Tuberc Respir Dis.
2009 Sep;67(3):229-233.
A Case of Pulmonary Sparganosis in a Patient with a History of Recurrent Sparganum Infections
- Affiliations
-
- 1Department of Internal Medicine, Bundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea. dhkim@dmc.or.kr
- 2Department of Thoracic Surgery, Bundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea.
- 3Department of Pathology, Bundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea.
Abstract
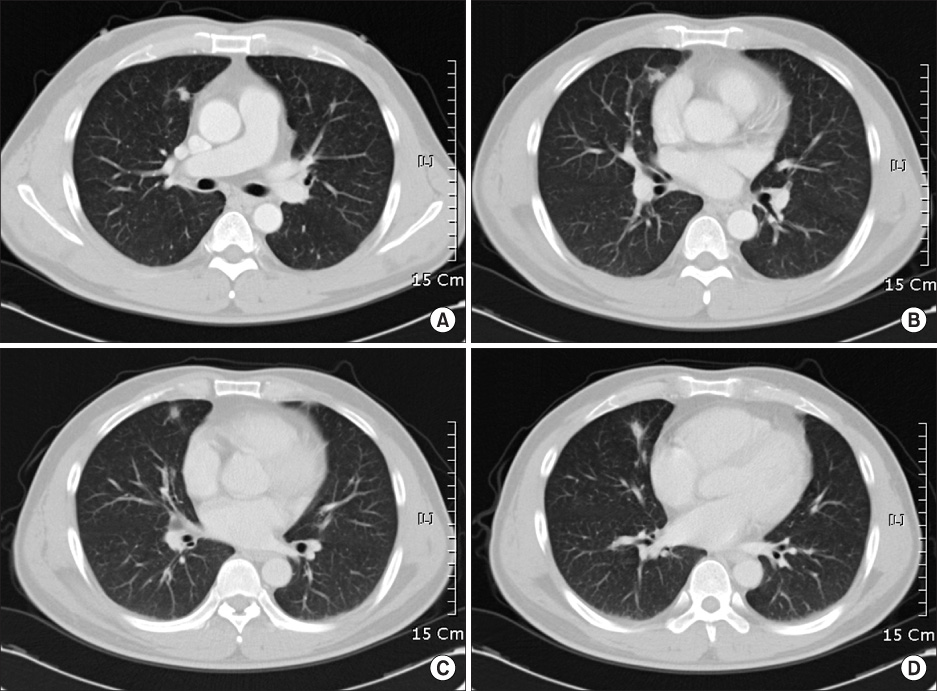
- Sparganosis is a zoonosis caused by the migrating larvae of cestode genus Spirometra. We report a rare form of sparganosis that invades the lung. A 44-year-old man presented with newly appeared pulmonary nodules that were found accidentally on regular medical checkup, and on sequential chest CT, which we checked at an interval of every 2 months, revealed that the pulmonary lesion had migrated. The patient had a medical history of having undergone surgical excisions for sparganosis in muscles and in subcutaneous tissues of the lower abdomen, perianus, thigh, right axilla, and scapula area, several times over 7 years. A right middle lobectomy was performed and the lesion was diagnosed as sparganosis based on the characteristic histological findings.
Keyword
MeSH Terms
Figure
Reference
-
1. Mueller JF. The biology of Spirometra. J Parasitol. 1974. 60:3–14.2. Cho SY, Bae JH, Seo BS. Some aspects of human sparganosis in Korea. Korean J Parasitol. 1975. 13:60–77.3. Lee BJ, Ahn SK, Kim SC, Lee SH. Clinical and histopathologic study of Sparganosis. Korean J Dermatol. 1992. 30:168–174.4. Mougeot G, Cambon M, Menerath JM, Dimeglio V, Houin R. Human eye anterior chamber sparganosis. Parasite. 1999. 6:365–367.5. Jeong SC, Bae JC, Hwang SH, Kim HC, Lee BC. Cerebral sparganosis with intracerebral hemorrhage: a case report. Neurology. 1998. 50:503–506.6. Lo YK, Chao D, Yan SH, Liu HC, Chu FL, Huang CI, et al. Spinal cord proliferative sparganosis in Taiwan: a case report. Neurosurgery. 1987. 21:235–238.7. Phunmanee A, Boonsawat W, Indharapoka B, Tuntisirin C, Kularbkeaw J. Pulmonary sparganosis: a case report with five years follow-up. J Med Assoc Thai. 2001. 84:130–135.8. Iwatani K, Kubota I, Hirotsu Y, Wakimoto J, Yoshioka M, Mori T, et al. Sparganum mansoni parasitic infection in the lung showing a nodule. Pathol Int. 2006. 56:674–677.9. Hur J, Lee SC, Lee CY. Pulmonary sparganosis: a case report. Korean J Thorac Cardiovasc Surg. 2003. 36:43–46.10. Beaver DC, Jung RC, Cupp EW. Clinical parasitology. 1984. 9th ed. Philadephia: Lea & Febriger.11. Cho BK, Chun CS, Choi WY, Cho SY. A case of unusual sparganosis. Korean J Dermatol. 1985. 23:672–677.12. Brown HW, Neva FA. Basic clinical parasitology. 1983. 5th ed. Norwalk: Appleton-Century-Crofts.13. Chi JG, Chi HS, Lee SH. Histopathologic study on human sparganosis. Korean J Parasitol. 1980. 18:15–23.14. Wang KC, Huh S, Hong ST, Chai JY, Choi KS, Lee SH. The fate of spargana inoculated into the cat brain and sequential changes of anti-sparganum IgG antibody levels in the cerebrospinal fluid. Korean J Parasitol. 1990. 28:1–10.15. Chai JY, Yu JR, Lee SH, Kim SI, Cho SY. Ineffectiveness of praziquantel treatment for human sparganosis (a case report). Seoul J Med. 1988. 29:397–399.