Korean J Urol.
2013 Oct;54(10):703-709.
Impact of Surgical Varicocele Repair on Pregnancy Rate in Subfertile Men With Clinical Varicocele and Impaired Semen Quality: A Meta-Analysis of Randomized Clinical Trials
- Affiliations
-
- 1Department of Urology, Severance Hospital, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. kscho99@yuhs.ac
- 2Department of Urology, National Forensic Hospital, Ministry of Justice, Gongju, Korea.
- 3Division of Epidemic Intelligence Service, Korea Centers for Disease Control and Prevention, Cheongwon, Korea.
- 4Department of Urology, Cheil General Hospital & Women's Healthcare Center, Kwandong University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
To elucidate the impact of surgical varicocele repair on the pregnancy rate through new meta-analyses of randomized clinical trials that compared surgical varicocele repair and observation.
MATERIALS AND METHODS
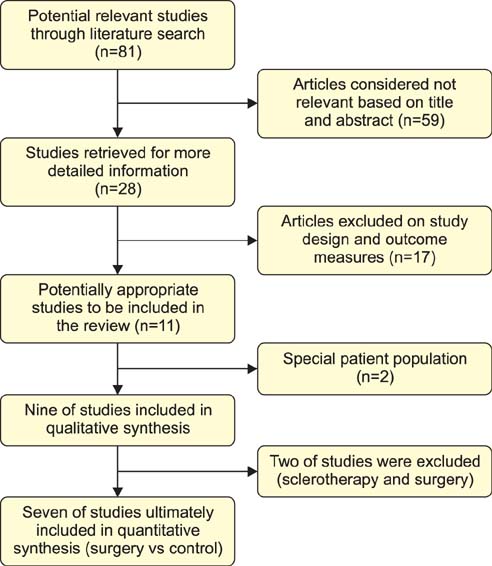
The PubMed and Embase online databases were searched for studies released before December 2012. References were manually reviewed, and two researchers independently extracted the data. To assess the quality of the studies, the Cochrane risk of bias as a quality assessment tool for randomized controlled trials was applied.
RESULTS
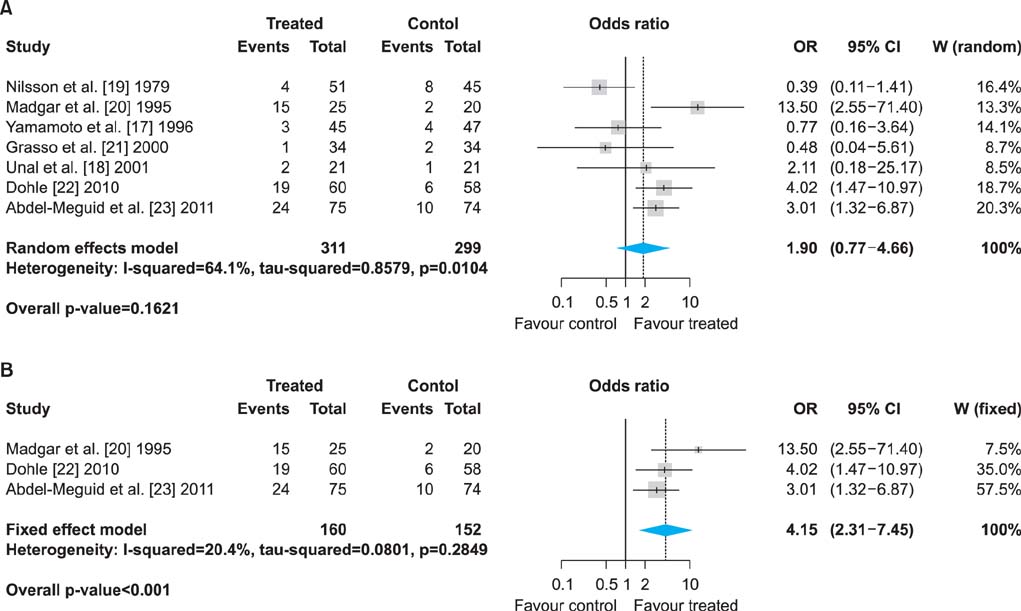
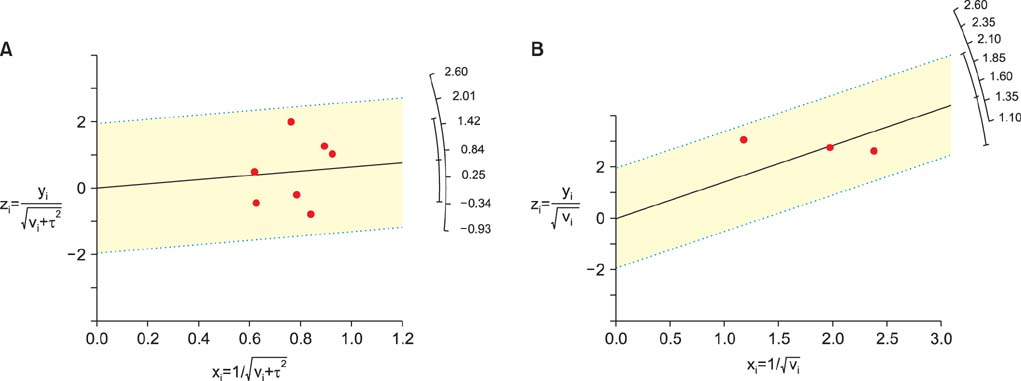
Seven randomized clinical trials were included in our meta-analyses, all of which compared pregnancy outcomes between surgical varicocele repair and control. There were differences in enrollment criteria among the studies. Four studies included patients with clinical varicocele, but three studies enrolled patients with subclinical varicocele. Meanwhile, four trials enrolled patients with impaired semen quality only, but the other three trials did not. In a meta-analysis of all seven trials, a forest plot using the random-effects model showed an odds ratio (OR) of 1.90 (95% confidence interval [CI], 0.77 to 4.66; p=0.1621). However, for subanalysis of three studies that included patients with clinical varicocele and abnormal semen parameters, the fixed-effects pooled OR was significant (OR, 4.15; 95% CI, 2.31 to 7.45; p<0.001), favoring varicocelectomy.
CONCLUSIONS
Varicocelectomy for male subfertility is proven effective in men with clinical varicocele and impaired semen quality. Therefore, surgical repair should be offered as the first-line treatment of clinical varicocele in subfertile men.
Keyword
MeSH Terms
Figure
Reference
-
1. Kass EJ, Reitelman C. Adolescent varicocele. Urol Clin North Am. 1995; 22:151–159.2. Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy: a critical analysis. Urol Clin North Am. 1994; 21:517–529.3. Choi WS, Kim SW. Current issues in varicocele management: a review. World J Mens Health. 2013; 31:12–20.4. Kang DH, Lee JY, Chung JH, Jo JK, Lee SH, Ham WS, et al. Laparoendoscopic single site varicocele ligation: comparison of testicular artery and lymphatic preservation versus complete testicular vessel ligation. J Urol. 2013; 189:243–249.5. Seo JT, Kim KT, Moon MH, Kim WT. The significance of microsurgical varicocelectomy in the treatment of subclinical varicocele. Fertil Steril. 2010; 93:1907–1910.6. Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011; 108:1157–1172.7. Lee HS, Seo JT. Advances in surgical treatment of male infertility. World J Mens Health. 2012; 30:108–113.8. Evers JL, Collins JA, Vandekerckhove P. Surgery or embolisation for varicocele in subfertile men. Cochrane Database Syst Rev. 2001; CD000479.9. Evers JH, Collins J, Clarke J. Surgery or embolisation for varicoceles in subfertile men. Cochrane Database Syst Rev. 2009; CD000479.10. Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012; 10:CD000479.11. Goldstein M. Surgical management of male infertility. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 678–687.12. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.13. Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986; 7:267–275.14. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007; 28:105–114.15. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–1101.16. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.17. Yamamoto M, Hibi H, Hirata Y, Miyake K, Ishigaki T. Effect of varicocelectomy on sperm parameters and pregnancy rate in patients with subclinical varicocele: a randomized prospective controlled study. J Urol. 1996; 155:1636–1638.18. Unal D, Yeni E, Verit A, Karatas OF. Clomiphene citrate versus varicocelectomy in treatment of subclinical varicocele: a prospective randomized study. Int J Urol. 2001; 8:227–230.19. Nilsson S, Edvinsson A, Nilsson B. Improvement of semen and pregnancy rate after ligation and division of the internal spermatic vein: fact or fiction? Br J Urol. 1979; 51:591–596.20. Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. 1995; 63:120–124.21. Grasso M, Lania C, Castelli M, Galli L, Franzoso F, Rigatti P. Low-grade left varicocele in patients over 30 years old:the effect of spermatic vein ligation on fertility. BJU Int. 2000; 85:305–307.22. Dohle GR. Does varicocele repair result in more spontaneous pregnancies? A randomised prospective trial. Int J Androl. 2010; 33:29.23. Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial. Eur Urol. 2011; 59:455–461.24. Marmar JL, Agarwal A, Prabakaran S, Agarwal R, Short RA, Benoff S, et al. Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysis. Fertil Steril. 2007; 88:639–648.25. Evers JL, Collins JA. Surgery or embolisation for varicocele in subfertile men. Cochrane Database Syst Rev. 2004; CD000479.26. Ficarra V, Cerruto MA, Liguori G, Mazzoni G, Minucci S, Tracia A, et al. Treatment of varicocele in subfertile men: the Cochrane review: a contrary opinion. Eur Urol. 2006; 49:258–263.27. Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, Salonia A, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011; 60:796–808.28. Cayan S, Shavakhabov S, Kadioglu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009; 30:33–40.29. Sayfan J, Soffer Y, Orda R. Varicocele treatment: prospective randomized trial of 3 methods. J Urol. 1992; 148:1447–1449.30. Nieschlag E, Behre HM, Schlingheider A, Nashan D, Pohl J, Fischedick AR. Surgical ligation vs. angiographic embolization of the vena spermatica: a prospective randomized study for the treatment of varicocele-related infertility. Andrologia. 1993; 25:233–237.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Varicocelectomy on Male Infertility
- Does Varicocele Repair Improve Conventional Semen Parameters? A Meta-Analytic Study of Before-After Data
- Scrotal Hypothermia in the Infertile Men
- The Changes of Seminal Quality after Varicocelectomy in Adolescence
- Results and Parameters Related to the Improvement of Semen Characteristics after Surgical Repair of Varicocele