J Korean Soc Radiol.
2011 Sep;65(3):257-265.
Radiation-Induced Pulmonary Injury after Cyberknife Radiosurgery for Lung Malignancy: CT Appearance
- Affiliations
-
- 1Department of Radiology, Konyang University College of Medicine, Daejeon, Korea. cyj126@paran.com
- 2Department of Radiation Oncology, Konyang University College of Medicine, Daejeon, Korea.
Abstract
- PURPOSE
To evaluate the CT appearance of radiation-induced pulmonary injury in patients who have undergone cyberknife radiosurgery for lung malignancy
MATERIALS AND METHODS
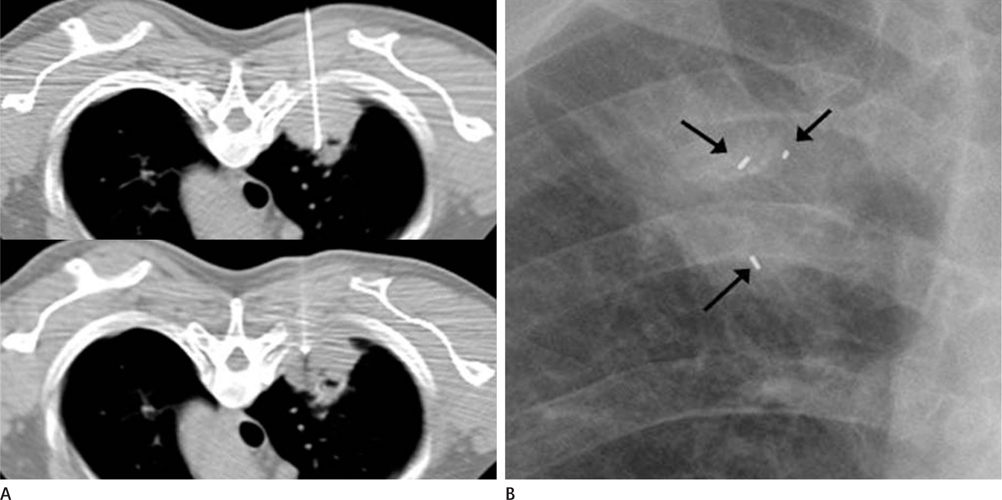
Thirty-four patients with 39 malignant lung tumors who underwent cyberknife radiosurgery were enrolled for evaluation. A total of 24-60 Gy was administered in 3 fractions. We evaluated the CT appearance of radiation pneumonitis and radiation fibrosis. We also evaluated the location of radiation pneumonitis and the minimal dose which causes radiation pneumonitis.
RESULTS
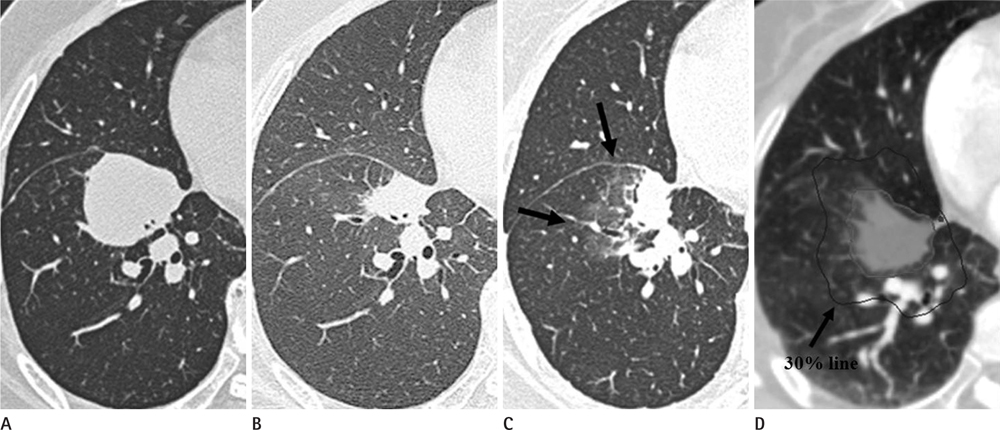
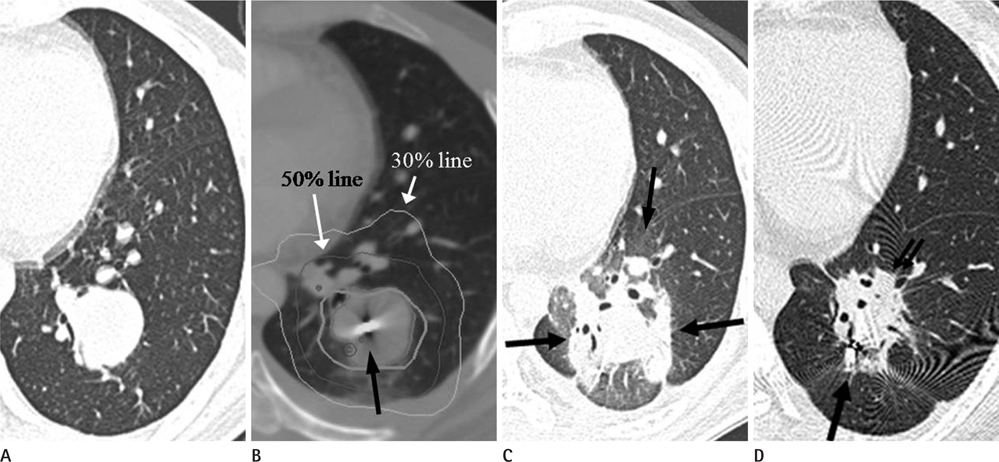
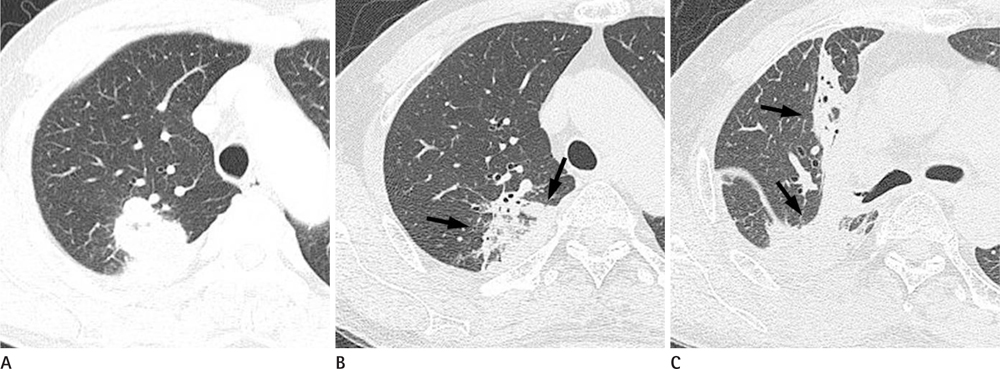
Radiation pneumonitis and radiation fibrosis occurred in 95% and 90% of cases, respectively. CT patterns of radiation pneumonitis demonstrated 20 cases (54%) as ground glass opacities (GGO). GGO included only 7 cases (19%), while 6 cases (16%) had patchy consolidations and 4 cases (11%) were diffuse consolidations, respectively. Radiation pneumonitis demonstrated 30 cases (81%) as concentric patterns surrounding the tumor, while 7 cases (19%) included the eccentric patterns. The radiation pneumonitis appeared within the 13-38 Gy (mean 21 Gy). CT findings of radiation fibrosis demonstrated as the modified conventional patterns, which decreased to 17 cases (65%), while 7 cases (27%) had mass-like patterns and 2 cases (8%) had scar-like patterns, respectively.
CONCLUSION
Radiation pneumonitis after cyberknife radiosurgery commonly develops as concentric patterns surrounding a tumor. The mass-like pattern of radiation fibrosis was sometimes difficult to distinguish from tumor recurrence. Thus, knowledge of the CT finding of radiation-induced lung injury might be helpful in distinguishing pulmonary changes from tumor recurrence.
Figure
Reference
-
1. Aoki T, Nagata Y, Negoro Y, Takayama K, Mizowaki T, Kokubo M, et al. Evaluation of lung injury after three-dimensional conformal stereotactic radiation therapy for solitary lung tumors: CT appearance. Radiology. 2004; 230:101–108.2. Bucci MK, Bevan A, Roach M 3rd. Advances in radiation therapy: conventional to 3D, to IMRT, to 4D, and beyond. CA Cancer J Clin. 2005; 55:117–134.3. Koenig TR, Munden RF, Erasmus JJ, Sabloff BS, Gladish GW, Komaki R, et al. Radiation injury of the lung after three-dimensional conformal radiation therapy. AJR Am J Roentgenol. 2002; 178:1383–1388.4. Park HJ, Kim KJ, Park SH, Kay CS, Oh JS. Early CT findings of tomotherapy-induced radiation pneumonitis after treatment of lung malignancy. AJR Am J Roentgenol. 2009; 193:W209–W213.5. Kim GJ, Shim SJ, Kim JH, Min CK, Chung WK. Evaluation of Real-time Measurement Liver Tumor's Movement and SynchronyTM System's Accuracy of Radiosurgery using a Robot CyberKnife. J Korean Soc Ther Radiol Oncol. 2008; 26:263–270.6. Chai GY, Lim YK, Kang KM, Jeong BG, Ha IB, Park KB, et al. Comparison of Three- and Four-dimensional Robotic Radiotherapy Treatment Plans for Lung Cancers. J Korean Soc Ther Radiol Oncol. 2010; 28:238–248.7. Sotiropoulou E, Stathochristopoulou I, Stathopoulos K, Verigos K, Salvaras N, Thanos L. CT-guided fiducial placement for cyberknife stereotactic radiosurgery: an initial experience. Cardiovasc Intervent Radiol. 2010; 33:586–589.8. Baba F, Shibamoto Y, Tomita N, Ikeya-Hashizume C, Oda K, Ayakawa S, et al. Stereotactic body radiotherapy for stage I lung cancer and small lung metastasis: evaluation of an immobilization system for suppression of respiratory tumor movement and preliminary results. Radiat Oncol. 2009; 4:15.9. van der Voort van Zyp NC, Prévost JB, Hoogeman MS, Praag J, van der Holt B, Levendag PC, et al. Stereotactic radiotherapy with real-time tumor tracking for non-small cell lung cancer: clinical outcome. Radiother Oncol. 2009; 91:296–300.10. Haasbeek CJ, Lagerwaard FJ, de Jaeger K, Slotman BJ, Senan S. Outcomes of stereotactic radiotherapy for a new clinical stage I lung cancer arising postpneumonectomy. Cancer. 2009; 115:587–594.11. Inoue T, Shimizu S, Onimaru R, Takeda A, Onishi H, Nagata Y, et al. Clinical outcomes of stereotactic body radiotherapy for small lung lesions clinically diagnosed as primary lung cancer on radiologic examination. Int J Radiat Oncol Biol Phys. 2009; 75:683–687.12. Uematsu M, Shioda A, Suda A, Fukui T, Ozeki Y, Hama Y, et al. Computed tomography-guided frameless stereotactic radiotherapy for stage I non-small cell lung cancer: a 5-year experience. Int J Radiat Oncol Biol Phys. 2001; 51:666–670.13. Brown WT, Wu X, Amendola B, Perman M, Han H, Fayad F, et al. Treatment of early non-small cell lung cancer, stage IA, by image-guided robotic stereotactic radioablation--CyberKnife. Cancer J. 2007; 13:87–94.14. Kimura T, Matsuura K, Murakami Y, Hashimoto Y, Kenjo M, Kaneyasu Y, et al. CT appearance of radiation injury of the lung and clinical symptoms after stereotactic body radiation therapy (SBRT) for lung cancers: are patients with pulmonary emphysema also candidates for SBRT for lung cancers? Int J Radiat Oncol Biol Phys. 2006; 66:483–491.15. Takeda T, Takeda A, Kunieda E, Ishizaka A, Takemasa K, Shimada K, et al. Radiation injury after hypofractionated stereotactic radiotherapy for peripheral small lung tumors: serial changes on CT. AJR Am J Roentgenol. 2004; 182:1123–1128.16. Collins BT, Vahdat S, Erickson K, Collins SP, Suy S, Yu X, et al. Radical cyberknife radiosurgery with tumor tracking: an effective treatment for inoperable small peripheral stage I non-small cell lung cancer. J Hematol Oncol. 2009; 2:1.17. Choi YW, Munden RF, Erasmus JJ, Park KJ, Chung WK, Jeon SC, et al. Effects of radiation therapy on the lung: radiologic appearances and differential diagnosis. Radiographics. 2004; 24:985–997. discussion 998.18. Movsas B, Raffin TA, Epstein AH, Link CJ Jr. Pulmonary radiation injury. Chest. 1997; 111:1061–1076.19. Abratt RP, Morgan GW. Lung toxicity following chest irradiation in patients with lung cancer. Lung Cancer. 2002; 35:103–109.20. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005; 235:208–215.21. Park KJ, Chung JY, Chun MS, Suh JH. Radiation-induced lung disease and the impact of radiation methods on imaging features. Radiographics. 2000; 20:83–98.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT findings of radiation-induced pulmonary injury
- A Case of Acute Injury in the Stomach and Duodenum after Cyberknife Therapy
- Clinical Results of Cyberknife(R) Radiosurgery for Spinal Metastases
- Cyberknife radiosurgery for inoperable recurred oral cancer
- Intravascular Placement of Metallic Coils as Lung Tumor Markers for CyberKnife Stereotactic Radiation Therapy