J Korean Ophthalmol Soc.
2016 Jul;57(7):1144-1149. 10.3341/jkos.2016.57.7.1144.
A Case of Primary Orbital Peripheral T-cell Lymphoma with Panniculitis-like Features
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yswoph@hanmail.net
- KMID: 2317577
- DOI: http://doi.org/10.3341/jkos.2016.57.7.1144
Abstract
- PURPOSE
To report a case of complete remission of primary orbital peripheral T-cell lymphoma with panniculitis-like features after chemotherapy.
CASE SUMMARY
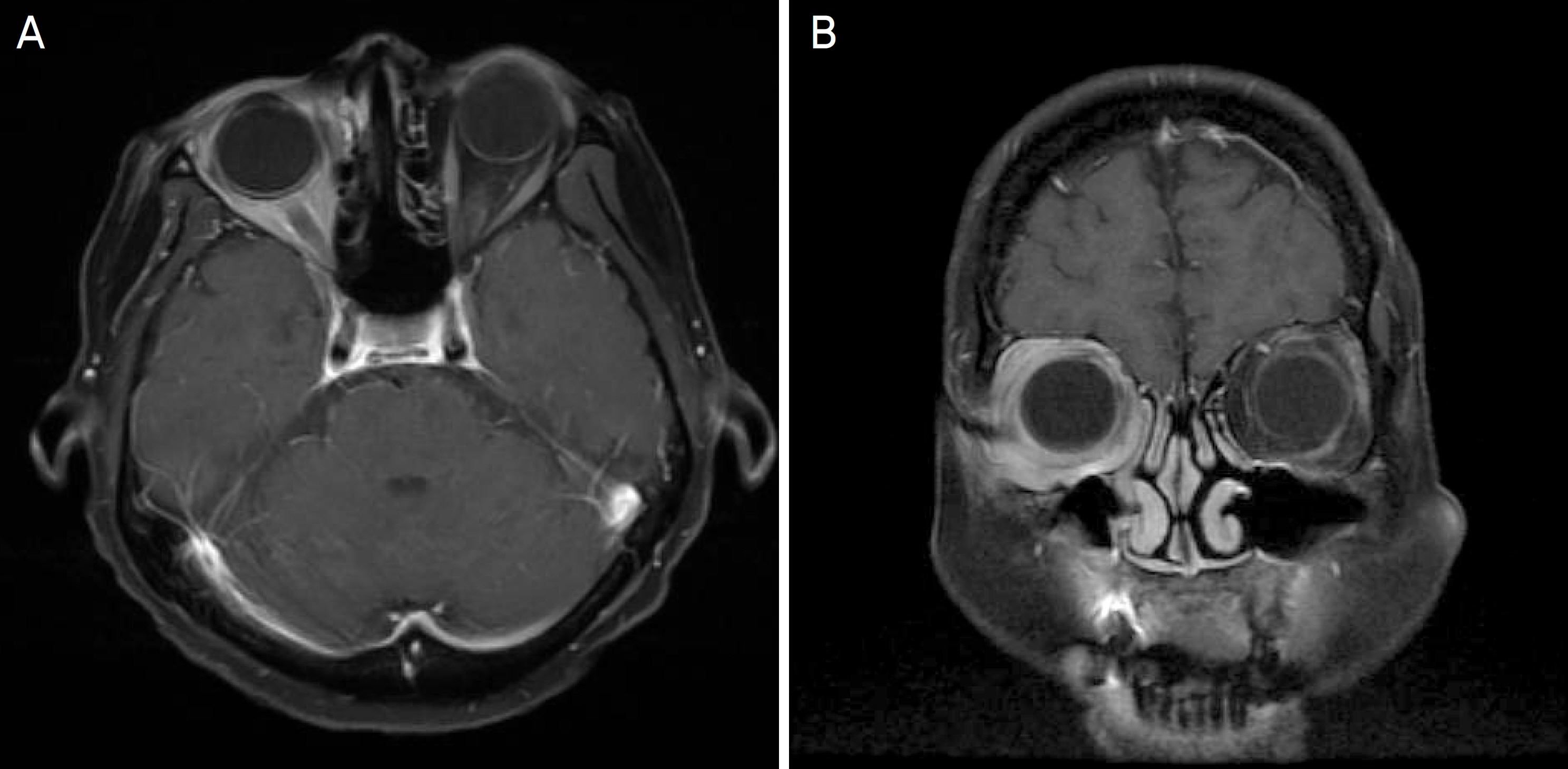
A 57-year-old healthy female presented with periorbital swelling and symptoms of diplopia. The patient was first treated with high-dose systemic corticosteroids, however, symptoms persisted. Therefore, anterior orbitotomy with excisional biopsy was performed for diagnostic purposes. On microscopic examination, the excised mass showed localized dense lymphocyte infiltrates, and cytologic atypia was observed under a high-power field. On immunehistochemical examination, tumor cells were positive for CD3 and CD8 but negative for CD4, CD20 and CD56. Based on histopathological results, primary orbital peripheral T-cell lymphoma with panniculitis-like features was diagnosed. Additionally, molecular pathological testing was positive for Epstein-Barr virus. Subsequently, the patients underwent chemotherapy and complete remission was obtained.
CONCLUSIONS
Peripheral T-cell lymphoma often manifests as systemic symptoms, including lymph node enlargement and B symptom. The primary form of the disease in an orbit is very rare, and has a poor prognosis with a high mortality rate because the disease quickly progresses. Herein, the authors report a rare case of a healthy patient without any past medical history who achieved complete remission of a fast-growing primary orbital T-cell lymphoma with no preceding systemic symptoms.
MeSH Terms
Figure
Reference
-
References
1. Amit S, Purwar N, Agarwal A, Kanchan S. Primary orbital non-Hod-gkin's lymphoma. BMJ Case Rep. 2012; 2012:pii: bcr2012006847.
Article2. Lee DS, Woo KI, Chang HR. T-cell lymphoma presenting as abdominal ophthalmoplegia. Korean J Ophthalmol. 2006; 20:192–4.3. Fitzpatrick PJ, Macko S. Lymphoreticular tumors of the orbit. Int J Radiat Oncol Biol Phys. 1984; 10:333–40.
Article4. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of abdominal lymphomas. Cancer. 1972; 29:252–60.5. Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica. 2010; 102:83–7.6. Vose J, Armitage J, Weisenburger D; International T-Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008; 26:4124–30.7. Cho EY, Han JJ, Ree HJ, et al. Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone b-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol. 2003; 73:87–96.
Article8. Janatpour KA, Choo PH, Lloyd WC 3rd. Primary orbital peripheral T-cell lymphoma: histologic, immunophenotypic, and genotypic features. Arch Ophthalmol. 2007; 125:1289–92.
Article9. Ferry JA, Fung CY, Zukerberg L, et al. Lymphoma of the ocular abdominal: a study of 353 cases. Am J Surg Pathol. 2007; 31:170–84.10. Hatef E, Roberts D, McLaughlin P, et al. Prevalence and nature of systemic involvement and stage at initial examination in patients with orbital and ocular adnexal lymphoma. Arch Ophthalmol. 2007; 125:1663–7.
Article11. Shields CL, Shields JA, Eagle RC. Clinicopathologic reports, case reports, and small case series: rapidly progressive T-cell abdominal of the conjunctiva. Arch Ophthalmol. 2002; 120:508–9.12. Okano M, Osato T, Koizumi S, et al. Epstein-Barr virus infection and oncogenesis in primary immunodeficiency. AIDS Res. 1986; 2(Suppl 1):S115–9.13. Stein H, Foss HD, Dürkop H, et al. CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features. Blood. 2000; 96:3681–95.14. Zhou XG, Hamilton-Dutoit SJ, Yan QH, Pallesen G. High abdominal of Epstein-Barr virus in Chinese peripheral T-cell lymphoma. Histopathology. 1994; 24:115–22.15. Dupuis J, Emile JF, Mounier N, et al. Prognostic significance of Epstein-Barr virus in nodal peripheral T-cell lymphoma, abdominal: a Groupe d'Etude des Lymphomes de l'Adulte (GELA) study. Blood. 2006; 108:4163–9.16. Cheng AL, Su IJ, Tien HF, et al. Characteristic clinicopathologic features of adult B-cell lymphoblastic lymphoma with special abdominal on differential diagnosis with an atypical form probably of blastic lymphocytic lymphoma of intermediate differentiation origin. Cancer. 1994; 73:706–10.17. Su IJ, Hsieh HC, Lin KH, et al. Aggressive peripheral T-cell abdominals containing Epstein-Barr viral DNA: a clinicopathologic and molecular analysis. Blood. 1991; 77:799–808.18. Gallamini A, Stelitano C, Calvi R, et al. Peripheral T-cell abdominal unspecified (PTCL-U): a new prognostic model from a abdominal multicentric clinical study. Blood. 2004; 103:2474–9.19. Kim K, Kim WS, Jung CW, et al. Clinical features of peripheral T-cell lymphomas in 78 patients diagnosed according to the Revised European-American lymphoma (REAL) classification. Eur J Cancer. 2002; 38:75–81.
Article20. Jagasia M, Morgan D, Goodman S, et al. Histology impacts the outcome of peripheral T-cell lymphomas after high dose abdominal and stem cell transplant. Leuk Lymphoma. 2004; 45:2261–7.21. Rodriguez J, Caballero MD, Gutierrez A, et al. High dose abdominal and autologous stem cell transplantation in patients with peripheral T-cell lymphoma not achieving complete response after induction chemotherapy. The GEL-TAMO experience. abdominal. 2003; 88:1372–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Findings of Subcutaneous Panniculitis-like T-Cell Lymphoma: A Case Report
- CT and (18F)FDG PET/CT Findings of Subcutaneous Panniculitis like T-Cell Lymphoma: A Case Report
- A Case of Atypical Lymphocytic Lobular Panniculitis
- Two Cases of Subcutaneous Panniculitis-like T-cell Lymphoma
- A Case of Eosinophilic Panniculitis Accompanied with Nodal Diffuse Large B-cell Lymphoma