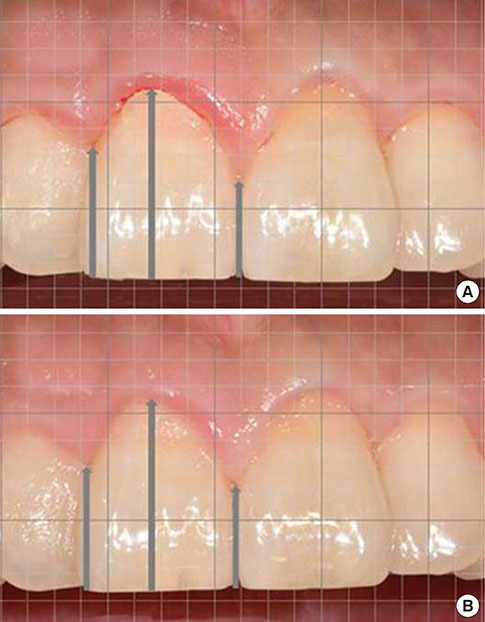
Twenty-five patients diagnosed with chronic periodontitis participated in the present study. The PPD and GSH of the labial side of the maxillary anterior teeth (from the right canine to the left canine) were evaluated at baseline and 3 months after SRP. Changes in the PPD following SRP were classified into 4 groups according to the gingival thickness and initial PPD. Two more groups representing normal gingival crevices were added in evaluation of the GSH. The results were statistically analyzed using the independent t-test.
RESULTS
In the end, 16 patients participated in the present study. With regard to PPD reduction, there were no significant differences according to gingival biotype (P>0.05). Likewise, sites with a PPD of over 3 mm failed to show any significant differences in the GSH (P>0.05). However, among the sites with a PPD of under 3 mm, those with the thin gingival biotype showed more GSH (P<0.05).
CONCLUSIONS
PPD changes after SRP were not affected by gingival biotype with either shallow or deep periodontal pockets. GSH also showed equal outcomes in all the groups without normal gingival crevices. The results of SRP seem not to differ according to gingival biotype.
Keyword
MeSH Terms
Figure
Reference
-
1. Seibert J, Lindhe J. Esthetics and periodontal therapy. In : Lindhe J, editor. Textbook of clinical periodontology. 2nd ed. Copenhagen: Munksgaard;1989. p. 477–514.2. Muller HP, Eger T. Gingival phenotypes in young male adults. J Clin Periodontol. 1997; 24:65–71.
Article3. Olsson M, Lindhe J, Marinello CP. On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol. 1993; 20:570–577.
Article4. Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month clinical wound healing study. J Periodontol. 2001; 72:841–848.
Article5. Olsson M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisors. J Clin Periodontol. 1991; 18:78–82.
Article6. Weisgold AS. Contours of the full crown restoration. Alpha Omegan. 1977; 70:77–89.7. Romeo E, Lops D, Rossi A, Storelli S, Rozza R, Chiapasco M. Surgical and prosthetic management of interproximal region with single-implant restorations: 1-year prospective study. J Periodontol. 2008; 79:1048–1055.
Article8. Baldi C, Pini-Prato G, Pagliaro U, Nieri M, Saletta D, Muzzi L, et al. Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage?: a 19-case series. J Periodontol. 1999; 70:1077–1084.
Article9. Lindhe J, Westfelt E, Nyman S, Socransky SS, Heijl L, Bratthall G. Healing following surgical/non-surgical treatment of periodontal disease: a clinical study. J Clin Periodontol. 1982; 9:115–128.
Article10. Stahl SS, Slavkin HC, Yamada L, Levine S. Speculations about gingival repair. J Periodontol. 1972; 43:395–402.
Article11. Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy: I. Moderately advanced periodontitis. J Clin Periodontol. 1981; 8:57–72.
Article12. Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy: II. Severely advanced periodontitis. J Clin Periodontol. 1984; 11:63–76.
Article13. Fu JH, Lee A, Wang HL. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants. 2011; 26:499–508.14. Fredsen A. Mechanical oral hygiene practices. In : Loe H, Kleinman DV, editors. Dental plaque control measures and oral hygiene practices: proceedings from a state-of-the-science workshop. Oxford: IRL Press;1986. p. 93–116.15. Claffey N, Shanley D. Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol. 1986; 13:654–657.
Article16. Cosyn J, Hooghe N, De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol. 2012; 39:582–589.17. Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013; 15:847–857.
Article18. Cosyn J, Eghbali A, De Bruyn H, Dierens M, De Rouck T. Single implant treatment in healing versus healed sites of the anterior maxilla: an aesthetic evaluation. Clin Implant Dent Relat Res. 2012; 14:517–526.
Article19. Chou CH, Mo JJ, Si MS, Gu YX, Du J, Zhang ZY, et al. Papilla alteration in different gingival biotypes at single implant-supported restoration in anterior maxilla. Shanghai Kou Qiang Yi Xue. 2012; 21:541–545.20. De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009; 36:428–433.
Article21. Anderegg CR, Metzler DG, Nicoll BK. Gingiva thickness in guided tissue regeneration and associated recession at facial furcation defects. J Periodontol. 1995; 66:397–402.
Article22. Zigdon H, Machtei EE. The dimensions of keratinized mucosa around implants affect clinical and immunological parameters. Clin Oral Implants Res. 2008; 19:387–392.
Article23. Aimetti M, Massei G, Morra M, Cardesi E, Romano F. Correlation between gingival phenotype and Schneiderian membrane thickness. Int J Oral Maxillofac Implants. 2008; 23:1128–1132.24. Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent. 2011; 31:345–354.25. Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003; 74:557–562.
Article26. Greenberg J, Laster L, Listgarten MA. Transgingival probing as a potential estimator of alveolar bone level. J Periodontol. 1976; 47:514–517.
Article27. Muller HP, Barrieshi-Nusair KM, Kononen E. Repeatability of ultrasonic determination of gingival thickness. Clin Oral Investig. 2007; 11:439–442.
Article28. Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent. 2010; 30:237–243.29. Eger T, Muller HP, Heinecke A. Ultrasonic determination of gingival thickness. Subject variation and influence of tooth type and clinical features. J Clin Periodontol. 1996; 23:839–845.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gingival color change after scaling & subgingival root planing
- The Effectiveness of Subgingival Scaling and Root Planing via Closed Approach in Calculus Removal
- Scaling and Root Planing with Concomitant Subgingival Curettage
- Clinical Evaluation After Periodontal Flap Surgery with/without Non-Surgical Periodontal Therapy
- Effect of tetracycline-HCl root conditioning on gingival epithelial cell attachment to root surface