J Korean Surg Soc.
2010 Sep;79(3):189-195.
Clinical Evaluation of Immediate Removal of Transurethral Catheter after Radical Gastrectomy: A Result of Feasibility Study
- Affiliations
-
- 1Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, Catholic University of Korea, Seoul, Korea. hmjeon@catholic.ac.kr
Abstract
- PURPOSE
Transurethral catheterization is restricted to fewer procedures and a limited time with an increase in enhanced recovery after surgery (ERAS) programs or fast-track surgical procedures. We aim to evaluate the feasibility of immediate removal of transurethral catheter in hemodymically stable patients undergoing radical gastrectomy prior to a prospective randomized control trial.
METHODS
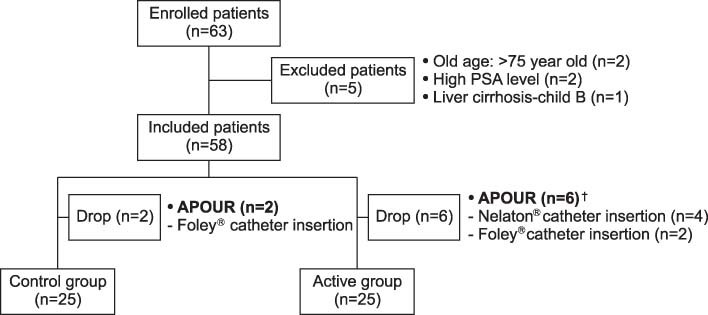
A total 63 gastric cancer patients undergoing elective radical gastrectomy were enrolled in a feasibility study. Patients were randomized to either the active group (immediate removal group) or control group (removal at postoperative day 1 group) with blinding, and 58 patients were finally included. Amount of residual and voiding urine, operative factors (operation time, infused fluid, urine output, and blood loss), first voiding discomfort level, urinary discomfort score, and urine analysis were measured.
RESULTS
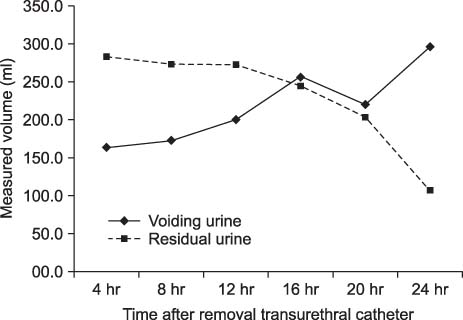
In the active group, the self-voiding volume and residual urine volume measured nearly equal (256 ml vs 244 ml) at 16 hours after transurethral catheter removal. The discomfort score of first self-voiding was lower in active group (P=0.041). Regarding urinary discomfort at postoperative day 2 and the urine analysis at postoperative day 5, there were no significant differences between the 2 groups.
CONCLUSION
Immediate removal of the transurethral catheter could be feasible and safe in hemodynamically stable patients undergoing radical gastrectomy in aspects of ERAS programs. A prospective randomized controlled trial would be scheduled for acceptable evidence.
MeSH Terms
Figure
Reference
-
1. Baldini G, Bagry H, Aprikian A, Carli F. Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology. 2009. 110:1139–1157.2. Nasr AM, ElBigawy AF, Abdelamid AE, Al-Khulaidi S, Al-Inany HG, Sayed EH. Evaluation of the use vs nonuse of urinary catheterization during cesarean delivery: a prospective, multicenter, randomized controlled trial. J Perinatol. 2009. 29:416–421.3. Baan AH, Vermeulen H, van der Meulen J, Bossuyt P, Olszyna D, Gouma DJ. The effect of suprapubic catheterization versus transurethral catheterization after abdominal surgery on urinary tract infection: a randomized controlled trial. Dig Surg. 2003. 20:290–295.4. Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008. 248:189–198.5. Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002. 183:630–641.6. Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999. 79:231–252.7. Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 2002. 359:1812–1818.8. Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003. 238:641–648.9. Pavlin DJ, Pavlin EG, Gunn HC, Taraday JK, Koerschgen ME. Voiding in patients managed with or without ultrasound monitoring of bladder volume after outpatient surgery. Anesth Analg. 1999. 89:90–97.10. Keita H, Diouf E, Tubach F, Brouwer T, Dahmani S, Mantz J, et al. Predictive factors of early postoperative urinary retention in the postanesthesia care unit. Anesth Analg. 2005. 101:592–596.11. Mulroy MF, Salinas FV, Larkin KL, Polissar NL. Ambulatory surgery patients may be discharged before voiding after short-acting spinal and epidural anesthesia. Anesthesiology. 2002. 97:315–319.12. Petros JG, Mallen JK, Howe K, Rimm EB, Robillard RJ. Patient-controlled analgesia and postoperative urinary retention after open appendectomy. Surg Gynecol Obstet. 1993. 177:172–175.13. Lamonerie L, Marret E, Deleuze A, Lembert N, Dupont M, Bonnet F. Prevalence of postoperative bladder distension and urinary retention detected by ultrasound measurement. Br J Anaesth. 2004. 92:544–546.14. Gonullu NN, Gonullu M, Utkan NZ, Dulger M, Gokgoz S, Karsli B. Postoperative retention of urine in general surgical patients. Eur J Surg. 1993. 159:145–147.15. Stevens E. Bladder ultrasound: avoiding unnecessary catheterizations. Medsurg Nurs. 2005. 14:249–253.16. Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary-tract infection. N Engl J Med. 1982. 307:637–642.17. Akhtar MS, Beere DM, Wright JT, MacRae KD. Is bladder catheterization really necessary before laparoscopy? Br J Obstet Gynaecol. 1985. 92:1176–1178.18. Shapiro J, Hoffmann J, Jersky J. A comparison of suprapubic and transurethral drainage for postoperative urinary retention in general surgical patients. Acta Chir Scand. 1982. 148:323–327.19. Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000. 160:678–682.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Catheter Removal after Radical Retropubic Prostatectomy
- Clinical experience of early catheter removal following transurethral resection of the prostate
- Catheter Removal on the First Day after Transurethral Prostatectomy: Probability of Successful Voiding and Its Safety
- Breakage of a thoracic epidural catheter during its removal: A case report
- Transient Cortical Blindness after Removal of Subclavian Vein Catheter