Tuberc Respir Dis.
2013 Oct;75(4):165-169.
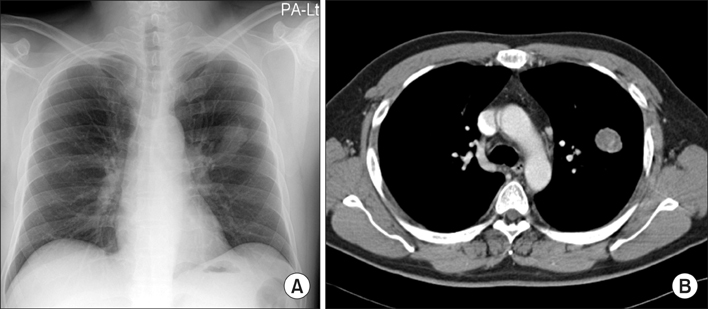
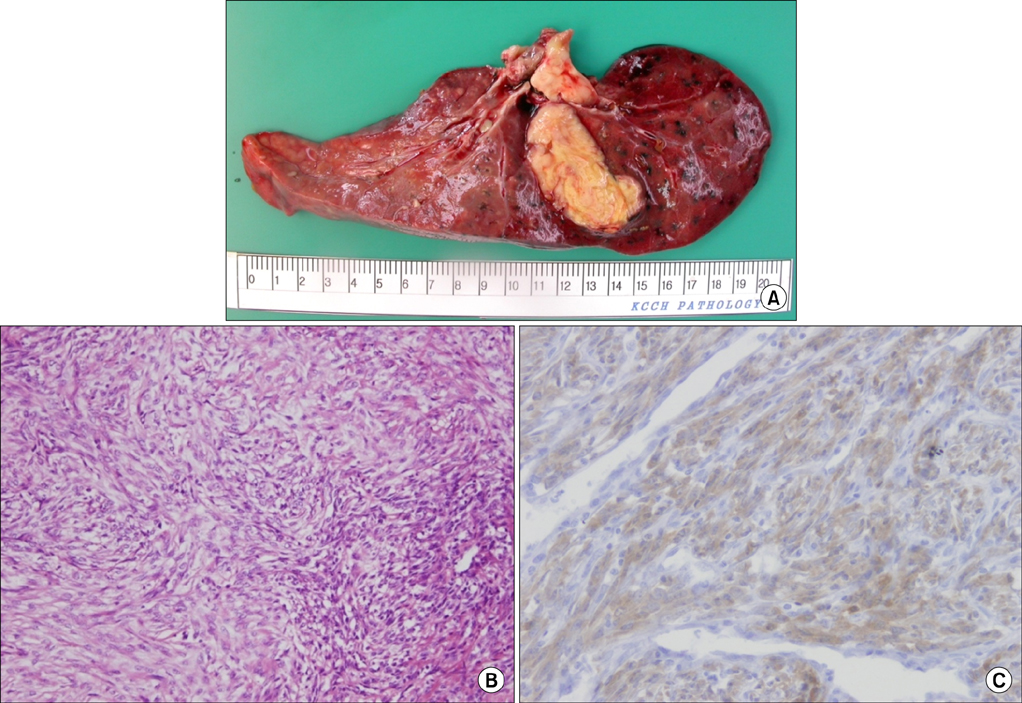
A Case of Recurrent Pulmonary Inflammatory Myofibroblastic Tumor with Aggressive Metastasis after Complete Resection
- Affiliations
-
- 1Department of Internal Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea. cheol@kcch.re.kr
Abstract
- An inflammatory myofibroblastic tumor (IMT) is a rare disease entity reported to arise in various organs. It is thought to be a neoplastic or reactive inflammatory condition, controversially. The treatment of choice for myofibroblastic tumor is surgery, and recurrence is known to be rare. The optimal treatment method is not well-known for patients ineligible for surgery. We report a 47-year-old patient with aggressive recurrent IMT of the lungs. The patient had been admitted for an evaluation of back-pain two years after a complete resection of pulmonary IMT. Radiation therapy was performed for multiple bone recurrences, and the symptoms were improved. However the patient presented again with aggravated back-pain six months later. High-dose steroid and non-steroidal anti-inflammatory drugs were administered, but the disease progressed aggressively, resulting in spinal cord compression and metastasis to intra-abdominal organs. This is a very rare case of aggressively recurrent pulmonary IMT with multi-organ metastasis.
Keyword
MeSH Terms
Figure
Reference
-
1. Cerfolio RJ, Allen MS, Nascimento AG, Deschamps C, Trastek VF, Miller DL, et al. Inflammatory pseudotumors of the lung. Ann Thorac Surg. 1999; 67:933–936.2. Hagenstad CT, Kilpatrick SE, Pettenati MJ, Savage PD. Inflammatory myofibroblastic tumor with bone marrow involvement: a case report and review of the literature. Arch Pathol Lab Med. 2003; 127:865–867.3. Kim DY, Park HS, Kim SM, Park JH, Hong YS, Lee JL, et al. Inflammatory myofibroblastic tumor showing durable remission after anthracycline-containing cytotoxic chemotherapy: report of a case. Korean J Med. 2012; 82:749–753.4. Sasagawa Y, Akai T, Itou S, Iizuka H. Multiple intraosseous inflammatory myofibroblastic tumors presenting with an aggressive clinical course: case report. Neurosurgery. 2011; 69:E1010–E1015.5. Brunn H. Two interesting benign lung tumors of contradictory histopathology. J Thorac Surg. 1939; 9:119–131.6. Coffin CM, Fletcher JA. Fletcher CD, Unni KK, Mertens F, editors. World Health Organization classification of tumours: pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press;2002. p. 91–93.7. Coffin CM, Patel A, Perkins S, Elenitoba-Johnson KS, Perlman E, Griffin CA. ALK1 and p80 expression and chromosomal rearrangements involving 2p23 in inflammatory myofibroblastic tumor. Mod Pathol. 2001; 14:569–576.8. Suetsugu S, Yamamoto H, Izumi M, Takayama K, Inoue H, Nakanishi Y. A case of rapidly growing inflammatory myofibroblastic tumor in the lung. Nihon Kokyuki Gakkai Zasshi. 2009; 47:1156–1160.9. Kubo N, Harada T, Anai S, Otsubo K, Yoneshima Y, Ijichi K, et al. Carboplatin plus paclitaxel in the successful treatment of advanced inflammatory myofibroblastic tumor. Intern Med. 2012; 51:2399–2401.10. Applebaum H, Kieran MW, Cripe TP, Coffin CM, Collins MH, Kaipainen A, et al. The rationale for nonsteroidal antiinflammatory drug therapy for inflammatory myofibroblastic tumors: a Children's Oncology Group study. J Pediatr Surg. 2005; 40:999–1003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of the Lung in a Child: A case report
- A Case of Inflammatory Myofibroblastic Tumor of Nasal Cavity in an 8 Year-Old Girl
- Adult Intussusception Caused by Inflammatory Myofibroblastic Tumor of the Jejunum
- Inflammatory Myofibroblastic Tumor (InflammatoryFibrosarcoma) of the Lung: A Case Report