Tuberc Respir Dis.
2013 Dec;75(6):244-249.
Pleural Fluid Pentraxin-3 for the Differential Diagnosis of Pleural Effusions
- Affiliations
-
- 1Department of Internal Medicine, Uijeongbu St. Mary's Hospital, The Catholic University of Korea College of Medicine, Uijeongbu, Korea.
- 2Department of Internal Medicine, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. cmcksj@catholic.ac.kr
- 3Department of Internal Medicine, St. Paul's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Yeouido St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 5Department of Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 6Department of Biostatistics, Clinical Research Coordinating Center, The Catholic University of Korea, Seoul, Korea.
- 7Division of Cancer Prevention and Control, Moffitt Cancer Center, Tampa, FL, USA.
Abstract
- BACKGROUND
Conventional biomarkers cannot always establish the cause of pleural effusions; thus, alternative tests permitting rapid and accurate diagnosis are required. The primary aim of this study is to assess the ability of pentraxin-3 (PTX3) in order to diagnose the cause of pleural effusion and compare its efficacy to that of other previously identified biomarkers.
METHODS
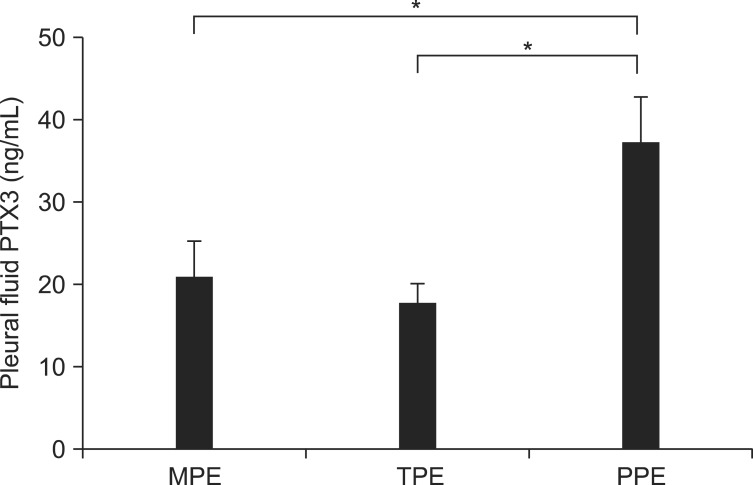
We studied 118 patients with pleural effusion, classified as transudates and exudates including malignant, tuberculous, and parapneumonic effusions (MPE, TPE, and PPE). The levels of PTX3, C-reactive protein (CRP), procalcitonin (PCT) and lactate in the pleural fluid were assessed.
RESULTS
The levels of pleural fluid PTX3 were significantly higher in patients with PPE than in those with MPE or TPE. PTX3 yielded the most favorable discriminating ability to predict PPE from MPE or TPE by providing the following: area under the curve, 0.74 (95% confidence interval, 0.63-0.84), sensitivity, 62.07%; and specificity, 81.08% with a cut-off point of 25.00 ng/mL.
CONCLUSION
Our data suggests that PTX3 may allow improved differentiation of PPE from MPE or TPE compared to the previously identified biomarkers CRP and PCT.
Keyword
MeSH Terms
Figure
Reference
-
1. Marel M, Zrustova M, Stasny B, Light RW. The incidence of pleural effusion in a well-defined region: epidemiologic study in central Bohemia. Chest. 1993; 104:1486–1489. PMID: 8222812.2. Daniil ZD, Zintzaras E, Kiropoulos T, Papaioannou AI, Koutsokera A, Kastanis A, et al. Discrimination of exudative pleural effusions based on multiple biological parameters. Eur Respir J. 2007; 30:957–964. PMID: 17690119.
Article3. Light RW. Clinical practice: pleural effusion. N Engl J Med. 2002; 346:1971–1977. PMID: 12075059.4. Hooper C, Lee YC, Maskell N. BTS Pleural Guideline Group. Investigation of a unilateral pleural effusion in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65(Suppl 2):ii4–ii17. PMID: 20696692.
Article5. Yilmaz Turay U, Yildirim Z, Turkoz Y, Biber C, Erdogan Y, Keyf AI, et al. Use of pleural fluid C-reactive protein in diagnosis of pleural effusions. Respir Med. 2000; 94:432–435. PMID: 10868705.6. Kiropoulos TS, Kostikas K, Oikonomidi S, Tsilioni I, Nikoulis D, Germenis A, et al. Acute phase markers for the differentiation of infectious and malignant pleural effusions. Respir Med. 2007; 101:910–918. PMID: 17270413.
Article7. Lin MC, Chen YC, Wu JT, Ko YC, Wang CC. Diagnostic and prognostic values of pleural fluid procalcitonin in parapneumonic pleural effusions. Chest. 2009; 136:205–211. PMID: 19255287.
Article8. Porcel JM, Vives M, Cao G, Bielsa S, Ruiz-Gonzalez A, Martinez-Iribarren A, et al. Biomarkers of infection for the differential diagnosis of pleural effusions. Eur Respir J. 2009; 34:1383–1389. PMID: 19541708.
Article9. Peri G, Introna M, Corradi D, Iacuitti G, Signorini S, Avanzini F, et al. PTX3, a prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation. 2000; 102:636–641. PMID: 10931803.
Article10. He X, Han B, Liu M. Long pentraxin 3 in pulmonary infection and acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2007; 292:L1039–L1049. PMID: 17277044.
Article11. Garlanda C, Hirsch E, Bozza S, Salustri A, De Acetis M, Nota R, et al. Non-redundant role of the long pentraxin PTX3 in antifungal innate immune response. Nature. 2002; 420:182–186. PMID: 12432394.
Article12. Ozsu S, Abul Y, Mentese A, Bektas H, Uzun A, Ozlu T, et al. Pentraxin-3: a novel biomarker for discriminating parapneumonic from other exudative effusions. Respirology. 2013; 18:657–662. PMID: 23286371.
Article13. Papageorgiou E, Kostikas K, Kiropoulos T, Karetsi E, Mpatavanis G, Gourgoulianis KI. Increased oxidative stress in exudative pleural effusions: a new marker for the differentiation between exudates and transudates? Chest. 2005; 128:3291–3297. PMID: 16304274.14. Light RW, Macgregor MI, Luchsinger PC, Ball WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972; 77:507–513. PMID: 4642731.
Article15. Garlanda C, Bottazzi B, Bastone A, Mantovani A. Pentraxins at the crossroads between innate immunity, inflammation, matrix deposition, and female fertility. Annu Rev Immunol. 2005; 23:337–366. PMID: 15771574.
Article16. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999; 340:448–454. PMID: 9971870.
Article17. Mauri T, Coppadoro A, Bellani G, Bombino M, Patroniti N, Peri G, et al. Pentraxin 3 in acute respiratory distress syndrome: an early marker of severity. Crit Care Med. 2008; 36:2302–2308. PMID: 18596636.
Article18. He X, Han B, Bai X, Zhang Y, Cypel M, Mura M, et al. PTX3 as a potential biomarker of acute lung injury: supporting evidence from animal experimentation. Intensive Care Med. 2010; 36:356–364. PMID: 19921147.
Article19. Porcel JM, Bielsa S, Esquerda A, Ruiz-Gonzalez A, Falguera M. Pleural fluid C-reactive protein contributes to the diagnosis and assessment of severity of parapneumonic effusions. Eur J Intern Med. 2012; 23:447–450. PMID: 22726374.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pleural fluid to serum cholinesterase ratio for the differential diagnosis of transudates and exsudates
- Diagnostic Tools of Pleural Effusion
- TNF-alpha in the Pleural Fluid for the Differential Diagnosis of Tuberculous and Malignant Effusion
- Comparison of Characteristics of Pleural Fluid and Blood in Mycoplasmal and Tuberculous Pleural Effusions
- A study on lactic dehydrogenase activity of tuberculous pleural effusion