J Korean Surg Soc.
2012 Jun;82(6):374-379.
Early treatment outcome of isolated calf vein thrombosis after total knee arthroplasty
- Affiliations
-
- 1Division of Vascular/Endovascular Surgery, Department of Surgery, Daegu Catholic University Medical Center, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 2Division of Transplantation and Vascular Surgery, Department of Surgery, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea. shuh@knu.ac.kr
- 3Department of Orthopedic Surgery, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea.
Abstract
- PURPOSE
In contrast to proximal deep vein thrombosis (DVT), the treatment of isolated calf vein thrombosis (ICVT) remains controversial. This study aimed to investigate early treatment outcomes of ICVT after total knee arthroplasty (TKA).
METHODS
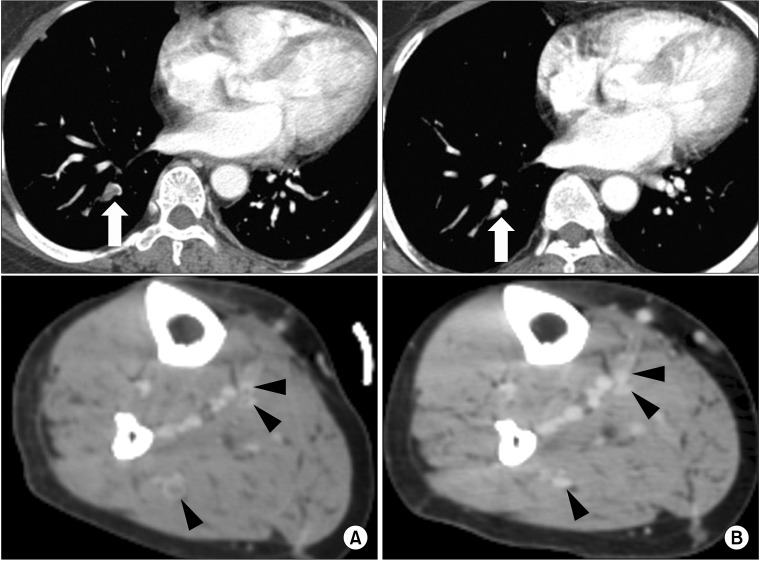
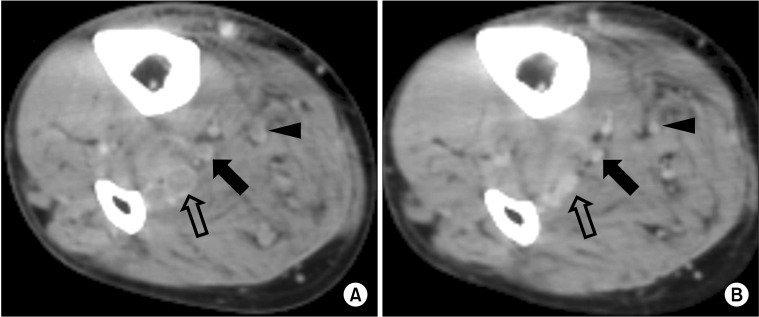
Medical records of 313 patients who underwent TKA from October 2007 to December 2009 were retrospectively reviewed. A DVT-computed tomography (CT) was performed 7 days after surgery. ICVT was identified in 76 limbs of 73 patients. Of them, follow-up DVT-CT was available in 39 limbs of 37 patients. The patients with ICVTs were categorized into two groups: oral anticoagulation group (group I, 17 patients with 18 limbs) and conservative treatment group (group II, 20 patients with 21 limbs). Group I received an oral vitamin K antagonist for 3 to 6 months following low molecular weight heparin. Change of thrombus extent and development of pulmonary embolism (PE) was assessed in follow-up DVT-CT.
RESULTS
Mean age was 68 years and 95% were female. Of 39 limbs with ICVT, 16 (41%) involved major lower leg veins (posterior tibial vein or peroneal vein), 13 (33%) involved muscular veins (soleal vein or gastrocnemius vein) and 10 (26%) involved both. During 1 to 6 months, follow-up DVT-CT revealed complete thrombus resolution in all limbs and there was no proximal propagation of thrombus or PE in both groups.
CONCLUSION
There is no evidence of DVT propagation or newly developed PE in the conservative treatment group. This result suggests that anticoagulation therapy for ICVT patients without PE after TKA may not be mandatory.
MeSH Terms
Figure
Reference
-
1. Gottlieb RH, Widjaja J. Clinical outcomes of untreated symptomatic patients with negative findings on sonography of the thigh for deep vein thrombosis: our experience and a review of the literature. AJR Am J Roentgenol. 1999; 172:1601–1604. PMID: 10350297.
Article2. Oishi CS, Grady-Benson JC, Otis SM, Colwell CW Jr, Walker RH. The clinical course of distal deep venous thrombosis after total hip and total knee arthroplasty, as determined with duplex ultrasonography. J Bone Joint Surg Am. 1994; 76:1658–1663. PMID: 7962026.
Article3. Ohgi S, Tachibana M, Ikebuchi M, Kanaoka Y, Maeda T, Mori T. Pulmonary embolism in patients with isolated soleal vein thrombosis. Angiology. 1998; 49:759–764. PMID: 9756428.
Article4. Lohr JM, Kerr TM, Lutter KS, Cranley RD, Spirtoff K, Cranley JJ. Lower extremity calf thrombosis: to treat or not to treat? J Vasc Surg. 1991; 14:618–623. PMID: 1942369.
Article5. Sevitt S, Gallagher N. Venous thrombosis and pulmonary embolism: a clinico-pathological study in injured and burned patients. Br J Surg. 1961; 48:475–489. PMID: 13750445.
Article6. Giachino A. Relationship between deep-vein thrombosis in the calf and fatal pulmonary embolism. Can J Surg. 1988; 31:129–130. PMID: 3349377.7. Guias B, Simoni G, Oger E, Lemire A, Leroyer C, Mottier D, et al. Calf muscle venous thrombosis and pulmonary embolism. J Mal Vasc. 1999; 24:132–134. PMID: 10399646.8. Hollerweger A, Macheiner P, Rettenbacher T, Gritzmann N. Sonographic diagnosis of thrombosis of the calf muscle veins and the risk of pulmonary embolism. Ultraschall Med. 2000; 21:66–72. PMID: 10838706.9. Philbrick JT, Becker DM. Calf deep venous thrombosis: a wolf in sheep's clothing? Arch Intern Med. 1988; 148:2131–2138. PMID: 3052345.
Article10. Deitcher SR, Caprini JA. Calf deep venous thrombosis should be treated with anticoagulation. Med Clin North Am. 2003; 87:1157–1164. PMID: 14680297.
Article11. Lohr JM, James KV, Deshmukh RM, Hasselfeld KA, Allastair B. Karmody Award. Calf vein thrombi are not a benign finding. Am J Surg. 1995; 170:86–90. PMID: 7631940.12. Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U. Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet. 1985; 2:515–518. PMID: 2863541.
Article13. Lautz TB, Abbas F, Walsh SJ, Chow C, Amaranto DJ, Wang E, et al. Isolated gastrocnemius and soleal vein thrombosis: should these patients receive therapeutic anticoagulation? Ann Surg. 2010; 251:735–742. PMID: 19858700.14. Wang CJ, Wang JW, Weng LH, Hsu CC, Lo CF. Outcome of calf deep-vein thrombosis after total knee arthroplasty. J Bone Joint Surg Br. 2003; 85:841–844. PMID: 12931802.
Article15. Solis MM, Ranval TJ, Nix ML, Eidt JF, Nelson CL, Ferris EJ, et al. Is anticoagulation indicated for asymptomatic postoperative calf vein thrombosis? J Vasc Surg. 1992; 16:414–418. PMID: 1522645.
Article16. Masuda EM, Kessler DM, Kistner RL, Eklof B, Sato DT. The natural history of calf vein thrombosis: lysis of thrombi and development of reflux. J Vasc Surg. 1998; 28:67–73. PMID: 9685132.
Article17. Meissner MH, Caps MT, Bergelin RO, Manzo RA, Strandness DE Jr. Propagation, rethrombosis and new thrombus formation after acute deep venous thrombosis. J Vasc Surg. 1995; 22:558–567. PMID: 7494356.
Article18. MacDonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. J Vasc Surg. 2003; 37:523–527. PMID: 12618686.
Article19. Schwarz T, Schmidt B, Beyer J, Schellong SM. Therapy of isolated calf muscle vein thrombosis with low-molecular-weight heparin. Blood Coagul Fibrinolysis. 2001; 12:597–599. PMID: 11685050.
Article20. Schwarz T, Buschmann L, Beyer J, Halbritter K, Rastan A, Schellong S. Therapy of isolated calf muscle vein thrombosis: a randomized, controlled study. J Vasc Surg. 2010; 52:1246–1250. PMID: 20630682.
Article21. Browse NL, Clemenson G, Thomas ML. Is the postphlebitic leg always postphlebitic? Relation between phlebographic appearances of deep-vein thrombosis and late sequelae. Br Med J. 1980; 281:1167–1170. PMID: 7427621.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Foot Pump on Prevention of Deep Vein Thrombosis Following Total Knee Arthroplasty
- Deep Vein Thrombosis after Total Knee Replacement: Incidence and correlation with clinical risk factors
- May–Thurner Syndrome after Total Knee Arthroplasty
- Isolated Posterior Malleolar Fracture of Ankle Occurring with Total Knee Arthroplasty in Severe Osteoporotic Patient
- Compartment Syndrome Following Total Knee Arthroplasty: Clinical Results of Late Fasciotomy