J Dent Anesth Pain Med.
2016 Jun;16(2):123-129. 10.17245/jdapm.2016.16.2.123.
A survey of the intravenous sedation status in one provincial dental clinic center for the disabled in Korea
- Affiliations
-
- 1Department of Pediatric Department, School of Dentistry, Dankook University, Cheonan, Korea. jbkim0222@dankook.ac.kr
- 2Department of Anesthesiology, School of Dentistry, Dankook University, Cheonan, Korea.
- KMID: 2328855
- DOI: http://doi.org/10.17245/jdapm.2016.16.2.123
Abstract
- BACKGROUND
The objective of the present study was to examine the status of patients who had received dental treatment under intravenous (IV) sedation at Chungnam Dental Clinic for the Disabled in Korea from its inception to the present time, and to review the analysis results.
METHODS
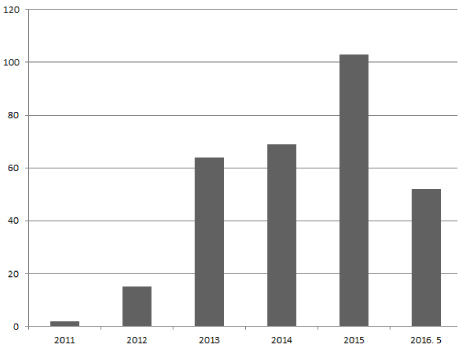
Retrospective analysis was performed on 305 cases of patients who had received dental treatments under IV sedation between January 2011 and May 2016. The analysis examined the patient's sex, age, primary reason for IV sedation, duration of anesthesia and dental treatment, type of dental treatment performed, number of clinical departments involved in the dental treatment and level of multidisciplinary cooperation, and annual trends.
RESULTS
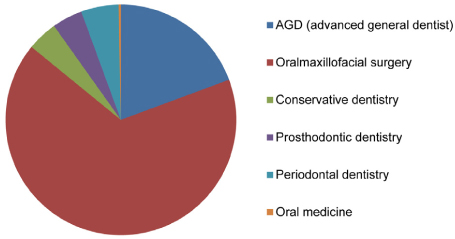
Most dental treatments using intravenous sedation were performed on medically disabled patients or dentally disabled patients with an extreme gag reflex or dental phobia. The mean duration of IV sedation was 72.5 min, while the mean duration of treatment was 58.0 min. The types of dental treatments included surgical treatment (n = 209), periodontal treatment (n = 28), prosthodontic treatment (n = 28), restorative treatment (n = 23), implant surgery (n = 22), endodontic treatment (n = 9), reduction of temporomandibular joint dislocation (n = 1), and treatment of traumatic injuries (n = 1), with treatments mostly performed on adult patients.
CONCLUSIONS
With increasing demand for minimally painful treatment, cases using IV sedation are on an upward trend and are expected to continue to increase.
MeSH Terms
Figure
Reference
-
1. Dionne RA, Yagiela JA, Moore PA, Gonty A, Zuniga J, BEIRNE OR, et al. Comparing efficacy and safety of four intravenous sedation regimens in dental outpatients. J Am Dent Assoc. 2001; 132:740–751.
Article2. Kwak HJ, Kim JY, Kwak YL, Park WS, Lee KC. Comparison of a bolus of fentanyl with an infusion of alfentanil during target-controlled propofol infusion in third molar extraction under conscious sedation. J Oral Maxillofac Surg. 2006; 64:1577–1582.
Article3. Whitwam J. Co-induction of anaesthesia: Day-case surgery. Eur J Anaesthesiol Suppl. 1995; 12:25–34.4. You YS, Kim JS, Kim SO. A survey of the outpatient general anesthesia and dental treatment in chungnam dental clinic for the disabled. J Korean Dent Soc Anesthesiol. 2011; 11:133–140.
Article5. Kim SO. A survey of general anesthesia, sevoflurane sedation and intravenous sedation in chungnam dental clinic for the disabled. J Korean Acad Pediatr Dent. 2013; 40:28–39.
Article6. McMurray T, Johnston J, Milligan K, Grant I, Mackenzie S, Servin F, et al. Propofol sedation using diprifusortm target-controlled infusion in adult intensive care unit patients. Anaesthesia. 2004; 59:636–641.
Article7. De Castro V, Godet G, Mencia G, Raux M, Coriat P. Target-controlled infusion for remifentanil in vascular patients improves hemodynamics and decreases remifentanil requirement. Anesth Analg. 2003; 96:33–38.
Article8. O JE, Kim JS, Kim SO. A study of intravenous sedation in dankook university dental hospital. J Korean Dent Soc Anesthesiol. 2013; 13:1–7.
Article9. O SR, Lee J. Intravenous sedation using propofol and midazolam in the exaggerated gag reflex patient's dental implant treatment. J Korean Dent Soc Anesthesiol. 2010; 10:27–33.
Article10. Sebel PS, Lowdon JD. Propofol: A new intravenous anesthetic. Anesthesiology. 1989; 71:260–277.11. Tesniere A, Servin F. Intravenous techniques in ambulatory anesthesia. Anesthesiol Clin North America. 2003; 21:273–288.
Article12. Barash PG, Cullen BF, Stoelting RK. Clinical anesthesia. 5th ed. Lippincott Williams Willkins;2006. p. 269p. 270p. 341–342. p. 371p. 37513. Glass PS, Dyar OJ, Jacobs JR, Reves JG. Intravenous anesthetic drugs: Infusion regimens. Int Anesthesiol Clin. 1991; 29:73–82.
Article14. Keidan I, Berkenstadt H, Sidi A, Perel A. Propofol/remifentanil versus propofol alone for bone marrow aspiration in paediatric haemato-oncological patients. Paediatr Anaesth. 2001; 11:297–301.
Article15. Dar AQ, Shah ZA. Anesthesia and sedation in pediatric gastrointestinal endoscopic procedures: A review. World J Gastrointest Endosc. 2010; 2:257–262.
Article16. Craig DC, Boyle CA, Fleming GJ, Palmer P. A sedation technique for implant and periodontal surgery. J Clin Periodontol. 2000; 27:955–959.
Article17. Pirwitz B, Schlender M, Enders A, Knauer O. [risks and complications anesthesia with intubation during dental treatment]. Rev Stomatol Chir Maxillofac. 1998; 98:387–389.18. Saunders RM, Cameron J. Psychogenic gagging: Identification and treatment recommendations. Compend Contin Educ Dent. 1997; 18:430–433.19. Kramer RB, Braham RL. The management of the chronic or hysterical gagger. ASDC J Dent Child. 1977; 44:111–116.20. Weinstein P. Treating fearful dental patients: a patient management handbook. 2nd ed. University of Washington;1996.21. Hodgkiss A. The puzzle of pain. Med Hist. 1996; 40:114–115.22. Jones A, Bentler P, Petry G. The reduction of uncertainty concerning future pain. Journal of abnormal psychology. 1966; 71:87.
Article23. van Wijk AJ, Hoogstraten J. Reducing fear of pain associated with endodontic therapy. Int Endod J. 2006; 39:384–388.
Article24. Holzman RS, Cullen DJ, Eichhorn JH, Philip JH. Guidelines for sedation by nonanesthesiologists during diagnostic and therapeutic procedures. The risk management committee of the department of anaesthesia of harvard medical school. J Clin Anesth. 1994; 6:265–276.25. Yoshida H, Ayuse T, Ishizaka S, Ishitobi S, Nogami T, Oi K. Management of exaggerated gag reflex using intravenous sedation in prosthodontic treatment. Tohoku J Exp Med. 2007; 212:373–378.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Survey of the sevoflurane sedation status in one provincial dental clinic center for the disabled
- A Survey of the Sedation or Outpatient General Anesthesia in Department of Pediatric Dentistry, Chonnam National University Dental Hospital and Gwangju Dental Clinic for the Disabled
- Application of sevoflurane inhalation sedation in dental treatment: a mini review
- Introduction of Sedation Clinic at Department of Dentistry in Hanyang University Medical Center (I)
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)