Tuberc Respir Dis.
2011 Apr;70(4):342-346.
Coexistence of Hodgkin's Lymphoma and Tuberculosis in the Same Axillary Lymph Nodes
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. mdlee@catholic.ac.kr
- 2Department of Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
Abstract
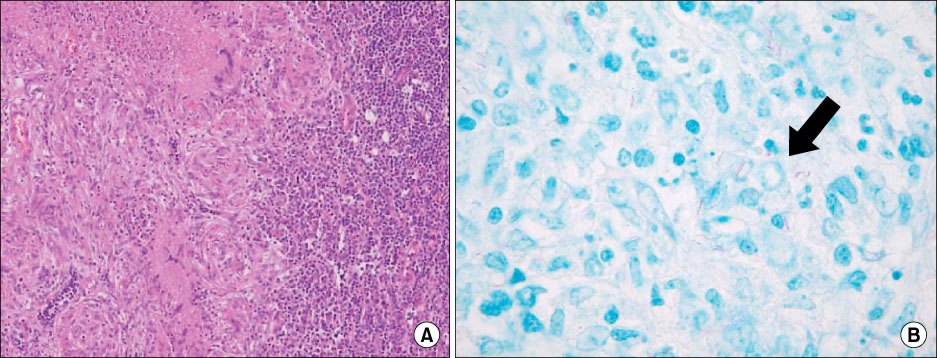
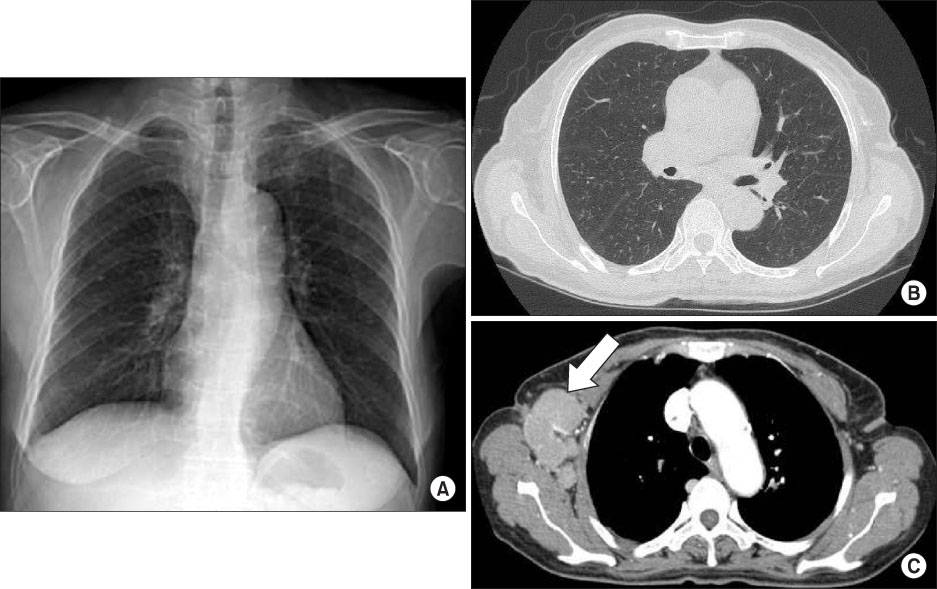
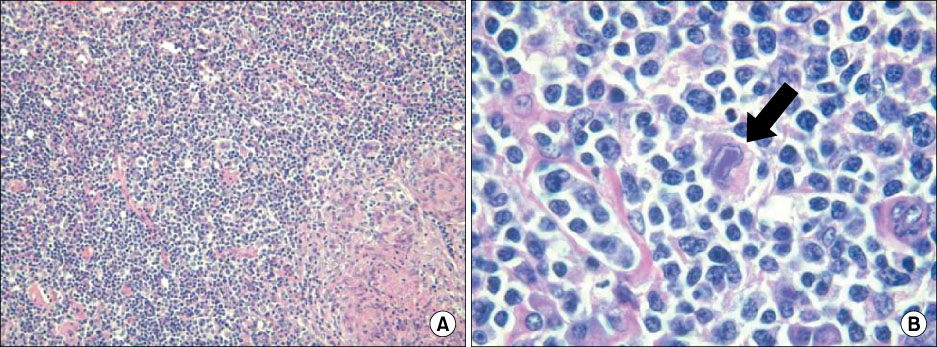
- Herein we report the case of a 71-year-old woman who complained of fatigue and enlarged right axillary lymph nodes for 18 months. At her first visit, her chest X-ray showed diffuse nodular opacities in both lung fields. Initial excisional biopsy of the axillary lymph nodes showed granulomatous lesions and acid fast bacilli were seen on Ziehl-Neelsen staining. However, even after 15 months of anti-tuberculosis (TB) medication, her right axillary lymph nodes were enlarged. We re-performed an excisional biopsy of the nodes, which showed Hodgkin's lymphoma (HL). A retrograde review of the biopsy before anti-tuberculous medication, revealed HL coexisting with TB. HL and TB cause difficulties in differential diagnosis due to similarities in clinical course, imaging procedures and histopathological analysis of the involved tissue. Therefore, it is important to consider the possibility of concurrent HL and TB when patients who undergo treatment for TB or chemotherapy for lymphoma complain of persistent systemic symptoms or enlarged lymph nodes.
Keyword
MeSH Terms
Figure
Reference
-
1. Poppema S. Immunobiology and pathophysiology of Hodgkin lymphomas. Hematology Am Soc Hematol Educ Program. 2005. 231–238.2. Centkowski P, Sawczuk-Chabin J, Prochorec M, Warzocha K. Hodgkin's lymphoma and tuberculosis coexistence in cervical lymph nodes. Leuk Lymphoma. 2005. 46:471–475.3. Karakas Z, Agaoglu L, Taravari B, Saribeyoglu E, Somer A, Guler N, et al. Pulmonary tuberculosis in children with Hodgkin's lymphoma. Hematol J. 2003. 4:78–81.4. Lee SS, Koh JS, Park S, Kim MS, Cho SY, Chung SY, et al. Cytomorphologic comparison of Hodgkin lymphoma and anaplastic large cell lymphoma in fine needle aspiration cytology. Korean J Cytopathol. 2006. 17:126–135.5. Johnson LN, Iseri O, Knodell RG. Caseating hepatic granulomas in Hodgkin's lymphoma. Gastroenterology. 1990. 99:1837–1840.6. Plank L, Adamkov M. Syncytial variant of the nodular sclerosing type of Hodgkin's disease in cervical lymph nodes with simultaneous sarcoidosis-like granulomatosis in the intrathoracic lymph nodes and liver. Zentralbl Pathol. 1992. 138:292–297.7. Urba WJ, Longo DL. Hodgkin's disease. N Engl J Med. 1992. 326:678–687.8. Mohapatra PR, Janmeja AK. Tuberculous lymphadenitis. J Assoc Physicians India. 2009. 57:585–590.9. Yang ZG, Min PQ, Sone S, He ZY, Liao ZY, Zhou XP, et al. Tuberculosis versus lymphomas in the abdominal lymph nodes: evaluation with contrast-enhanced CT. AJR Am J Roentgenol. 1999. 172:619–623.10. Rüdiger T, Jaffe ES, Delsol G, deWolf-Peeters C, Gascoyne RD, Georgii A, et al. Workshop report on Hodgkin's disease and related diseases ('grey zone' lymphoma). Ann Oncol. 1998. 9:Suppl 5. S31–S38.11. Lee AJ, Kim SG, Jeon CH, Suh HS, Yoon GS, Seo AN. A case of natural killer cell leukemia misdiagnosed as tuberculous lymphadenopathy. Korean J Lab Med. 2009. 29:194–198.