Tuberc Respir Dis.
2012 Jan;72(1):50-54.
A Case of Hereditary Hemorrhagic Telangiectasia Diagnosed through Spontaneous Hemothorax
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. sanghakim@yonsei.ac.kr
- 2Department of Thoracic Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Radiology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 4Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
Abstract
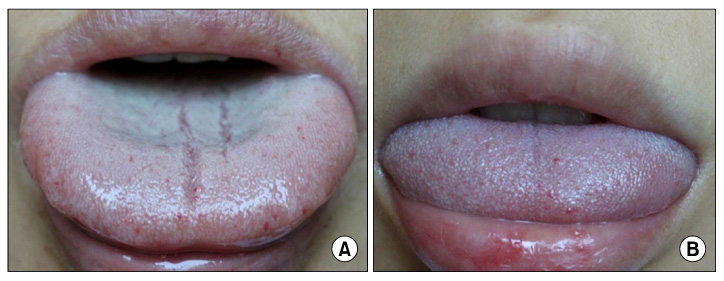
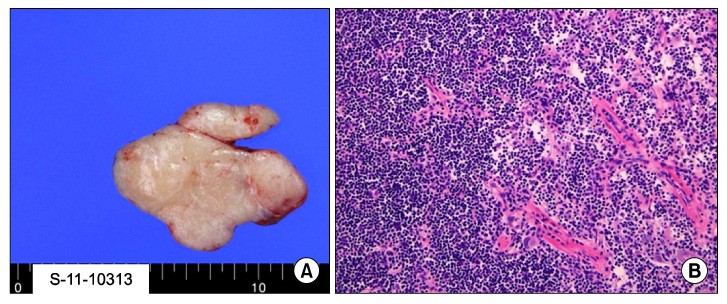
- Hereditary hemorrhagic telangiectasia (HHT, Osler-Weber-Rendu disease) is a rare autosomal dominant disease characterized by heterogenous multisystemic dysplasia of the vascular tissue. Prevalence of HHT is 1 in 5,000~8,000. HHT commonly presents with recurrent epistaxis, but may have more serious consequences if visceral vascular beds are involved. Approximately 30~50% of HHT cases also present with pulmonary arteriovenous malformation (PAVM). Spontaneous hemothorax is less common, and PAVM is one of the causes leading to hemothorax. Our case involved an 18-year-old female who had suddenly developed right chest pain. The reason for chest pain was due to right spontaneous hemothorax accompanied by PAVM in the right middle lobe. The patient was additionally diagnosed with HHT upon examination of her family history, specifically through her mother's symptom that included recurrent epistaxis and mucosal telangiectasia.
MeSH Terms
Figure
Reference
-
1. Ali HA, Lippmann M, Mundathaje U, Khaleeq G. Spontaneous hemothorax: a comprehensive review. Chest. 2008. 134:1056–1065.2. Shovlin CL, Jackson JE. Mason RJ, Broaddus VC, Martin TR, King TE, Schraufnagel DE, Murray JF, Nadel JA, editors. Pulmonary arteriovenous malformations and other vascular abnormalities. Murray & Nadel's textbook of respiratory medicine. 2010. 5th ed. Philadelphia: Saunders;1262–1265.3. Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000. 91:66–67.4. Ishikawa T, Pollak S, Pflugradt R, Bohnert M, Grosse Perdekamp M, Thierauf A, et al. Pulmonary arteriovenous malformation causing sudden death due to spontaneous hemothorax. Int J Legal Med. 2010. 124:459–465.5. Sabbà C, Pasculli G, Lenato GM, Suppressa P, Lastella P, Memeo M, et al. Hereditary hemorrhagic telangiectasia: clinical features in ENG and ALK1 mutation carriers. J Thromb Haemost. 2007. 5:1149–1157.6. Cottin V, Dupuis-Girod S, Lesca G, Cordier JF. Pulmonary vascular manifestations of hereditary hemorrhagic telangiectasia (rendu-osler disease). Respiration. 2007. 74:361–378.7. Ference BA, Shannon TM, White RI Jr, Zawin M, Burdge CM. Life-threatening pulmonary hemorrhage with pulmonary arteriovenous malformations and hereditary hemorrhagic telangiectasia. Chest. 1994. 106:1387–1390.8. Cottin V, Chinet T, Lavolé A, Corre R, Marchand E, Reynaud-Gaubert M, et al. Pulmonary arteriovenous malformations in hereditary hemorrhagic telangiectasia: a series of 126 patients. Medicine (Baltimore). 2007. 86:1–17.9. Pollak JS, Saluja S, Thabet A, Henderson KJ, Denbow N, White RI Jr. Clinical and anatomic outcomes after embolotherapy of pulmonary arteriovenous malformations. J Vasc Interv Radiol. 2006. 17:35–44.10. Kim M, Song HY, Choi JK, Jeong H, Park IN, Choi SB, et al. A familial case of hereditary hemorrhagic telangiectasia. Tuberc Respir Dis. 2009. 66:314–318.11. Bevelaqua FA, Ordorica SA, Lefleur R, Young B. Osler-Weber-Rendu disease. Diagnosis and management of spontaneous hemothorax during pregnancy. N Y State J Med. 1992. 92:551–552.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hereditary Hemorrhagic Telangiectasia in a Family
- Hereditary Hemorrhagic Telangiectasia Combined with Pulmonary Arteriovenous Malformation Treated with Transcatheter Embolotherapy
- A Case of Hereditary Hemorrhagic Telangiectasia
- A Case of Hereditary Hemorrhagic Telangiectasia Combined with Pulmonary- Systemic Fistula
- A Case of Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia Presenting as High Output Heart Failure