J Korean Soc Menopause.
2012 Apr;18(1):60-66.
Survey on the Prevalence of Overactive Bladder in Healthy Korean Postmenopausal Women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, College of Medicine, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- 2Department of Obstetrics and Gynecology, College of Medicine, Chung-Ang University, Seoul, Korea. cauob@hanmail.net
Abstract
OBJECTIVES
Overactive bladder (OAB) is characterized by urinary urgency, usually accompanied with frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection (UTI) or other obvious pathology. This study was performed to investigate the prevalence of OAB and the effect of hormone therapy (HT) on the OAB prevalence in healthy Korean postmenopausal women.
METHODS
The frequency, nocturia, urgency, and urgency incontinence were investigated by using questionnaire in 350 healthy postmenopausal women over 45 years old among patients who visited the Department of Obstetrics and Gynecology, Chung-Ang University Hospital, between November 2010 and February 2011.
RESULTS
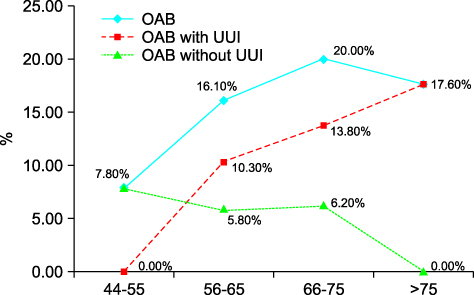
In our study, the prevalence of OAB was 14.3% and OAB with urgency incontinence was present in 8.0% of the investigated participants. There was no difference in OAB related to older age or the presence of HT, but signifi cant difference was found in the duration of menopause (odds ratio [OR] 3.451, 95% confidence interval [CI] 1.422-8.377, P = 0.004). Higher risks for both frequency (OR 2.921, 95% CI 1.587-5.375, P = 0.001) and nocturia (OR 2.469, 95% CI 1.069-5.702, P = 0.037) were observed in OAB subjects compared to postmenopausal women without OAB.
CONCLUSION
To the best of our knowledge, this is the fi rst study investigating the prevalence of overactive bladder in Korean postmenopausal women. Older age or HT did not affect the prevalence of OAB, and HT was not effective in treating the symptoms of OAB. However, the prevalence of OAB was increased with the age, duration of menopause.
Keyword
MeSH Terms
Figure
Reference
-
1. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010. 21:5–26.2. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.3. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003. 20:327–336.4. Homma Y, Yamaguchi O, Hayashi K. An epidemiological survey of overactive bladder symptoms in Japan. BJU Int. 2005. 96:1314–1318.5. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006. 50:1306–1314.6. de Boer TA, Slieker-ten Hove MC, Burger CW, Vierhout ME. The prevalence and risk factors of overactive bladder symptoms and its relation to pelvic organ prolapse symptoms in a general female population. Int Urogynecol J. 2011. 22:569–575.7. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011. 29:185–190.8. Komaroff AL, Fagioli LR, Doolittle TH, Gandek B, Gleit MA, Guerriero RT, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996. 101:281–290.9. Kelleher CJ, Reese PR, Pleil AM, Okano GJ. Health-related quality of life of patients receiving extended-release tolterodine for overactive bladder. Am J Manag Care. 2002. 8:S608–S615.10. Liberman JN, Hunt TL, Stewart WF, Wein A, Zhou Z, Herzog AR, et al. Health-related quality of life among adults with symptoms of overactive bladder: results from a U.S. community-based survey. Urology. 2001. 57:1044–1050.11. Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, Ensrud KE, et al. Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000. 48:721–725.12. Hashim H, Abrams P. Is the bladder a reliable witness for predicting detrusor overactivity? J Urol. 2006. 175:191–194.13. Brading AF. A myogenic basis for the overactive bladder. Urology. 1997. 50:57–67.14. de Groat WC. A neurologic basis for the overactive bladder. Urology. 1997. 50:36–52.15. Drake MJ, Mills IW, Gillespie JI. Model of peripheral autonomous modules and a myovesical plexus in normal and overactive bladder function. Lancet. 2001. 358:401–403.16. Zorn BH, Montgomery H, Pieper K, Gray M, Steers WD. Urinary incontinence and depression. J Urol. 1999. 162:82–84.17. Melville JL, Walker E, Katon W, Lentz G, Miller J, Fenner D. Prevalence of comorbid psychiatric illness and its impact on symptom perception, quality of life, and functional status in women with urinary incontinence. Am J Obstet Gynecol. 2002. 187:80–87.18. Lee KS, Na YG, Dean-McKinney T, Klausner AP, Tuttle JB, Steers WD. Alterations in voiding frequency and cystometry in the clomipramine induced model of endogenous depression and reversal with fluoxetine. J Urol. 2003. 170:2067–2071.19. Ouslander JG. Management of overactive bladder. N Engl J Med. 2004. 350:786–799.20. Temml C, Heidler S, Ponholzer A, Madersbacher S. Prevalence of the overactive bladder syndrome by applying the International Continence Society definition. Eur Urol. 2005. 48:622–627.21. Grady D, Brown JS, Vittinghoff E, Applegate W, Varner E, Snyder T. Postmenopausal hormones and incontinence: the Heart and Estrogen/Progestin Replacement Study. Obstet Gynecol. 2001. 97:116–120.22. Grodstein F, Lifford K, Resnick NM, Curhan GC. Postmenopausal hormone therapy and risk of developing urinary incontinence. Obstet Gynecol. 2004. 103:254–260.23. Hendrix SL, Cochrane BB, Nygaard IE, Handa VL, Barnabei VM, Iglesia C, et al. Effects of estrogen with and without progestin on urinary incontinence. JAMA. 2005. 293:935–948.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overactive Bladder and Urinary Incontinence in Adult Women: Prevalence and Effects on Daily Life and Sexual Activity
- Correlation analysis about effect of cardiovascular risk factors and disease in women on overactive bladder and stress urinary incontinence
- The Prevalence and Quality of Life of Overactive Bladder and Urinary Incontinence in Young Women
- Overactive Bladder
- Age Related Changes of Voiding Patterns in Women with Overactive Bladder