J Korean Neurosurg Soc.
2016 Jul;59(4):405-409. 10.3340/jkns.2016.59.4.405.
Experience with 7.0 T MRI in Patients with Supratentorial Meningiomas
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea. paeksh@snu.ac.kr
- 2Department of Neurosurgery, Konkuk University Medical Center, Seoul, Korea.
- 3Neuroscience Research Institute, Gachon University of Medicine and Science, Incheon, Korea.
- 4Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea.
- KMID: 2315978
- DOI: http://doi.org/10.3340/jkns.2016.59.4.405
Abstract
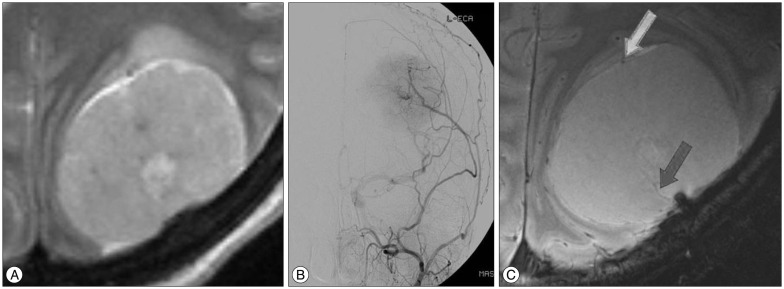
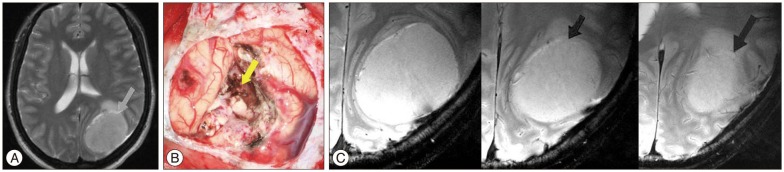
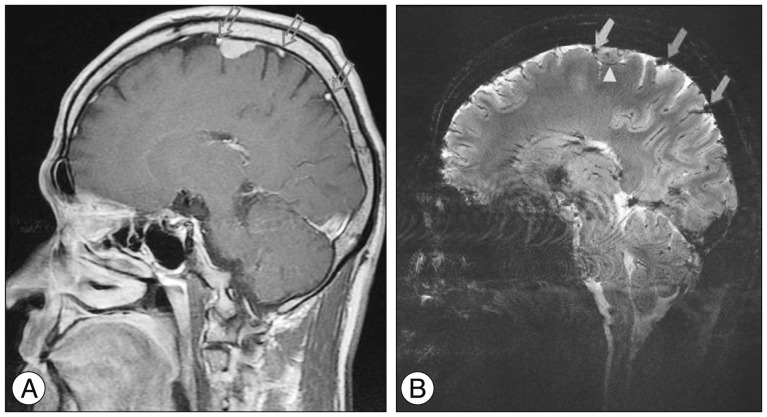
- Meningiomas are typically diagnosed by their characteristic appearance on conventional magnetic resonance imaging (MRI). However, detailed image findings regarding peri- and intra-tumoral anatomical structures, tumor consistency and vascularity are very important in pre-surgical planning and surgical outcomes. At the 7.0 T MRI achieving ultra-high resolution, it could be possible to obtain more useful information in surgical strategy. Four patients who were radiologically diagnosed with intracranial meningioma in 1.5 T MRI underwent a 7.0 T MRI. Three of them underwent surgery afterwards, and one received gamma knife radiosurgery. In our study, the advantages of 7.0 T MRI over 1.5 T MRI were a more detailed depiction of the peri- and intra-tumoral vasculature and a clear delineation of tumor-brain interface. In the safety issues, all patients received 7.0 T MRI without any adverse event. One disadvantage of 7.0 T MRI was the reduced image quality of skull base lesions. 7.0 T MRI in patients with meningiomas could provide useful information in surgical strategy, such as the peri-tumoral vasculature and the tumor-brain interface.
Keyword
Figure
Reference
-
1. Abduljalil AM, Robitaille PM. Macroscopic susceptibility in ultra high field MRI. J Comput Assist Tomogr. 1999; 23:832–841. PMID: 10589555.
Article2. Abduljalil AM, Schmalbrock P, Novak V, Chakeres DW. Enhanced gray and white matter contrast of phase susceptibility-weighted images in ultra-high-field magnetic resonance imaging. J Magn Reson Imaging. 2003; 18:284–290. PMID: 12938122.
Article3. Bitzer M, Wöckel L, Luft AR, Wakhloo AK, Petersen D, Opitz H, et al. The importance of pial blood supply to the development of peritumoral brain edema in meningiomas. J Neurosurg. 1997; 87:368–373. PMID: 9285600.
Article4. Cha S, Johnson G, Wadghiri YZ, Jin O, Babb J, Zagzag D, et al. Dynamic, contrast-enhanced perfusion MRI in mouse gliomas : correlation with histopathology. Magn Reson Med. 2003; 49:848–855. PMID: 12704767.
Article5. Giombini S, Solero CL, Lasio G, Morello G. Immediate and late outcome of operations for Parasagittal and falx meningiomas. Report of 342 cases. Surg Neurol. 1984; 21:427–435. PMID: 6710323.
Article6. Ide M, Jimbo M, Kubo O, Yamamoto M, Imanaga H. Peritumoral brain edema associated with meningioma--histological study of the tumor margin and surrounding brain. Neurol Med Chir (Tokyo). 1992; 32:65–71. PMID: 1376862.7. Kollia K, Maderwald S, Putzki N, Schlamann M, Theysohn JM, Kraff O, et al. First clinical study on ultra-high-field MR imaging in patients with multiple sclerosis : comparison of 1.5T and 7T. AJNR Am J Neuroradiol. 2009; 30:699–702. PMID: 19147714.
Article8. Lupo JM, Banerjee S, Hammond KE, Kelley DA, Xu D, Chang SM, et al. GRAPPA-based susceptibility-weighted imaging of normal volunteers and patients with brain tumor at 7 T. Magn Reson Imaging. 2009; 27:480–488. PMID: 18823730.
Article9. Moenninghoff C, Maderwald S, Theysohn JM, Kraff O, Ladd ME, El Hindy N, et al. Imaging of adult astrocytic brain tumours with 7 T MRI : preliminary results. Eur Radiol. 2010; 20:704–713. PMID: 19763581.
Article