Tuberc Respir Dis.
2011 Jan;70(1):10-20.
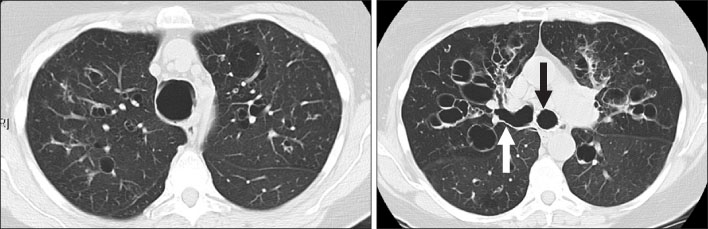
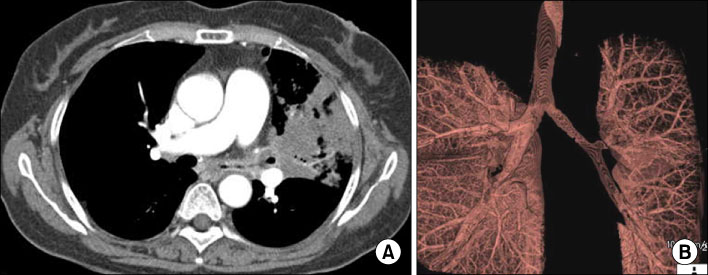
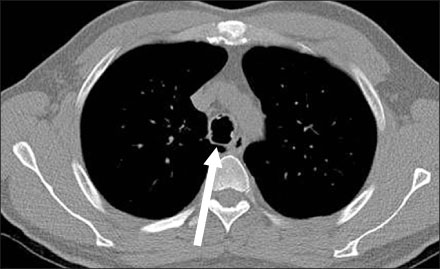
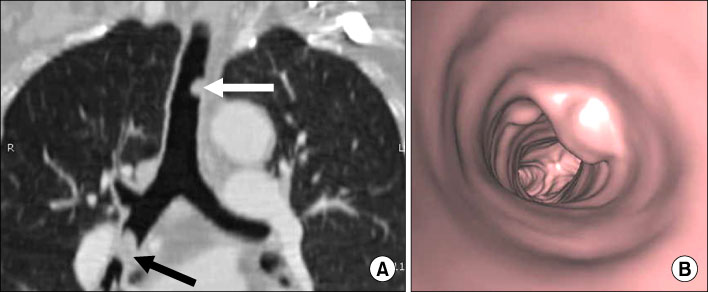
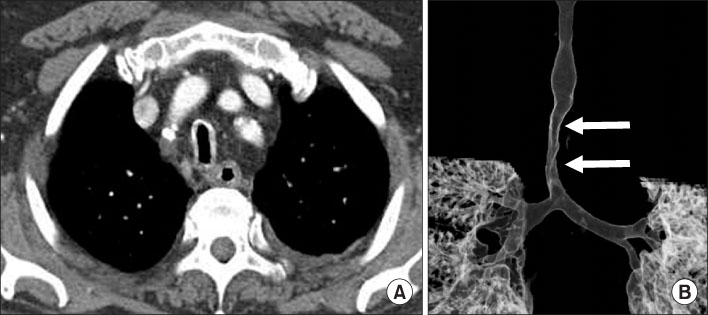
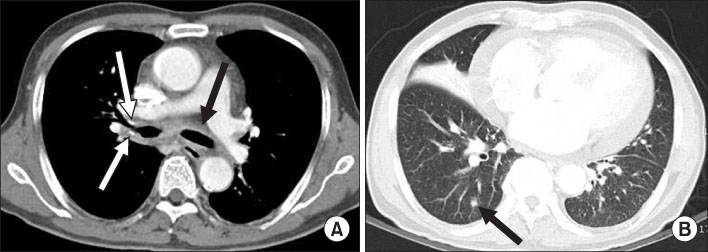
Pictorial Review of Diffuse Central Airway Diseases: Focus on CT Findings
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. jhhwang@schmc.ac.kr
Abstract
- Various diseases can diffusely involve central airways, including the trachea and main stem bronchi. Central airway abnormalities are frequently not apparent or are overlooked on chest radiographs, even though the patient may have significant symptoms. Recent advances in spiral and multi-detector computed tomography (CT) with multi-planar reconstruction and three-dimensional demonstration, including virtual bronchoscopy, allow for excellent display of central airway anatomy and abnormalities with visualization of accurate locations of lesions. Early detection and proper diagnosis of airway diseases based on various radiographic findings will help determine appropriate treatment, including surgical planning and evaluation of treatment response. Herein we describe and illustrate the imaging findings of a wide spectra of diffuse central airway diseases.
MeSH Terms
Figure
Reference
-
1. Kwong JS, Müller NL, Miller RR. Diseases of the trachea and main-stem bronchi: correlation of CT with pathologic findings. Radiographics. 1992. 12:645–657.2. Marom EM, Goodman PC, McAdams HP. Diffuse abnormalities of the trachea and main bronchi. AJR Am J Roentgenol. 2001. 176:713–717.3. Hansell DM, Armstrong P, Lynch DA, McAdams HP, editors. Chapter 12. Airway disease. Imaging of diseases of the chest. 2005. 4th ed. Philadelphia: Elsevier Mosby;711–783.4. Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2005. 25:789–801.5. Boiselle PM, Ernst A. Tracheal morphology in patients with tracheomalacia: prevalence of inspiratory lunate and expiratory "frown" shapes. J Thorac Imaging. 2006. 21:190–196.6. Prince JS, Duhamel DR, Levin DL, Harrell JH, Friedman PJ. Nonneoplastic lesions of the tracheobronchial wall: radiologic findings with bronchoscopic correlation. Radiographics. 2002. 22:S215–S230.7. Marom EM, Goodman PC, McAdams HP. Focal abnormalities of the trachea and main bronchi. AJR Am J Roentgenol. 2001. 176:707–711.8. Spizarny DL, Shepard JA, McLoud TC, Grillo HC, Dedrick CG. CT of adenoid cystic carcinoma of the trachea. AJR Am J Roentgenol. 1986. 146:1129–1132.9. Park HJ, Park SH, Im SA, Kim YK, Lee KY. CT differentiation of anthracofibrosis from endobronchial tuberculosis. AJR Am J Roentgenol. 2008. 191:247–251.10. Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR. Fibrosing mediastinitis. Radiographics. 2001. 21:737–757.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Findings of Central Airway Lesions Causing Airway Stenosis-Visualization and Quantification: A Pictorial Essay
- Neurological Complications Following Liver Transplant: A Pictorial Review of Radiological and Clinical Findings
- Multi-Detector Row CT of the Central Airway Disease
- Imaging Findings of Coronary Artery Fistula in Children: A Pictorial Review
- Non-Neoplastic Disorders of the Esophagus