J Korean Soc Radiol.
2013 Dec;69(6):421-425.
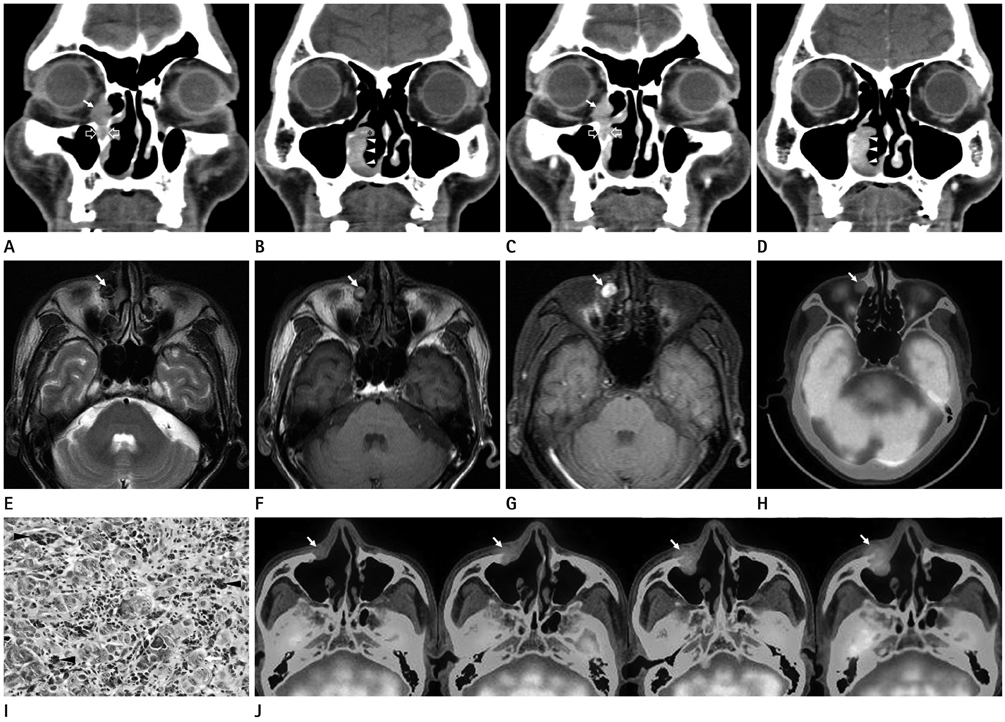
CT, MRI, and 18F-Fluorodeoxyglucose Positron Emission Tomography/CT Features of Primary Mucosal Melanoma Involving the Lacrimal Drainage Apparatus: A Case Report
- Affiliations
-
- 1Department of Radiology, Keimyung University School of Medicine, Daegu, Korea. sklee@dsmc.or.kr
- 2Department of Pathology, Keimyung University School of Medicine, Daegu, Korea.
Abstract
- We report CT, MRI, and initial and follow-up 18F-fluorodeoxyglucose positron emission tomography/CT (18F-FDG PET/CT) features of a case of primary mucosal melanoma of the lacrimal drainage apparatus in a 76-year-old man. The lesion was identified as an enhancing mass of the right lacrimal sac with extension into the inferior meatus through the nasolacrimal duct on CT. It was hyperintense and hypointense compared with gray matter on T1- and T2-weighted images, respectively, and intensely enhanced on gadolinium-enhanced T1-weighted images. Initial 18F-FDG PET/CT demonstrated mild fluorodeoxyglucose uptake of the mass. Surgical biopsy confirmed the diagnosis. Periodic follow-up 18F-FDG PET/CT demonstrated recurrent disease 18 months after surgery and its progression thereafter. In primary mucosal melanoma of the lacrimal drainage apparatus, CT, MRI, and initial and follow-up 18F-FDG PET/CT may be useful for early detection of the lesion and associated bony changes, lesion characterization, initial staging, and surveillance of recurrent and metastatic diseases, respectively.
MeSH Terms
Figure
Reference
-
1. Pujari A, Ali MJ, Mulay K, Naik MN, Honavar SG. The black lacrimal sac: a clinicopathological correlation of a malignant melanoma with anterior lacrimal crest infiltration. Int Ophthalmol. 2013; [Epub ahead of print].2. Sitole S, Zender CA, Ahmad AZ, Hammadeh R, Petruzzelli GJ. Lacrimal sac melanoma. Ophthal Plast Reconstr Surg. 2007; 23:417–419.3. Nam JH, Kim SM, Choi JH, Lee YK, Baek JH, Jang TJ, et al. Primary malignant melanoma of the lacrimal sac: a case report. Korean J Intern Med. 2006; 21:248–251.4. Billing K, Malhotra R, Selva D, Saloniklis S, Taylor J, Krishnan S. Magnetic resonance imaging findings in malignant melanoma of the lacrimal sac. Br J Ophthalmol. 2003; 87:1187–1188.5. Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998; 83:1664–1678.6. Lloyd WC 3rd, Leone CR Jr. Malignant melanoma of the lacrimal sac. Arch Ophthalmol. 1984; 102:104–107.7. Levine MR, Dinar Y, Davies R. Malignant melanoma of the lacrimal sac. Ophthalmic Surg Lasers. 1996; 27:318–320.8. Montalban A, Liétin B, Louvrier C, Russier M, Kemeny JL, Mom T, et al. Malignant lacrimal sac tumors. Eur Ann Otorhinolaryngol Head Neck Dis. 2010; 127:165–172.9. Kim SS, Han MH, Kim JE, Lee CH, Chung HW, Lee JS, et al. Malignant melanoma of the sinonasal cavity: explanation of magnetic resonance signal intensities with histopathologic characteristics. Am J Otolaryngol. 2000; 21:366–378.10. Haerle SK, Soyka MB, Fischer DR, Murer K, Strobel K, Huber GF, et al. The value of 18F-FDG-PET/CT imaging for sinonasal malignant melanoma. Eur Arch Otorhinolaryngol. 2012; 269:127–133.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT, Magnetic Resonance, and 18F-Fluorodeoxyglucose Positron Emission Tomography/CT Imaging Features of Mucosa-Associated Lymphoid Tissue Lymphoma Involving Medial Rectus Muscle: A Case Report
- Fluorodeoxyglucose Positron-Emission Tomography/Computed Tomography and Magnetic Resonance Imaging for Adverse Local Tissue Reactions near Metal Implants after Total Hip Arthroplasty: A Preliminary Report
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- Verification of the Dystonic Muscles Using 18F-Fluorodeoxyglucose Positron Emission Tomography in a Patient with Cervical Dystonia: A case report
- Effectiveness of 18F-fluoro-deoxyglucose Positron Emission Tomography/Computed Tomography and Magnetic Resonance Imaging to Detect Iliopsoas Tendonitis after Total Hip Arthroplasty: A Case Report