Tuberc Respir Dis.
2008 Feb;64(2):153-157.
A Case of Different Response of Miliary Lung and Intracranial Nodules to Antituberculous Therapy
- Affiliations
-
- 1Department of Internal Medicine, Korea Cancer Center Hospital, Seoul, Korea. jclee@kcch.re.kr
Abstract
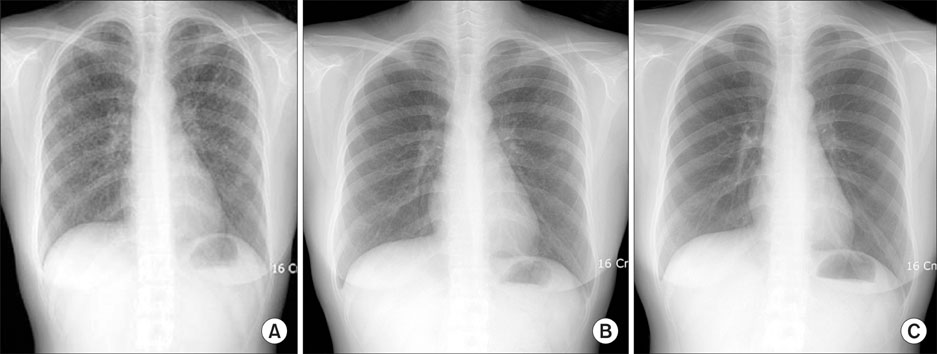
- Although a paradoxical response of tuberculosis to antituberculous therapy is not a rare phenomenon, it can be a clinical challenge to differentiate a paradoxical response from treatment failure. A 25-year-old woman was admitted for miliary lung nodules and multiple intracranial nodules. Antituberculous treatment was started with a preliminary diagnosis of tuberculosis based on the history and clinical findings. After one month, the miliary lung nodules improved while the intracranial nodules increased in size and number. Based on a stereotactic biopsy, it was confirmed that the intracranial lesions were tuberculomas. Although the therapeutic regimen was not changed, the symptoms eventually were ameliorated and the intracranial nodules improved two months later.
MeSH Terms
Figure
Reference
-
1. Cheng VC, Ho PL, Lee RA, Chan KS, Chan KK, Woo PC, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002. 21:803–809.2. Minn Y. 10 cases of paradoxical expansion of intracranial tuberculomas during chemotherapy. Tuberc Respir Dis. 2001. 51:260–264.3. Kang HD, Jun CS, Lee KY, Han JH, Lee HS, Choi J, et al. Miliary tuberculosis and multiple intracranial tuberculoma. Korean J Pediatr Infect Dis. 2001. 44:443–450.4. Jain SK, Kwon P, Moss WJ. Management and outcomes of intracranial tuberculomas developing during anti-tuberculous therapy. Clin Pediatr (Phila). 2005. 44:443–450.5. Afghani B, Lieberman JM. Paradoxical enlargement or development of intracranial tuberculomas during therapy: case report and review. Clin Infect Dis. 1994. 19:1092–1099.6. Ford AL, Foulcher E, Lemckert FA, Sedgwick JD. Microglia induce CD4 T lymphocyte final effector function and death. J Exp Med. 1996. 184:1737–1745.7. Matyszak MK, Perry VH. Bacillus Calmette-Guerin sequestered in the brain parenchyma escapes immune recognition. J Neuroimmunol. 1998. 82:73–80.8. Garcia de Viedma D, Marin M, Ruiz Serrano MJ, Alcala L, Bouza E. Polyclonal and compartmentalized infection by Mycobacterium tuberculosis in patients with both respiratory and extrarespiratory involvement. J Infect Dis. 2003. 187:695–699.9. Thrush DC, Barwick DD. Three patients with intracranial tuberculomas with unusual features. J Neurol Neurosurg Psychiatry. 1974. 37:566–569.10. Bouchama A, al-Kawi MZ, Kanaan I, Coates R, Jallu A, Rahm B, et al. Brain biopsy in tuberculoma: the risks and benefits. Neurosurgery. 1991. 28:405–409.11. Chambers ST, Hendrickse WA, Record C, Rudge P, Smith H. Paradoxical expansion of intracranial tuberculomas during chemotherapy. Lancet. 1984. 2:181–184.12. Teoh R, Humphries MJ, O'Mahony G. Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: a report of 10 patients and review of the literature. Q J Med. 1987. 63:449–460.13. Arseni C. Two hundred and one cases of intracranial tuberculoma treated surgically. J Neurol Neurosurg Psychiatry. 1958. 21:308–311.14. American Thoracic Society. Centers for Disease Control and Prevention and the Infectious Diseases Society. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.15. Lees AJ, MacLeod AF, Marshall J. Cerebral tuberculoma developing during treatment of tuberculous meningitis. Lancet. 1980. 1:1208–1211.16. Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical response to tuberculostatic chemotherapy. Infection. 1997. 25:233–239.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 10 Cases of Paradoxical Expansion of Intracranial Terculomas During Chemotherapy
- Paradoxical Response to Chemotherapy in Tuberculous Pleural Effusion
- Miliary Tuberculosis and Multiple Intracranial Tuberculoma : A Case Report
- Diffuse Large B-Cell Lymphoma Manifesting as Miliary Nodules in the Lung: A Case Report
- A Case of Complete Treatment of Multiple Intracranial Tuberculoma