Tuberc Respir Dis.
2006 Aug;61(2):101-108.
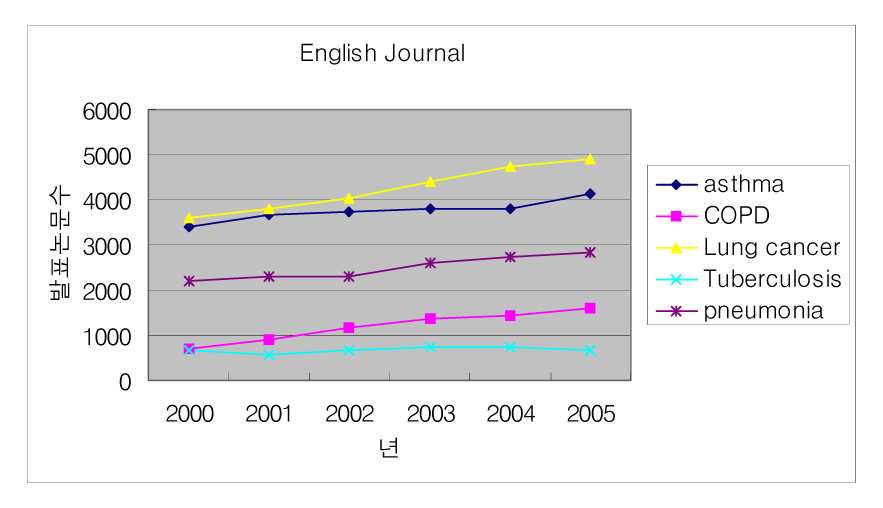
Clinical Year Review of COPD
- Affiliations
-
- 1Division of Pulmonary-Allergology, Department of Internal Medicine Yeungnam University College of Medicine, Daegu, Republic of Korea. ghlee@med.yu.ac.kr
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
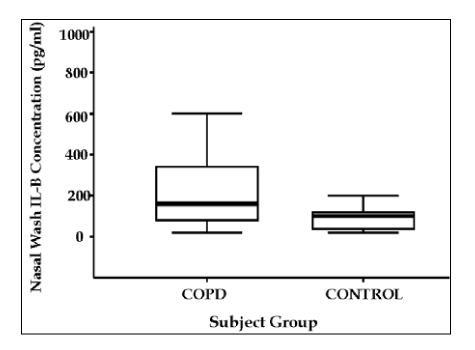
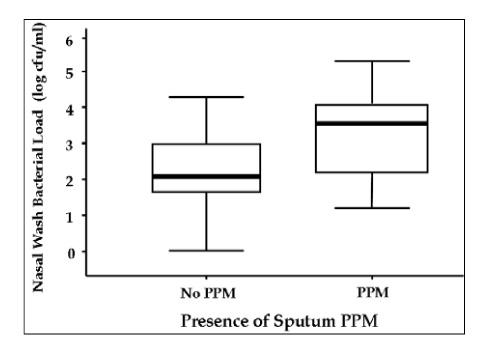
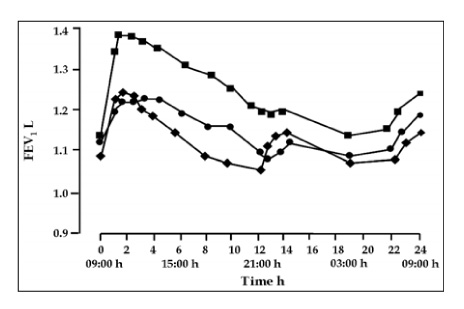
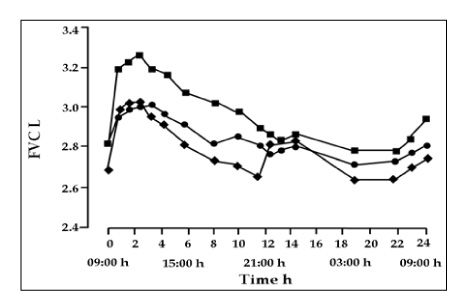
1. Hurst JR, Wilkinson TM, Perera WR, Donaldson GC, Wedzicha JA. Relationships among bacteria, upper airway, lower airway, and systemic inflammation in COPD. Chest. 2005. 127:1219–1226.2. Hurst JR, Perera WR, Wilkinson TM, Donaldson GC, Wedzicha JA. Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006. 173:71–78.3. Donaldson GC, Seemungal TA, Patel IS, Bhowmik A, Wilkinson TM, Hurst JR, et al. Airway and systemic inflammation and decline in lung function in patients With COPD. Chest. 2005. 128:1995–2004.4. Mahler DA, Huang S, Tabrizi M, Bell GM. Efficacy and safety of a monoclonal antibody recognizing interleukin-8 in COPD. Chest. 2004. 126:926–934.5. Wouters EF. Local and systemic inflammation in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:26–33.6. Buffels J, Degryse J, Heyrman J, Decramer M. Office spirometry significantly improves early detection of COPD in general practice. Chest. 2004. 125:1394–1399.7. Dales RE, Vandemheen KL, Clinch J, Aaron SD. Spirometry in the primary care setting: influence on clinical diagnosis and management of airflow obstruction. Chest. 2005. 128:2443–2447.8. Zielinski J, Bednarek M. Early detection in a high-risk population using spirometric screenig. Chest. 2001. 119:731–736.9. Bolton CE, Ionescu AA, Edwards PH, Faulkner TA, Edwards SM, Shale DJ. Attaining a correct diagnosis of COPD in general practice. Respir Med. 2005. 99:493–500.10. O'Donnell DE, Flűge T, Gerken F, Hamilton A, Webb K, Aguilaniu B, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respoir J. 2004. 23:832–840.11. Verkindre C, Bart F, Aguilaniu B, Fortin F, Guérin JC, le Merre C, et al. The effect of tiotropium on hyperinflation and exercise capacity in chronic obstructive pulmonary disease. Respiration. 2006. 73:420–427.12. Maltais F, Hamilton A, Marciniuk D, Hernandez P, Sciurba FC, Richter K, et al. Improvements in symptom-limited exercise performance over 8 h with once-daily tiotropium in patients with COPD. Chest. 2005. 128:1168–1178.13. van Noord JA, Aumann JL, Janssens E, Smeets JJ, Verhaert J, Disse B, et al. Comparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPD. Eur Respir J. 2005. 26:214–222.14. van Noord JA, Aumann JL, Janssens E, Vehaert J, Smeets JJ, Mueller A, et al. Effects of tiotropium with and without formoterol on airflow obstruction and resting hyperinflation in patients with COPD. Chest. 2006. 129:509–517.15. Wilkinson TM, Donaldson GC, Hurst JR, Seemungal TA, Wedzicha JA. Early therapy improves outcomes of exacervations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004. 169:1298–1303.16. Parker CM, Voduc N, Aaron SD, Webb KA, O'Donnell DE. Physiological changes during symptom recovery from moderate exacerbations of COPD. Eur Respir J. 2005. 26:420–428.17. Stevenson NJ, Walker PP, Costello RW, Calverley PM. Lung mechanics and dyspnea during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005. 172:1510–1516.18. Niewoehner DE, Rice K, Cote C, Paulson D, Cooper JA Jr, Korducki L, et al. Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator. Ann Intern Med. 2005. 143:317–326.19. Dusser D, Bravo ML, Iacono P. The effect of tiotropium on exacerbations and airflow in patients with COPD. Eur Respir J. 2006. 27:547–555.20. Celli BR. Chronic obstructive pulmonary disease from unjustified nihilism to evidence-based optimism. Proc Am Thorac Soc. 2006. 3:58–65.21. Buist S. COPD: a common disease that is preventable and treatable. Prim Care Rsepir J. 2006. 15:7–9.22. Anzueto A, Tashkin D, Menjoge S, Kesten S. One-year analysis of longitudinal changes in spirometry in patients with COPD receiving tiotropium. Pulm Pharmacol Ther. 2005. 18:75–81.23. Barnes PJ, Stockley RA. COPD: current therapeutic interventions and future approaches. Eur Respir J. 2005. 25:1084–1106.24. Wilson R. Treatment of COPD exacerbations: antibiotics. Eur Respir Rev. 2005. 14:32–38.25. Beading C, Slifka MK. How do viral infections predispose patients to bacterial infections? Curr Opin Infect Dis. 2004. 17:185–191.26. Wikinson TM, Hurst JR, Perera WR, Wilks M, Donaldson GC, Wedzicha JA. Effect of interactions between lower airway bacterial and rhinoviral infection in exacerbations of COPD. Chest. 2006. 129:317–324.27. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987. 106:196–204.28. van der Valk P, Monninkhof E, van der Palen J, Zielhuis G, van Herwaarden C, Hendrix R. Clinical predictors of bacterial involvement in exacerbations of chronic obstructive pulmonary disease. Clin Infect Dis. 2004. 39:980–986.29. Rosell A, Monsó E, Soler N, Torres F, Angrill J, Riise G, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005. 165:891–897.30. Wilson R. Treatment of COPD exacerbations: antibiotics. Eur Respir Rev. 2005. 14:32–38.31. Sethi S. Bacteria in exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2004. 1:109–114.32. Wilson R, Schentag JJ, Ball P, Mandell L. A comparison of gemifloxacin and clrithromycin in acute exacerbations of chronic bronchitis and lung-term clinical outcomes. Clin Ther. 2002. 24:639–652.33. Wilson R, Allegra L, Huchon G, Izquierdo JL, Jones P, Schaberg T, et al. Short-term and long-term outcomes of moxifloxcin compared to standard antibiotic treatment in acute exacerbations of chronic bronchitis. Chest. 2004. 125:953–964.34. Martinez FJ, Anzueto A. Appropriate outpatient treatment of acute bacterial exacerbation of chronic bronchitis. Am J Med. 2005. 118:Suppl 7A. 39S–44S.35. Casanova C, Cote C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, et al. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005. 171:591–597.36. Celli BR, Cote CG, Marin J, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004. 350:1005–1012.37. Ong KC, Earnest A, Lu SJ. A multidimensional grading system (BODE Index) as predictor of hospitalization for COPD. Chest. 2005. 128:3810–3816.38. Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J. 2005. 26:630–636.
- Full Text Links
- Actions
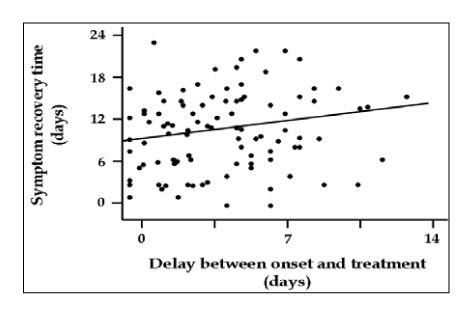
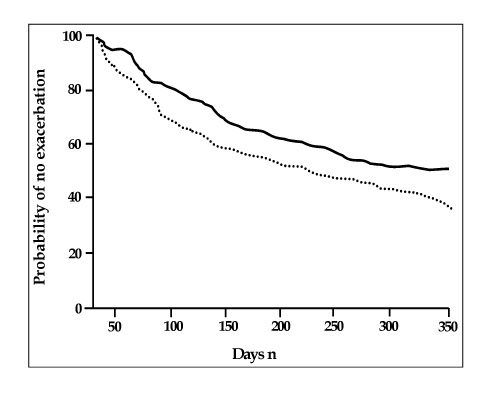
-
Cited
- CITED
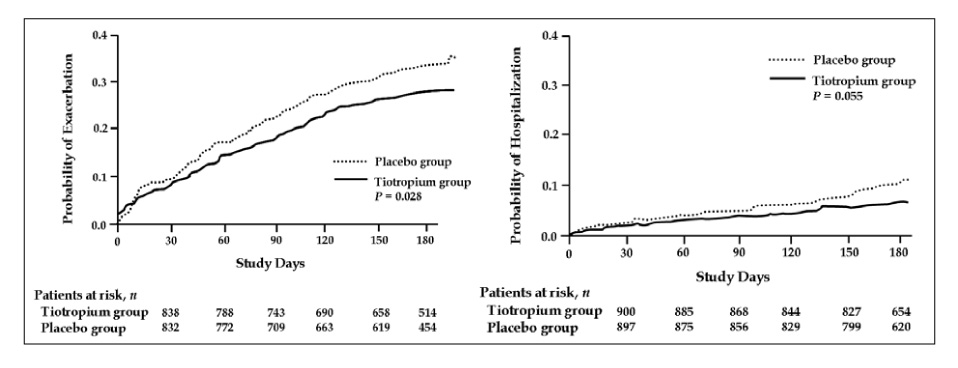
-
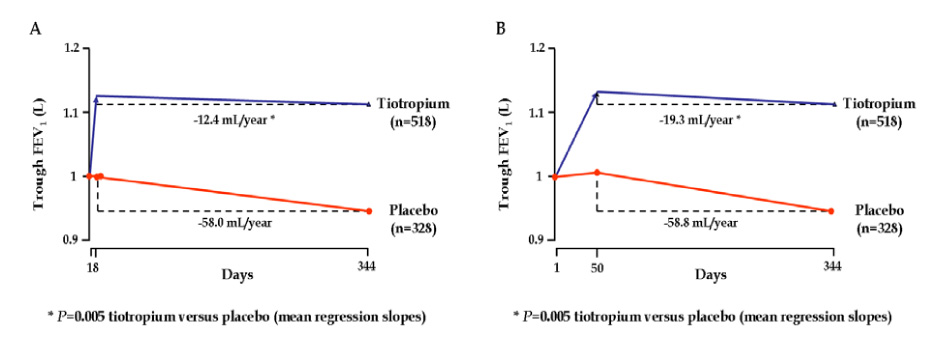
- Close
- Share
- Similar articles
-
- Clinical Year-in-Review of Chronic Obstructive Pulmonary Disease in Korea
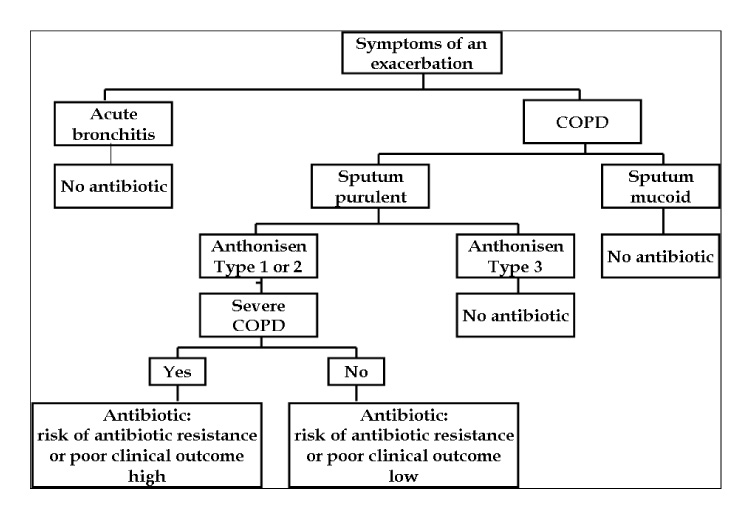
- Chronic Obstructive Pulmonary Disease: Respiratory Review of 2013
- Evaluation of Appropriate Management of Chronic Obstructive Pulmonary Disease in Korea: Based on Health Insurance Review and Assessment Service (HIRA) Claims
- Phenotype of Chronic Obstructive Pulmonary Disease Based on Computed Tomography–Defined Underlying Pathology
- Pathophysiology, clinical manifestation, and treatment of tuberculosis-associated chronic obstructive pulmonary disease: a narrative review